Stage 0 Cancer: A Rare Window of Opportunity That Demands Our Attention
In today’s fast-changing world, the importance of early detection in fighting cancer cannot be overstated. Stories such as Tina Knowles’ personal revelation serve as a powerful reminder of how crucial it is to schedule routine screenings. Even when diagnosed with what is known as stage 0 cancer—a condition that typically appears before cancer invades surrounding tissue—the experience can evoke mixed feelings of relief, anxiety, and uncertainty. This opinion piece takes a closer look at the early detection of stage 0 cancers, the treatment options available, and the emotional rollercoaster patients experience along the way.
Regular screening programs, particularly mammograms, have allowed many to catch these cancers at their earliest and most treatable stages. Yet, the rise in stage 0 diagnoses brings with it tangled issues about overtreatment and the challenge of deciding on the right course of action. In the following sections, we will dig into several key aspects of early cancer detection, share insights on treatment decisions, and underscore why steadfast screening routines remain essential.
Understanding Stage 0 Cancer: Unpacking the Meaning Behind “Carcinoma in Situ”
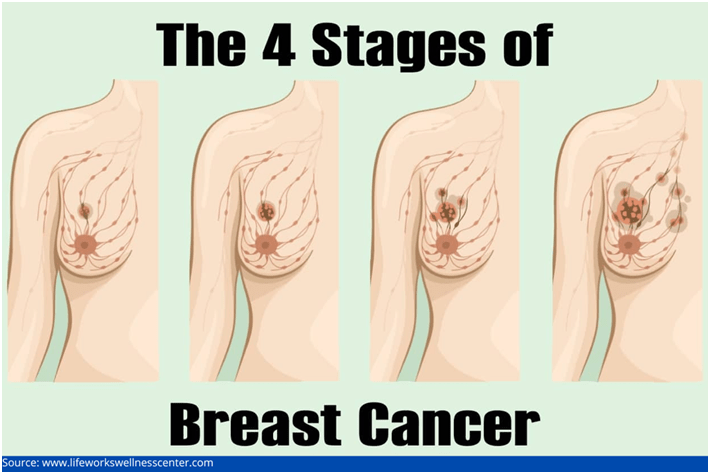
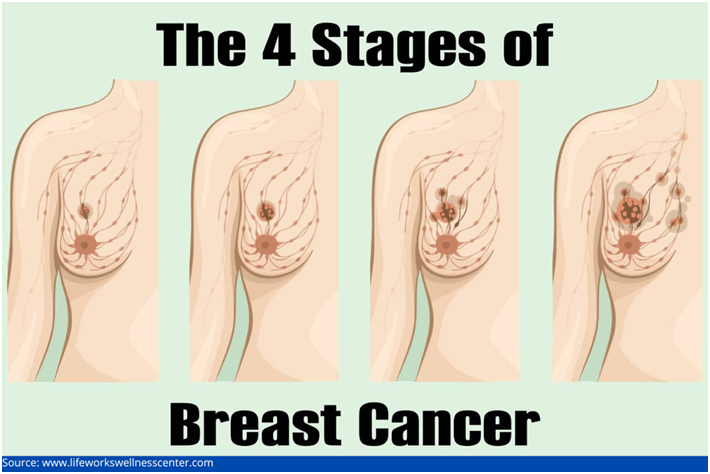
Stage 0 cancer is often referred to as “carcinoma in situ,” a term derived from Latin that means “in its original place.” In this condition, abnormal cells have developed, yet they remain confined to the initial site where they began—without invading surrounding tissues or metastasizing. For example, ductal carcinoma in situ (DCIS) is a well-known form of stage 0 breast cancer where the abnormal cells are limited to the milk ducts.
Because stage 0 cancers typically do not cause symptoms or palpable lumps, they are frequently detected through routine screenings rather than through self-examination or the discovery of a mass. In fact, the effectiveness of screening programs, especially for breast cancer, is a testament to modern medicine’s ability to identify these tricky parts of the disease at a point when they are most treatable.
This early cellular change is not exclusive to breast tissue. Similar non-invasive changes can be found in other organs, such as the cervix (with conditions like cervical intraepithelial neoplasia) or in the colon (in the form of certain types of polyps). The idea is simple: catching these changes in their early phase provides an important window for intervention—before the abnormal cells have the opportunity to progress into harmful, invasive cancers.
Early Detection During the COVID Era: Lessons Learned and Missed Opportunities
The story of Tina Knowles also underscores a pressing issue that many faced during the COVID pandemic: delays in routine health screenings. Many individuals, caught up in the overwhelming concerns of the global crisis, postponed appointments that were once seen as routine. For Knowles, missing a mammogram meant that her cancer might have been discovered even earlier, at stage 0, potentially sparing her from some of the complications associated with later detection.
COVID-19 disrupted regular healthcare practices in many ways. The pandemic introduced nerve-racking circumstances that led to scheduling delays, cancellations, and an overall hesitation to visit medical facilities—even when services were necessary. This experience has prompted a broader discussion about ensuring that even in times of global health crises, the need for regular screenings remains a key priority.
Healthcare providers are now working hard to figure a path through these challenges. They are implementing telehealth appointments, extended clinic hours, and stricter sanitary measures at screening centers. All these actions are super important to make sure that the interruption in routine check-ups does not translate into missed opportunities for early cancer detection.
Treatment Options for Stage 0 Cancer: Weighing Surgery, Radiation, and Active Surveillance
Once stage 0 cancer is detected, patients and their doctors face several treatment choices. The available methods tend to be less aggressive than those used in cases where cancer has invaded neighboring tissues. However, they still require careful, personalized decisions that take into account the patient’s overall health, lifestyle, and personal comfort level.
Surgical options for stage 0 breast cancer, for instance, typically include:
- Lumpectomy: This surgery involves removing only the area affected by abnormal cells, allowing the rest of the breast to remain intact.
- Mastectomy: On certain occasions, a complete removal of the breast is recommended, especially if the abnormal cells appear widespread or if there is a strong family history of breast cancer.
In addition to surgery, radiation therapy is often used after a lumpectomy to help reduce the risk of recurrence. For cancers that have hormone receptors, hormone therapy may also be recommended—this treatment works to lower the future risk of cancer coming back.
More recently, some experts have begun to explore active surveillance as an alternative approach. Active surveillance involves closely monitoring the lesion without rushing into immediate treatment. This approach may be appealing for low-grade lesions in selected patients, while offering options to avoid surgical and radiation side effects. However, active surveillance is still somewhat controversial. The concern remains that without decisive treatment, some cancers might silently progress to a more dangerous state.
Because research indicates that up to 40% of untreated DCIS cases could eventually develop into invasive breast cancer—although the annual risk is relatively low—most doctors currently lean towards early intervention. The key message here is that each treatment option comes with its own set of twists and turns. Patients should work with their healthcare team to weigh the benefits and potential risks of each method, ensuring they make fully informed decisions.
Coping with the Emotional Impact: The Psychological Side of an Early Cancer Diagnosis
An early cancer diagnosis, even one identified as stage 0, often brings heavy emotional challenges. While the statistics may reassure us—stage 0 breast cancer boasts a five-year survival rate nearing 99%—the diagnosis itself can feel like a bundle of nerve-racking emotions. For many individuals, there is a deep sense of relief paired with anxiety, overwhelm, and sometimes even guilt over missed appointments that could have led to even earlier detection.
Patients might experience:
- Fear of the Unknown: Even though the cancer is detected early, uncertainty about its future behavior can be deeply unsettling.
- Regret or Self-Blame: For someone like Tina Knowles, who lamented delaying her screening during the COVID crisis, feelings of regret can add emotional weight.
- Stress from Treatment Decisions: The need to decide between different treatment approaches can cause additional mental strain.
It is important to acknowledge these emotions. Open conversations with healthcare providers, support groups, friends, and family are essential in sorting out the many feelings that arise. A strong support system and clear guidance from medical professionals are absolutely key in helping patients traverse these challenging times.
For many, the journey involves going through a mix of disbelief, fear, and even occasional anger at the circumstances. However, sharing these experiences—as Knowles did—can empower others to prioritize their health and take proactive steps. Establishing a network of support not only eases the emotional burden but also brings to light shared experiences that can be profoundly encouraging.
The Debate on Over-Diagnosis and Over-Treatment: When Is Too Much Too Soon?
The increasing detection of stage 0 cancers has sparked plugged-in discussions among experts over overtreatment. Critics argue that in some instances, aggressively treating stage 0 cancers might lead to unnecessary procedures, given that many of these lesions might never progress to invasive disease. This issue is loaded with problems that hinge on balancing precaution and practicality.
At the heart of this debate lies a couple of tangled issues:
- Risk Assessment: Current medical tools sometimes struggle with predicting which abnormalities in stage 0 will eventually become invasive.
- Emotional and Physical Costs: Surgical procedures, radiation, and even long-term medication regimens are not without side effects and can significantly impact a patient’s quality of life.
- Healthcare Economics: There are also broader considerations regarding the allocation of resources and the psychological burden imposed by over-diagnosing conditions that might remain harmless.
Many experts advocate for a nuanced approach that might include terms like “precancer” or “non-invasive cancer” to better reflect these small distinctions. Clearly, there is a need to figure a path that avoids both the pitfalls of overtreatment and the risks of underestimating a potentially progressing condition.
In a table summarizing the discussion, the benefits and risks might be presented as follows:
| Aspect | Benefits | Risks/Challenges |
|---|---|---|
| Early Detection | High survival rates; possibility to treat before invasion | Psycho-emotional stress; possible overtreatment |
| Surgical Treatment | Definitive removal of abnormal cells | Physical side effects; cosmetic concerns |
| Active Surveillance | Less invasive; avoids unnecessary treatment | Risk of undetected progression; continuous monitoring anxiety |
This debate remains on edge because the scientific community continues to research ways to distinguish between lesions that will stay harmless and those that might pose a real threat. Until such tools become widely available, the consensus among most doctors is to lean towards treatment as a precautionary measure.
Innovations in Early Cancer Screening: Toward More Tailored Care
The remarkable outcomes associated with stage 0 cancer, such as nearly 99% five-year survival rates in breast cancer, highlight the importance of staying on top of our screening routines. Yet, the field of oncology is constantly evolving, and researchers are actively investigating more nuanced methods to determine which detected abnormalities truly require intervention.
Current and emerging strategies include:
- Molecular Profiling: Analyzing the genetic characteristics of cancer cells can help in predicting their behavior, offering clues about whether a specific lesion might progress.
- Advanced Imaging Techniques: Technologies such as digital mammography and 3D tomosynthesis provide more detailed images that aid healthcare professionals in spotting even the subtlest details.
- Biomarker Identification: The search for reliable biomarkers continues, as these could be used to monitor the transformation process of stage 0 lesions.
- Risk Prediction Models: Integrating patient history, genetics, and imaging data helps physicians offer an approach that is as personalized as possible.
These fine points of innovation are expected to make a significant difference in the near future. The goal is simple yet challenging: provide treatment tailored to the patient’s exact needs while avoiding unnecessary procedures that could add to the physical and emotional burdens.
Ongoing research is geared toward refining these methods, ensuring that as soon as a potential threat is identified, it can be accurately classified. Such advancements promise more precise treatment strategies and could potentially mitigate the concerns surrounding over-diagnosis and overtreatment.
Staying on Top of Regular Screenings: Your Best Defense Against Cancer
While medical innovation continues at a breakneck pace, there is no substitute for regular screenings when it comes to early detection. The recent trends only emphasize that proactive health management is super important. Individuals of all ages, especially those with a family history or other risk factors, must make screening appointments a top priority.
Here are some practical steps to ensure you stay on top of your screenings:
- Set Calendar Reminders: Mark your physician’s recommended timeline on your phone or physical calendar so that you never miss a scheduled screening.
- Stay Informed: Keep yourself updated on new screening technologies and guidelines, as medical advice can change with new research.
- Engage in Open Dialogue: Share any concerns or unusual changes with your healthcare provider. Clear communication is essential for early detection.
- Utilize Community Resources: Many communities offer free or low-cost screening programs, so take advantage of these services if available.
Healthcare providers and public health experts are working diligently to ensure that screening programs are accessible and well-communicated, even during times when life seems off-track. The persistent message is that the earlier we catch these abnormal cells, the better our chances of preventing a more invasive progression.
Personal Reflections: Why My Opinion on Early Cancer Detection Has Evolved
As both a commentator and observer of developments in healthcare, I have seen firsthand how early detection transforms patient outcomes. Personal stories, like that of Tina Knowles, remind us that behind every statistic is a human life enriched by personal triumphs and, at times, significant challenges. My view on stage 0 cancer has evolved to embrace not just the clinical benefits of early detection, but also the crucial role of informed patient choices and emotional support during the treatment process.
While there are some confusing bits and twists and turns in how we manage early detections, my conviction remains that routine screenings are a must-have part of modern healthcare. The ability to catch cancer in its earliest possible phase empowers humanity with time—one of our most precious resources—to make informed decisions about our future health.
It is equally important for healthcare professionals to take the time to explain the subtle details of stage 0 detection to their patients. When patients understand what these early findings mean, they can work through their emotions more effectively and determine the best course of action. In turn, this informed approach reduces both the physical and mental stress associated with a cancer diagnosis.
In reflecting on the broader implications, it seems clear that while our understanding of stage 0 cancer continues to improve, it is the combination of cutting-edge technology, patient education, and strong emotional support networks that truly makes a difference. Our healthcare systems should prioritize these aspects, ensuring that each patient is supported from diagnosis to treatment and beyond.
Taking a Closer Look at the Broader Picture: A Call to Action
The multifaceted issues surrounding stage 0 cancer—from diagnosis to treatment and the ensuing emotional rollercoaster—underscore a truth that resonates far beyond the realm of oncology: our health is our most valuable asset. The collective conversation about these early lesions reminds us that proactive care is not a luxury, but a necessity.
Here are some key takeaways that I believe everyone should consider:
- Early detection saves lives: Routine screenings, whether through mammograms, colonoscopies, or other methods, are incredibly effective.
- Informed decision-making is essential: With multiple treatment options available, clear communication between patients and healthcare professionals is super important.
- Emotional support matters: Beyond the clinical aspects, dealing with the emotional burden through counseling and community support can make all the difference.
- Be proactive even in challenging times: Events like the COVID pandemic remind us that our health routines should not be neglected.
These points are not merely medical facts—they represent choices that can dramatically influence the trajectory of a person’s life. For many, failing to prioritize regular screening appointments has led to missed opportunities for early intervention. Then again, a diagnosis in its earliest stage, even if it carries heavy emotions, offers a chance to manage the situation effectively.
Looking Ahead: Embracing a Future of Personalized Healthcare and Early Detection
The future of cancer care is undoubtedly shifting toward personalized medicine—a model where each patient’s treatment is carefully tailored based on their unique health profile. Innovations in molecular profiling, advanced imaging, and biomarker discovery are on the horizon, promising to refine our capacity to distinguish which stage 0 cases require aggressive treatment and which can be safely monitored.
This evolving landscape will likely redefine how we view early detection. In time, the fine shades between benign abnormalities and those that need intervention will become clearer. In the meantime, the current state of knowledge encourages us to adopt a vigilant, proactive stance towards our health.
One can imagine a future where active surveillance is an option for many patients—minimizing unnecessary interventions while ensuring timely treatment when needed. Until that time comes, our focus should remain on regular screening and open, honest communication between patients and healthcare providers. The lessons learned during the recent years, especially during the pandemic, should serve as a catalyst for improved healthcare access and more thoughtful, patient-centered care.
The Role of Community and Policy: Ensuring Accessible Screening for Everyone
Another significant aspect of the conversation revolves around the role of community outreach and public policy in facilitating early detection. Many communities have rallied to offer free or low-cost screening services, and local governments continue to champion public health campaigns that stress the importance of routine check-ups.
Effective public health policies can help steer through the confusing bits of healthcare access by:
- Increasing Awareness: Community programs educate residents on risk factors and the necessity of regular screenings.
- Ensuring Affordability: Subsidized screening initiatives remove financial barriers from routine cancer checks.
- Providing Accessibility: Mobile screening units and extended clinic hours are on the rise, ensuring that even those in remote areas have access to vital services.
The collaboration between healthcare providers, local governments, and community organizations is essential to make early detection a reality for all. By focusing on these connected efforts, we can ensure that everyone, regardless of their background or geographic location, benefits from the lifesaving potential of early cancer detection.
Conclusion: Empowering Patients to Act Before It’s Too Late
In wrapping up, the discussion around stage 0 cancer is a powerful call to action for both the public and healthcare practitioners. The experience shared by Tina Knowles is not just a celebrity headline—it is a testament to the need for vigilance, prompt action, and a solid support network when it comes to our health.
While the treatment options for stage 0 cancer are generally less invasive, the decisions that follow a diagnosis are loaded with implications, both physical and emotional. The benefits of early detection are crystal clear: higher survival rates, a broader range of treatment options, and the hope of intervening before cancer becomes invasive.
This opinion editorial reinforces the point that staying disciplined with your regular health screenings is not something to put off, even in the face of nerve-racking global events like a pandemic. Regular check-ups are not just preventive measures—they are opportunities to catch potential issues before they develop into complicated pieces that require more aggressive treatments.
Ultimately, each of us is responsible for our own health. By ensuring that we schedule and attend our routine screenings, we enable our healthcare providers to detect any abnormalities early on. That early detection might just be the difference between navigating a smooth path to recovery or encountering a cascade of more complicated issues later in life.
Take the time to review your screening schedule, and if you have postponed an appointment—even during a busy or challenging time—make it a priority to get back on track. Whether you are facing your first screening or revisiting your routine follow-ups, remember that the early detection of stage 0 cancers is one of the most effective means to safeguard your future health.
As we look forward to advances in personalized healthcare and more refined diagnostic tools, let’s not lose sight of one key principle: early detection is essential. When you reschedule that appointment today, you are taking the first step toward a healthier tomorrow—a step that could very well save your life.
Originally Post From https://theconversation.com/stage-0-cancer-is-often-overlooked-but-it-could-be-your-earliest-warning-sign-255460
Read more about this topic at
Early Detection Saves Lives Coalition
Early Detection Saves Lives: The Essential Cancer …