Digital Pathology: A New Frontier in Rural Cancer Diagnosis
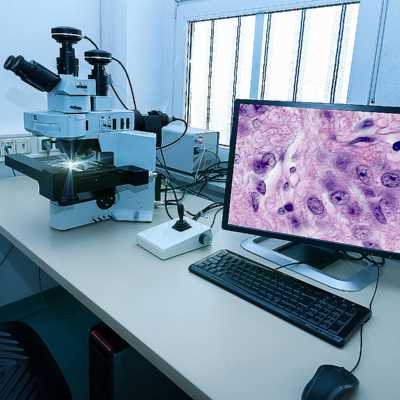
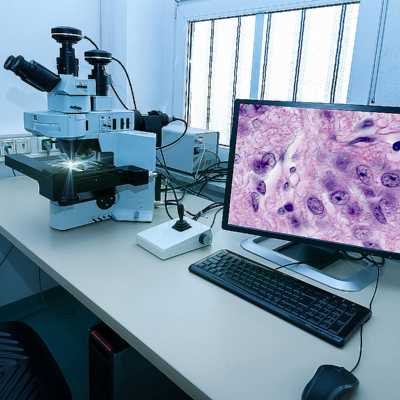
The way we diagnose and treat cancer is experiencing a transformative change, especially for patients living in rural areas. Digital pathology, an emerging field that shifts from traditional glass slide microscopy to high-resolution digital imaging, is making it easier than ever for expert pathologists to review tissue samples remotely. This advancing technology not only cuts down on the nerve-racking wait times for diagnosis but promises more precise and timely treatment options regardless of where a patient lives.
In rural communities, where access to specialized medical services is often limited, digital pathology is proving to be a game-changing tool. By converting physical slides into digital images that can be reviewed on computers across great distances, healthcare providers are now able to extend their reach far beyond urban centers. This advancement helps untangle the confusing bits of remote diagnosis and brings expert opinions directly to areas that have long struggled with limited access to medical specialists.
Improving Cancer Diagnosis with Remote Digital Imaging
Digital pathology creates an ecosystem where expert insights can be shared quickly and effectively. Instead of waiting for tissue samples to be physically transferred between facilities—a process often riddled with delays—digital images allow for almost real-time consultations. Physicians in rural hospitals can now get a second opinion from top-tier specialists without the intimidating need for long-distance travel.
This rapid turnaround not only expedites the diagnostic process but also enhances the accuracy of the diagnosis. Studies have shown that approximately 10% of initial diagnoses may be corrected upon review by experts at specialized centers. These improved assessments are crucial in developing optimal treatment plans and ensuring that patients receive the best care possible.
High-Resolution Imaging and Cloud-Based Storage Solutions
One of the key drivers behind digital pathology is the availability of high-resolution scanning devices. These advanced tools capture fine details of tissue samples that might be lost in traditional microscopy. Once these images are digitized, sophisticated cloud-based storage solutions ensure that they are accessible to physicians everywhere. This technology bridges the geographical gaps that have long been a tangled issue in cancer care.
Moreover, with cloud-based systems, these digital slides are easily shared and can be stored securely, ensuring compliance with privacy regulations. This accessibility not only improves workflow efficiency but also makes it easier for rural healthcare providers to get essential opinions, making the process less overwhelming and more collaborative.
Artificial Intelligence as a Supportive Diagnostic Tool
Alongside advanced imaging and digital storage, artificial intelligence (AI) plays a supportive role in the digital pathology workflow. Although nothing can replace the keen judgment of a highly trained, board-certified pathologist, AI algorithms serve as a useful second pair of eyes. These systems help highlight areas of concern on digital slides, ensuring that no subtle detail goes unnoticed.
AI can sift through a multitude of images rapidly, flagging cases that might require more nuanced attention. This is particularly useful for rural settings where a limited number of specialists might be available to interpret every case. By automating parts of the review process, AI reduces the risk of missing critical markers in tissue samples, thus serving as a practical aid to human expertise.
Addressing the Tricky Parts of Rural Cancer Care
For many rural communities, simply accessing advanced cancer care has been a nerve-racking challenge. Patients often face long travel times, financial burdens, and logistical hurdles that can delay diagnosis and treatment. Digital pathology is stepping in to help solve these tricky parts by reducing the dependency on physical transportation of samples and enabling remote consultation.
The technology simplifies what was once a complicated process. Instead of navigating confusing bits of scheduling and delayed lab reports, healthcare providers can now use digital platforms to quickly connect with top-tier experts. This removes some of the twists and turns associated with traditional pathology while offering renewed hope for patients in underserved regions.
Expert Collaboration: Solving the Tangled Issues of Diagnosis
One of the most exciting aspects of digital pathology is its ability to foster real-time collaboration among experts. Traditionally, when a rural hospital encountered a challenging case, local physicians might have to wait days or even weeks for a specialist’s input. Now, with digital images transmitted securely over the internet, expert centers can provide their feedback much more rapidly and reliably.
This collaborative approach is not just limited to diagnosing cancer. It can extend into treatment planning, where multiple specialists from different fields participate in a tumor board discussion. By working together on digital platforms, they can share insights, deliberate on treatment options, and decide on the best course of action. This collective effort helps untangle the complicated pieces of cancer care, ensuring that every decision is as informed as possible.
Steps Toward Effective Remote Collaboration
- Digital Communication Channels: Secure platforms that allow for the sharing of digital slides and patient data in real-time.
- Interdisciplinary Meetings: Regular virtual tumor board meetings facilitate the sharing of ideas and quick decision-making.
- Continuous Professional Development: Training programs and webinars help keep rural healthcare providers updated on the latest digital pathology advancements.
- Integrated Reporting Systems: Combining data from various departments ensures comprehensive reviews and accurate diagnoses.
These initiatives are like small, essential building blocks in improving overall cancer care. By using such methods, the healthcare community is better equipped to work through the subtle parts of diagnosing and treating cancer in remote locations.
Real-World Impact: A Closer Look at Enhanced Patient Outcomes
One of the most striking benefits of digital pathology is its impact on patient outcomes. With quicker and more precise diagnoses, treatment can begin earlier—an often critical factor in many cancer cases. In rural settings, where delays can sometimes be more nerve-racking than the diagnosis itself, a faster turnaround is key.
Let’s break down some of the real-world benefits:
- Faster Diagnosis: Digital pathology reduces waiting times, which means patients can begin treatment sooner.
- Improved Accuracy: With expert reviews, the chances of diagnostic error are minimized. This leads to more effective treatment plans and better health outcomes.
- Reduced Travel Burdens: By providing remote consultations, digital pathology eliminates the need for patients to travel long distances to specialist centers. This is particularly crucial in rural areas where transportation can be a significant barrier.
- Enhanced Patient Confidence: Knowing that their case is being reviewed by multiple experts helps build trust and reduces the anxiety often associated with cancer diagnosis.
Such improvements not only make the overall process less overwhelming for patients but also support healthcare providers in delivering more timely and effective care. The small distinctions between traditional and digital pathology methodologies end up making a big difference in the lives of those affected by cancer.
Success Stories from the Field
A number of success stories highlight the transformative effect of digital pathology in rural cancer care. In several case studies, patients who initially faced the risk of misdiagnosis received a second review that corrected up to 10% of initial interpretations. With these corrections, doctors were able to tailor more effective treatment strategies that substantially improved survival rates.
These accounts underscore the urgent need for broader adoption of digital pathology technology. They also serve as a reminder that when healthcare systems work through the tricky parts with modern solutions, the results can be life-changing for patients, and these improvements ripple out into the wider community.
Overcoming the Overwhelming Barriers in Rural Healthcare
Despite the many advantages of digital pathology, there are still a number of challenges that remain when it comes to implementation in rural areas. Staff training, technology costs, and ensuring reliable internet connectivity are just a few of the head-spinning factors that may initially seem off-putting or overwhelming.
However, by taking a closer look at these issues, we can identify strategic ways to mitigate them. For example, investing in comprehensive training programs can help local healthcare providers understand and effectively utilize digital pathology tools. Financial support and incentives—whether through public funding or private philanthropy—can also relieve some of the financial burdens linked to technology upgrades.
Many of these challenges are simply the result of navigating a new terrain. With careful planning and collaboration between government bodies, private entities, and the healthcare community, it is possible to figure a path that overcomes these obstacles. The goal is to ensure that every patient, regardless of their location, has access to top-quality cancer care.
Key Challenges and Practical Solutions
| Challenge | Practical Solution |
|---|---|
| Limited Access to Technology | Government grants and private partnerships to fund digital equipment |
| Training Needs | Develop targeted education programs and continuous professional development courses |
| Connectivity Issues | Invest in reliable broadband infrastructure in rural areas |
| Data Security | Implement robust encryption and security protocols for patient data |
By carefully addressing these key challenges, the healthcare sector can ease some of the intimidating twists and turns that can slow technological progress. Each step forward is another opportunity to deliver better care to those who need it most.
Integrating Telemedicine for a Broader Impact
Telemedicine is another promising avenue that complements digital pathology perfectly. By connecting rural healthcare providers with leading specialists through telecommunication tools, telemedicine extends the reach of expert opinions even further. This remote connectivity has proved indispensable for providing timely consultations, especially when every minute counts.
With telemedicine, patients no longer need to endure nerve-racking long-distance travel. Instead, virtual evaluations can be arranged quickly, allowing both patients and doctors to focus on immediate treatment needs. Furthermore, this approach can help train local physicians by allowing them to observe remote experts as they work through subtle details in difficult cases.
Benefits of Telemedicine in Rural Cancer Care
- Real-Time Consultations: Direct communication between rural doctors and specialists can lead to immediate clarification and quicker decisions on patient care.
- Enhanced Learning Opportunities: Telemedicine platforms offer educational sessions and virtual mentoring, enabling local doctors to upskill more rapidly.
- Reduction in Patient Stress: Avoiding long journeys to urban centers minimizes the physical and emotional strain on patients already dealing with a serious diagnosis.
- Cost-Effective Solutions: Both patients and healthcare facilities can save time and resources through virtual consultations.
When combined with digital pathology, telemedicine creates a comprehensive healthcare network that is both responsive and flexible. This dynamic duo is steadily chipping away at the barriers that have long hindered high-quality cancer care in rural settings.
Policy Implications and Future Trends in Digital Pathology
The increasing integration of digital pathology into mainstream cancer care also calls for supportive policies and regulatory frameworks. Governments and healthcare organizations must work together to establish guidelines that maintain high standards of care while encouraging innovation. This is especially critical in rural settings, where existing disparities can be further widened if not addressed by thoughtful policy decisions.
Policymakers need to consider several key factors:
- Funding and Reimbursement: Creating sustainable funding models to support the adoption of digital pathology tools in rural hospitals.
- Data Privacy and Security: Ensuring that digital images and patient data are handled with the utmost care and protected by stringent security protocols.
- Interoperability: Promoting systems that can seamlessly share data between various healthcare providers, ensuring smooth collaboration.
- Training Standards: Supporting standardized training programs so that rural healthcare professionals can confidently use digital tools.
The future trends in digital pathology seem encouraging. With continuous improvements in high-resolution imaging, AI algorithms, and data management, the technology is bound to become even more accessible and sophisticated. As these innovations mature, they will further demystify the complicated pieces of cancer diagnosis, ensuring that every patient—no matter how remote their location—is offered the most up-to-date care available.
Emerging Technologies and Their Impact
Looking ahead, emerging technologies such as augmented reality (AR) and enhanced machine learning models are poised to add extra layers of support to digital pathology. For instance, AR can help overlay critical data on digital slides during consultations, providing visual cues that can make the fine points of tissue analysis clearer to all involved. Additionally, improved machine learning tools will continue to hone in on the slight differences and small distinctions in tissue samples, ensuring that potential issues are flagged sooner rather than later.
These cutting-edge technologies empower pathologists to work through the tricky parts of diagnosis with even greater efficiency and certainty. When combined with robust telemedicine frameworks and supportive policies, the future of digital pathology is not just promising—it is essential for leveling the playing field in cancer care.
A Call for Continued Support and Funding
The success of digital pathology does not rest solely on technological advancements; it also requires sustained investment and widespread support. Community leaders, policymakers, and healthcare professionals must work together to secure funding that bridges the resource gap between urban and rural areas. Without adequate financial backing, even the most promising technologies can falter under the weight of practical challenges.
Investments in digital pathology yield dividends that go well beyond immediate financial returns. They ultimately translate into saved lives, more accurate treatments, and improved overall public health outcomes. To strengthen rural cancer care, it is essential to allocate resources toward:
- Training Programs: Developing education initiatives that help rural healthcare providers become proficient in digital technologies.
- Infrastructure Enhancements: Upgrading internet connectivity and ensuring secure digital storage across healthcare facilities.
- Research and Innovation: Funding clinical studies that explore new applications and refinements in digital pathology.
- Public-Private Partnerships: Encouraging collaborations that bring together different stakeholders to tackle the subtle parts of technological integration.
By addressing these key areas, we can ensure that the promising benefits of digital pathology extend to every corner of our healthcare system, reducing existing disparities and transforming the future of cancer care for rural populations.
Empowering Local Healthcare Providers through Education and Partnership
The shift toward digital pathology and telemedicine means that local healthcare providers must be empowered with the tools and knowledge necessary to embrace these changes. Continuous education is a must-have component in this evolving landscape. Regular training sessions, hands-on workshops, and virtual learning platforms can help bridge the nitty-gritty differences between conventional methods and modern technological approaches.
Moreover, establishing partnerships between urban medical centers and rural hospitals creates an environment of shared growth. These collaborations provide rural practitioners with direct access to expert consultations, online case reviews, and professional development opportunities. In essence, this network of support does more than just offer technical assistance—it builds a more resilient, integrated healthcare system that benefits patients at every level.
Key Strategies for Provider Empowerment
- Online Training Portals: Developing dedicated online modules focused on digital pathology applications and telemedicine protocols.
- Mentorship Programs: Pairing rural healthcare providers with experienced specialists for ongoing guidance.
- Collaborative Research: Engaging in joint studies that not only advance the science of digital pathology but also bring practical insights for rural applications.
- Regular Virtual Conferences: Hosting webinars and virtual conferences to discuss evolving trends and case studies in digital pathology.
These strategies help in smoothing out the rough edges of adopting new technology. With consistent training and support, healthcare professionals in remote areas can better manage the small twists of a rapidly changing medical landscape, ensuring that their patients receive crucial care without undue delays.
The Future of Digital Pathology in Rural Cancer Care
Digital pathology has already shown its transformative impact on cancer care, but this is only the beginning. As technological innovations continue to evolve, we can expect further improvement in the accuracy and speed of diagnoses. The integration of AI, enhanced imaging techniques, and streamlined telemedicine practices are all paving the way for a future where high-quality cancer care is within reach for every community.
Looking ahead, several factors will shape the future of digital pathology:
- Increased Adoption: As more institutions adopt digital workflows, the collective experience helps streamline processes and improve patient outcomes.
- Technological Refinement: Continuous improvements in imaging resolution and AI algorithms will enhance diagnostic precision even further.
- Expanded Collaborations: Greater integration between diverse medical specialties will enable a more holistic approach to cancer care, benefiting patients both in rural and urban settings.
- Policy Support: Forward-thinking policies will help ensure that digital pathology continues to advance while protecting patient privacy and data integrity.
The roadmap ahead illustrates a promising direction where the once intimidating gaps in cancer care are steadily being closed. Digital pathology is poised to become a super important element in transforming not only how we diagnose cancer but also how we support patients throughout their treatment journey.
Breaking Down Barriers for a Healthier Tomorrow
Every step taken today towards embracing digital pathology is a step towards breaking down the barriers that have long made accessing cancer care such a daunting task for rural populations. By taking advantage of advancements in technology, healthcare providers are not only making the diagnostic process more efficient but also fundamentally changing the way we think about and deliver care.
This convergence of technology, expert collaboration, and supportive policy is creating a robust network where every patient’s case is given the attention it deserves. With continuous investment and support from communities, governments, and healthcare organizations, the future of digital pathology shines brightly as a beacon of hope and progress.
Final Thoughts on Advancing Rural Cancer Care
Digital pathology is not just a technological upgrade—it represents a paradigm shift in our approach to cancer diagnosis and treatment. By easing the twists and turns that once complicated traditional pathology, this technology offers clear benefits in terms of speed, accuracy, and patient accessibility. For rural patients, who have long faced overwhelming hurdles in accessing specialized care, digital pathology is a welcome innovation that promises a more equitable healthcare future.
It is essential that we continue to support and fund these advances. With careful planning, robust training, and strong partnerships between all stakeholders, digital pathology can bridge the gap between rural and urban healthcare. The practical solutions discussed, from telemedicine integration to policy reform, pave the way for a future where every patient, regardless of location, can access the expert care they deserve.
As we take a closer look at the road ahead, the importance of investing in technology that helps untangle the confusing bits of cancer diagnosis cannot be overstated. Although challenges remain, the progress made so far is a testament to the power of innovation and collaboration. The benefits of digital pathology are clear: faster detection, more precise diagnoses, and ultimately, better patient outcomes.
A Roadmap for the Future
To summarize the ways forward, consider the following key points:
- Embrace New Technologies: Invest in state-of-the-art digital imaging and AI tools to support remote diagnosis.
- Strengthen Collaborative Networks: Foster partnerships between urban centers and rural clinics to facilitate expert consultations.
- Focus on Education and Training: Ensure that healthcare professionals are well-equipped to manage the subtle parts of digital pathology.
- Improve Infrastructure: Upgrade connectivity and secure digital storage systems across rural areas.
- Advocate for Supportive Policies: Work with policymakers to create an environment that accelerates technology adoption without compromising patient safety.
This combination of innovation, collaboration, and robust policy support is key to transforming cancer care in rural communities. Digital pathology represents a promising direction in our collective efforts to ensure that the best possible care reaches even the most remote corners of our society.
In Conclusion: A Shared Vision for Quality Cancer Care
The integration of digital pathology into rural cancer care is a prime example of how strategic thinking and technological advances can work together to solve the tricky parts of modern healthcare delivery. It allows experts to share knowledge more freely, speeds up the diagnostic process, and ultimately ensures that patients receive timely, accurate treatment recommendations.
While there are still many challenges to work through—from ensuring robust infrastructure to aligning policies and funding—each step taken in this direction is a valuable contribution towards a better future. By embracing digital pathology, we are not only addressing the immediate needs of cancer diagnosis but also setting the stage for continuous improvement that will benefit countless individuals in years to come.
The journey ahead may still involve some complicated pieces and the occasional nerve-racking obstacle, but the progress we have already seen is a testament to the power of innovation. Through continued investment, collaboration, and support, digital pathology will undoubtedly help bridge the health disparities that have long plagued rural communities, bringing sophisticated cancer care to patients no matter where they live.
In closing, this technological evolution is not just about upgrading our medical equipment—it’s about redefining what quality cancer care means for today’s world. By working together to support digital pathology, we are taking a confident stride toward a future where every individual can access the best possible care, without the limitations imposed by geography or resource disparities.
As healthcare professionals, policymakers, and community members, our commitment to making quality cancer care accessible and effective is paramount. It is by supporting advances like digital pathology that we can ensure a healthier, more equitable tomorrow for all.
Originally Post From https://www.moffitt.org/taking-care-of-your-health/taking-care-of-your-health-story-archive/digital-pathology-in-cancer-care-for-rural-communities/
Read more about this topic at
REVOLUTIONIZING RURAL HEALTHCARE: IMPLEMENTING …
AI-powered diagnostics: How do we ensure rural patients …