Immune Checkpoint Inhibitor Therapy and Kidney Cancer: An Evolving Frontier
The landscape of kidney cancer treatment is changing fast, and one approach that has been stirring discussion is the integration of surgery with immune checkpoint inhibitor (ICI) therapy. In recent times, the medical community has been taking a closer look at the procedure known as cytoreductive nephrectomy—surgical removal of a kidney tumor that has spread beyond its original site—in patients with metastatic renal cell carcinoma. This investigative move aims to figure a path towards not only prolonging survival but also improving quality of life, especially for those facing the overwhelming challenges posed by advanced kidney cancer.
In an era when personalized treatment plans are essential, the SWOG S1931 (PROBE) study has provided much-needed insight into the benefits and possible drawbacks of supplementing ICI therapy with surgery. The many twisted and tangled issues surrounding the treatment options require clinicians, patients, and caregivers to work through confusing bits and complicated pieces of information in order to decide on the best course of action.
Understanding Cytoreductive Nephrectomy in Metastatic Kidney Cancer
Cytoreductive nephrectomy involves removing a kidney tumor in order to reduce the overall tumor burden in the body. According to the Kidney Cancer Association, this surgery has emerged as one of the best options to extend the lives of patients with metastatic renal cancer. However, like any surgical procedure, it comes with its own set of intimidating and nerve-racking concerns.
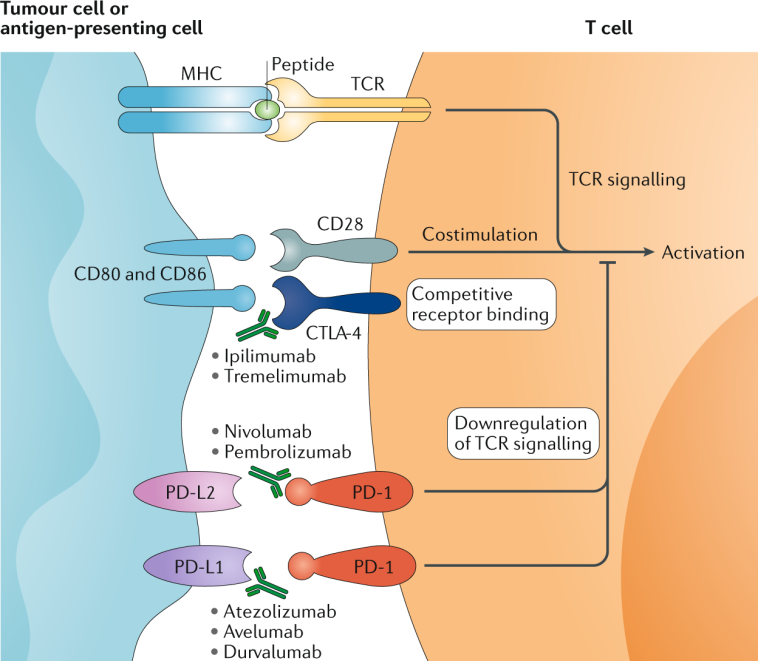
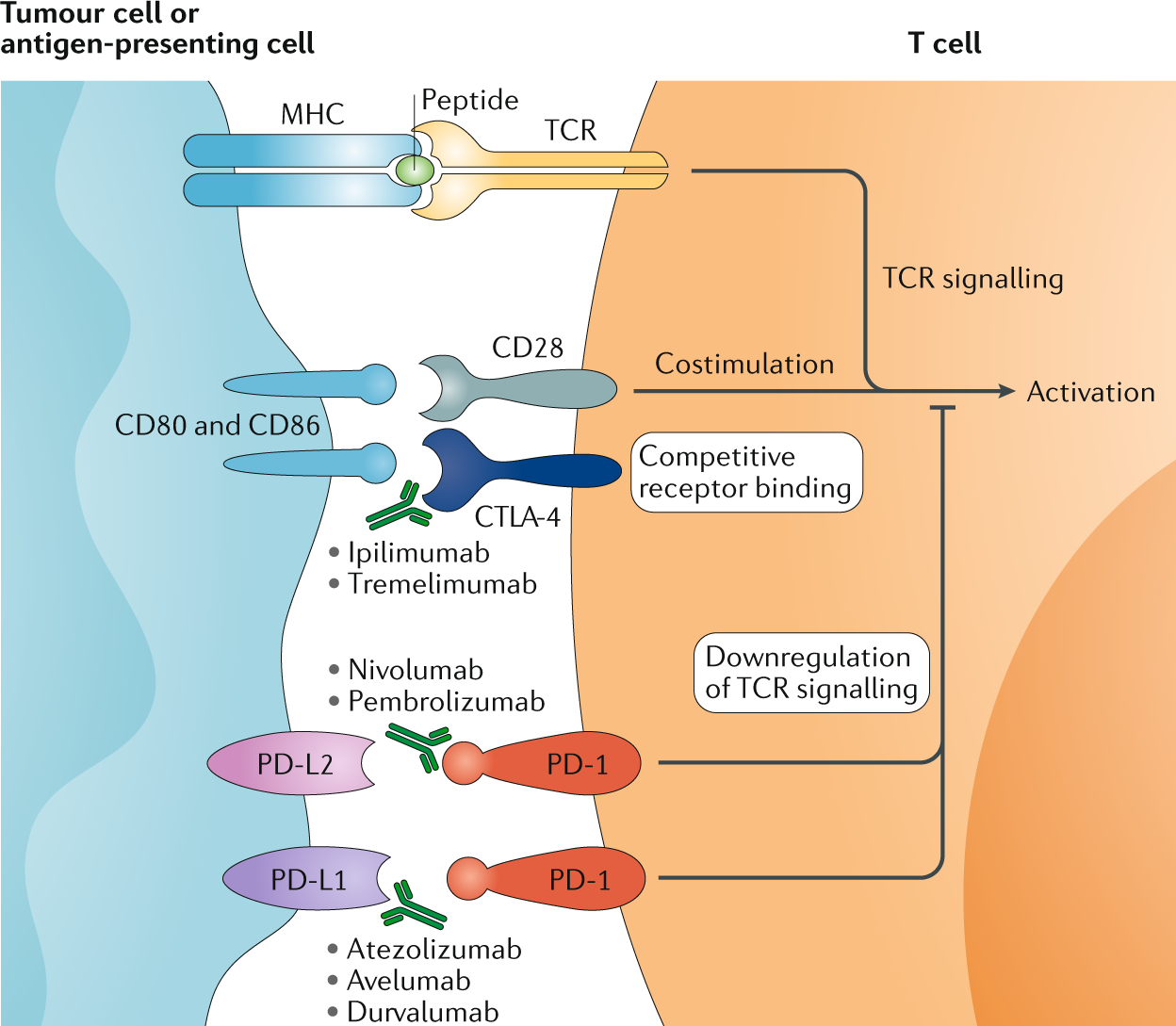
What makes the procedure particularly noteworthy is not just the act of removing the tumor, but its potential to work in tandem with immune therapies. The idea is that by removing a large tumor mass, the body’s immune system—already activated by ICI therapy—can work more effectively to target any remaining cancer cells. Despite the promising concept, the medical community acknowledges that there are many fine points and subtle parts to consider before broadly recommending this combined approach.
The SWOG S1931 Study: Key Findings and Patient Impact
At the heart of recent debates is the SWOG S1931 (PROBE) study, a phase 3 randomized trial designed to evaluate the survival benefits of adding cytoreductive nephrectomy to a combination treatment regimen based on immune checkpoint inhibitors. In this trial, patients with advanced kidney cancer were first given ICI therapy for around three months. Those who exhibited a stable disease status or achieved a partial response were then split into two groups: one group went on to have surgery, while the other group continued with non-surgical management.
This design allowed researchers to compare overall survival outcomes and quality of life data between the two cohorts. Observers in the field have been keen to get into the nitty-gritty of the findings, exploring both the fine details of the surgery’s effect and the subtle differences in patient outcomes after receiving a combination therapy approach.
Despite the encouraging results presented, there remain several challenging parts that need addressing. Doctors must fill in the dots regarding who benefits most from the addition of surgery. As the trial progressed, patients and clinicians alike had to work through a mix of practical challenges, including the timing of surgery relative to the immunotherapy regimen, the patient’s general health status, and the potential for unexpected complications during and after the surgery. Each of these issues brings its own twists and turns to the overall treatment strategy.
Benefits Beyond Survival: Quality of Life Improvements
While extending survival is a key goal in cancer treatment, many experts argue that a comprehensive approach should also prioritize patients’ quality of life. In the context of the SWOG S1931 trial, researchers explored whether adding cytoreductive nephrectomy to ICI therapy could yield improvements that went beyond simple survival statistics. For individuals dealing with not only the physical but also the psychological toll of advanced kidney cancer, every little improvement counts.
Some of the essential advantages observed in patients who underwent surgery include:
- Increased Response to Treatment: By removing the largest tumor mass, the immune system might be better equipped to target residual cancer cells on a micro level.
- Potential Reduction in Symptoms: Patients sometimes experience improvements in pain management and overall discomfort when the tumor burden is reduced.
- Enhanced Engagement in Daily Life: There are accounts suggesting patients return to normal activities sooner, reporting improvements in energy levels and overall well-being.
Even though these potential benefits sound promising, it is important to remember that the effects can be quite individual. The trial outcomes indicate that for some patients, the addition of surgery may open up a clear, direct path toward an improved quality of life, while for others, the risks might outweigh the advantages. This complexity reinforces the need for personalized treatment plans and informed discussions between physicians and patients.
Examining the Tricky Parts and Tangled Issues in Treatment Selection
The decision to add cytoreductive nephrectomy to ICI therapy is packed with many tricky parts. One must account for the patient’s specific condition, the stage of the disease, and the response to initial ICI treatment. For many patients facing metastatic kidney cancer, the idea of undergoing surgery might seem overwhelming. Many are understandably anxious—the prospect of surgery combined with the side effects of immunotherapy introduces several nerve-racking and off-putting procedures.
Here are a few of the complicated pieces that medical professionals need to consider:
- Patient Selection: Not all patients are suitable candidates for surgery. Often, doctors need to carefully evaluate the overall health of the patient and the extent of the tumor’s spread.
- Timing of Surgical Intervention: The decision to perform surgery after approximately three months of ICI therapy is based on the patient’s initial response; however, determining this exact timing requires a detailed analysis of many small distinctions in clinical status.
- Managing Post-Surgical Recovery: Postoperative care is critical, and a well-structured plan must be in place to navigate the intense recovery period that follows a major surgery.
- Balancing Risks and Rewards: The addition of surgery carries potential side effects and complications which necessitate clear, balanced communication with patients about what they might expect.
For many facing the prospect of combined therapy, making your way through these confusing bits may seem a bit like traversing a labyrinth. In order to decide whether this treatment route is best, patients and professionals must engage in detailed discussions where every twist and turn is explored. The challenge isn’t simply in reducing tumor mass—it’s in finding the right equilibrium that aligns medical insights with patient goals.
Quality Evidence Meets Real-World Experiences: The Patient Perspective
In discussions about advanced kidney cancer therapy, the patient’s voice is one that cannot be overlooked. It’s clear that while clinical trial data provide essential numbers and percentages regarding survival rates and response levels, everyday experiences often provide deeper insight into what works in practice.
Patients who have gone through the combined treatment approach have reported a mix of outcomes. Some have expressed relief at the prospect of actively fighting back against cancer by removing the primary tumor, while others have struggled with the nerve-racking side effects of surgery combined with the ongoing demands of systemic immunotherapy. In many cases, the improvement in symptoms after surgery has been a key element in regaining a sense of control over life.
It is super important to remember that the decision to take on such an aggressive treatment plan is highly personal. Many patients weigh the potential gains in survival and well-being against the possibility of complications. To aid in this decision-making process, doctors often encourage patients to consider factors such as lifestyle, overall health, and support systems. The shared decision-making model has become a cornerstone in modern healthcare, ensuring that both the science and the distinct personal circumstances come together to form a treatment plan that is just right for the patient.
Clinical Trials: How They Shape Future Treatment Directions
The SWOG S1931 trial is an example of how modern clinical trials are instrumental in guiding treatment strategies. By testing the addition of cytoreductive nephrectomy to ICI therapy in a controlled, randomized study, researchers have managed to dig into the subtle details of how such combined approaches can be harmonized to offer the best patient outcomes.
Clinical trials like this one are loaded with both promise and challenges. On one hand, they pave the way for new treatment pathways that can potentially improve survival and quality of life. On the other, they also highlight the many fine shades of decision-making required when integrating multiple therapies. This on-edge balancing act has led to several important revelations:
- Refined Patient Stratification: With clear criteria and well-defined patient groups, trials help in identifying which individuals are most likely to benefit from surgery in addition to immunotherapy.
- Adapting Treatment Timelines: Data from the study help flesh out the optimal treatment sequence—when to start with ICI therapy and the best time to consider surgery.
- Understanding Treatment Tolerability: Both clinicians and patients gain insights into the potential side effects and recovery trajectory so that they can plan accordingly.
These findings do not only stimulate academic discussion; they have real-world implications. For many practitioners, the evidence presented opens up a discussion on the best ways to work through the tangled issues of metastatic kidney cancer treatment. As additional data emerge from long-term follow-up studies, the hope is that more refined treatment protocols will be developed. For patients and clinicians alike, this is a promising direction, though it does mean that there will continue to be a need for careful, personalized decision-making.
Combining Surgery with Immunotherapy: Weighing the Evidence
The idea of combining cytoreductive nephrectomy and immunotherapy is both innovative and, at times, nerve-racking. With each new study comes a mix of good news and also questions that remain to be answered. Advocates of the combined approach point to the theoretical advantage of reducing tumor load to allow immunotherapy to work unimpeded. Skeptics, however, note that surgery is not without its risks and that in many cases, the benefits might be marginal when measured against the potential for complications.
Some of the critical points that emerge when evaluating this combination include:
- Effectiveness in Tumor Reduction: The combination may help in lowering the overall tumor burden, thereby creating a more favorable environment for the immunotherapy to work.
- Potential for Long-Term Survival Gains: Early data suggest that some patients might experience improved overall survival, though the evidence is still evolving.
- Improved Quality Metrics: Many patients report an enhanced quality of life, especially when surgery successfully alleviates symptoms that were previously hard to manage.
- Risk Management: Surgeons must be cautious, as the balancing act between potential benefits and unwanted side effects is full of problems that require attention at every step.
When patients and their families are confronted with the overwhelming task of deciding on a treatment plan, these points help to picture the entire scenario. They highlight the need for clear, honest discussions wherein both the potential rewards and the complicated pieces—the confusing bits of timing, expected recovery, and overall outcome—are brought to light. For doctors, it is a matter of presenting the patient with all the necessary information so that they can figure a path that best suits their needs.
Real-World Decision Making: Patient-Centered Care in Action
The decision to integrate surgery with ICI therapy is not simply about reading through numbers in a clinical trial. Instead, it’s about considering the whole person—each patient’s medical history, personal preferences, and the support systems they have in place. In practice, many patients find themselves in a situation where choices are not clear-cut. Instead, they must pick through a jumble of conflicting data, personal fears, and a myriad of medical opinions.
For many, the process might look something like this:
| Step | Considerations |
|---|---|
| Initial Diagnosis | Understanding the extent of the tumor spread and available treatment options. |
| Treatment Discussion | Reviewing the benefits and side effects of ICI therapy along with possible surgical intervention. |
| Clinical Trial Eligibility | Determining if the patient qualifies for trials like SWOG S1931, which may offer additional options. |
| Informed Decision Making | Discussing with family, friends, and healthcare providers to weigh the potential risks against the rewards. |
| Post-Treatment Management | Planning the recovery process and managing ongoing therapeutic needs. |
This table provides a snapshot of the many stages during which patients and healthcare providers must dig into the small distinctions and subtle details to craft the best treatment plan. For many patients, each of these steps can be as intimidating as it is critical, and the ability to discuss and figure out each twist and turn with their medical team cannot be overstated.
Future Directions: Where Do We Go from Here?
As promising as the combined approach of cytoreductive nephrectomy and ICI therapy might be, the next steps require careful refinement and further study. One crucial hurdle remains: standardizing the treatment strategy so that it yields consistent, reproducible results across varied patient populations. Researchers and clinicians alike are faced with several off-putting challenges as they work through the remaining questions, including:
- Refinement of Patient Selection Criteria:
- Which patients are most likely to benefit from the addition of surgery?
- How can we account for differences in overall health and tumor biology?
- Optimizing Treatment Timelines:
- Determining the precise moment when surgery can have the maximum benefit.
- Adjusting immunotherapy timing based on individual responses.
- Managing Complications and Recovery:
- What best practices can be developed to minimize post-operative complications?
- How can supportive care be enhanced to ensure a smooth recovery?
These assessments represent more than just the next chapter in clinical research; they are essential steps in figuring out a path that can transform how advanced kidney cancer is treated. The future promises further trials, longer follow-up periods, and hopefully, treatment algorithms that combine the best of both surgical and immunotherapy approaches.
Balancing Risks and Rewards: A Personal Reflection
From a personal perspective, the addition of cytoreductive nephrectomy to ICI therapy represents both promise and a series of complicated pieces that need to be managed. For patients facing metastatic kidney cancer, the option of having the primary tumor surgically removed is often seen as a proactive step. However, each individual must weigh the potential life-extending benefits against the intimidating risks of surgery.
It is critical to remain neutral and consider all aspects of the treatment, including:
- The immediate side effects: The recovery period after surgery can be nerve-racking and may involve strong post-operative discomfort.
- Potential long-term benefits: For many, even small improvements in symptoms can be seen as a win.
- Emotional and psychological impacts: The decision-making process is full of problems, and no two patient journeys are identical.
Patients and healthcare providers must work together to sift through the confusing bits and find a path forward that balances the need for aggressive treatment with the overarching goal of maintaining or improving quality of life. This collaboration is one of the cornerstones of patient-centered care, ensuring that every decision is discussed in detail and in a language that everyone can understand—be it the doctor, the patient, or the family members involved in the care plan.
Synthesizing Research and Real-World Insights
Modern medicine is increasingly focused on synthesizing high-quality research with real-world insights. In the case of combining cytoreductive nephrectomy with immune checkpoint inhibitor therapy, both clinical data and patient experiences are shaping a treatment approach that is pragmatic and patient-focused.
Here are a few super important points that encapsulate the current sentiment in the medical community:
- Data-Driven Decisions: Clinical trial results provide a foundation that informs treatment protocols, with survival statistics and quality of life measurements guiding practice.
- Individualized Treatment: While the overall statistics are promising, the success of treatment hinges on tailoring therapy to the fine shades of each patient’s condition.
- Continuous Research: Ongoing studies and follow-up data will help refine treatment timelines, risk assessment, and patient selection criteria.
- Collaboration Between Specialties: Urologists, oncologists, and surgical specialists must all steer through a category of responsibilities, offering balanced advice informed by both science and the human experience.
As we continue to gather more data and as the medical community’s understanding evolves, it is crucial to keep an open mind and recognize that the combination of surgery with immunotherapy might not be a one-size-fits-all solution. Instead, it should be viewed as another tool in a multifaceted treatment toolbox, one that—when used correctly—can make a significant difference in the lives of patients.
Reflections on the Integration of Surgery and Immunotherapy
It is clear that the addition of cytoreductive nephrectomy to ICI therapy in kidney cancer treatment is reshaping how both patients and practitioners think about cancer care. When traditional methods meet modern immunotherapy, the resulting treatment strategy is full of potential, yet it is also loaded with problems that require careful deliberation. The integration of these two approaches forces us to get into the nitty-gritty of combining physically invasive procedures with systemic therapies designed to harness the body’s natural defenses.
This journey is not without its nerve-racking elements. For those who have to decide whether to undergo the surgery, the process can seem as if it’s between a rock and a hard place. The decision-making process involves not only learning the small distinctions between treatment options but also managing the emotional roller coaster that comes with facing a life-threatening disease.
Nevertheless, the promise embedded in the clinical trial data is too significant to ignore. Both improved survival rates and the potential for enhanced quality of life provide a compelling case for continued research and, eventually, broader adoption of a combined treatment approach. As the evidence base grows, we may see more refined and patient-specific guidelines that help steer through these tricky parts with greater confidence.
Looking Ahead: The Future of Kidney Cancer Treatment
Looking ahead, the integration of cytoreductive nephrectomy with immune checkpoint inhibitors appears to be a promising avenue for transforming the treatment of metastatic kidney cancer. The research community is now tasked with overcoming many of the complicated pieces and confusing bits that still plague our current treatment protocols. Several areas will likely see major benefits as further studies are conducted:
- Enhanced Predictive Models: New tools like advanced imaging techniques and molecular biomarkers may soon help identify which patients will benefit most from surgical intervention after immunotherapy.
- Tailored Treatment Algorithms: By combining clinical insight with patient-specific data, future treatment protocols could be even more personalized, offering a step-by-step guide that minimizes risk while acknowledging the unique circumstances of each patient.
- Holistic Care Approaches: The future of kidney cancer treatment will likely integrate not only advanced medical therapies but also supportive care measures that address the psychological and emotional challenges of dealing with cancer.
- Long-Term Follow-Up and Survivorship Studies: Understanding the long haul effects of this combination therapy will be a key area of interest, ensuring that patients not only live longer but live better.
As healthcare providers work to untangle the remaining twists and turns of this combined approach, the ultimate goal remains clear: to provide patients with a treatment plan that is both effective and considerate of the overall human experience. In doing so, the blending of surgery with immune checkpoint blockade symbolizes the exciting progress that modern medicine is capable of achieving when research and compassionate care come together.
Conclusion: Charting a Balanced Course in Advanced Kidney Cancer Care
The integration of cytoreductive nephrectomy with immune checkpoint inhibitor therapy represents a dynamic and evolving frontier in the treatment of metastatic kidney cancer. As we stand at the intersection of surgical innovation and advanced immunotherapy, patients and clinicians are engaged in a joint effort to work through the myriad of tricky parts, tangled issues, and subtle details that define the modern battle against cancer.
From the initial diagnosis to the painstaking process of clinical trial development, and ultimately to the personal decision-making journey of each patient, the picture that emerges is one of hope tempered by realism. It is a picture that acknowledges the nerve-racking nature of combining treatments, yet remains optimistic about the potential benefits for survival and quality of life.
The SWOG S1931 trial, along with similar studies, is not simply a collection of data points—it is a reflection of the many lives touched by kidney cancer and the collective effort of the medical community to guide patients safely through the maze of treatment choices. Every study, every patient story, and every challenging decision add up to a broader understanding that will ultimately lead to more effective, personalized care for patients facing metastatic kidney cancer.
As we move forward, it is essential that both research and clinical practice remain flexible, adaptive, and deeply connected to the real-world experiences of patients. For the individuals who are confronted with the daunting prospect of a cancer diagnosis, having a tailored treatment plan that considers both the scientific evidence and the human elements of care can make the difference between feeling overwhelmed and feeling empowered.
In summary, while combining surgery with immune checkpoint therapy is still a subject under careful scrutiny, its promise offers a window into the future of kidney cancer management—one where every patient’s journey is respected and where treatment decisions are guided by both hard evidence and the deeper, personal quest for quality living. The path is far from straightforward, but with continued research, thoughtful discussion, and a commitment to patient-centered care, the future holds hope for improved outcomes in this challenging area of oncology.
Ultimately, the integration of cytoreductive nephrectomy with ICI therapy demands that we all—researchers, clinicians, patients, and families alike—come together to find our way through the confusing bits and complicated pieces of advanced cancer care. By embracing the lessons learned from clinical trials and the invaluable feedback from those who live with the disease, we can work towards treatment approaches that not only extend life but also enhance its quality. This is the promise of modern medicine: a commitment to balance scientific breakthroughs with the everyday realities of those on the cancer journey.
Originally Post From https://www.curetoday.com/view/investigating-the-addition-of-surgery-to-ici-therapy-in-kidney-cancer
Read more about this topic at
Immunotherapy Could Replace Surgery, Enabling Patients …
How Immunotherapy Before Surgery Can Impact Patient …