An Emerging Measles Outbreak in the Americas: A Cautionary Tale for Modern Public Health
The recent surge in measles cases across the Americas has stirred feelings that are both concerning and nerve-racking. Measles, caused by one of the most infectious viruses known to humankind, now looms as a stark reminder of the tangled issues associated with vaccine hesitancy and public misinformation. As we take a closer look at the situation, it becomes clear that both modern medicine and alternative health practices are being pushed to their limits, demanding a balanced conversation about prevention, treatment, and community health.
Once nearly eradicated in the United States due to widespread vaccination efforts, measles has reappeared amid falling immunization rates. This concerning trend is not exclusive to the United States; across the globe, vaccination rates – which are critical to establishing herd immunity – have plummeted. In many areas, the percentage of immunized children has stubbornly hovered around 83%, far below the super important 95% threshold required to fend off outbreaks.
Understanding the Measles Threat in the Modern World
Historical Perspective and Declining Immunization Rates
Historically, vaccines have been seen as a cornerstone of public health, protecting millions from diseases that once devastated communities. The United States, for example, enjoyed a near-eradication of measles thanks to widespread vaccine coverage. However, recent years have witnessed a palpable dip in vaccination rates. According to the Centers for Disease Control and Prevention (CDC), by 2019 only about 91.9% of Americans between the ages of 13 and 17 had received the recommended two doses of the measles, mumps, and rubella (MMR) vaccine.
This decline is particularly worrisome because measles is so contagious that even a small drop in immunization coverage can lead to large-scale outbreaks. The tricky parts of this dilemma lie in the fact that achieving herd immunity is not just a numerical goal—it requires community-wide trust and uptake of vaccines. When vaccination rates fall below the critical limit, areas become vulnerable to outbreaks, especially when unvaccinated individuals travel and inadvertently reintroduce the virus.
Below is a table that highlights vaccination coverage in different regions of the Americas, showcasing the fine points that contribute to our current predicament:
| Region | Vaccination Rate (%) | Comments |
|---|---|---|
| United States | Approximately 91.9% (13-17 years old) | Below the 95% threshold; majority of outbreaks appear in states with lower coverage. |
| Canada | Varies by province and territory | Some regions report over 95%, while others struggle to maintain herd immunity. |
| Mexico | Below optimal coverage | Recent outbreaks have been linked to inconsistent vaccination campaigns. |
| Overall Americas | Roughly 83% in some regions | Significantly under the ideal vaccination threshold, exposing communities to risk. |
The Challenge of Vaccine Hesitancy and Public Misinformation
Tangled Issues in Vaccine Acceptance
The re-emergence of measles is not solely a matter of biological vulnerability—it also reflects the complicated pieces of public trust and communication. With increasing skepticism towards established medical recommendations, many communities have witnessed a drop in vaccine uptake, often fueled by misinformation and personal beliefs that conflict with scientific consensus.
When unvaccinated or under-protected travelers become exposed to measles abroad, they often bring back the virus, causing domestic outbreaks. The situation is full of problems beyond the immediate medical risks: it highlights how vulnerable our public health systems are and how quickly misinformation can spread. Many experts argue that the responsibility to find your way through these challenges lies not just with individual communities, but with coordinated national and international health efforts.
The following bullet list summarizes some of the tangled issues impacting vaccine uptake:
- Distrust in government and healthcare institutions.
- Proliferation of alternative treatments that claim to replace vaccination.
- Lack of accessible, clear, and balanced scientific communication.
- Cultural and socio-economic factors that shape personal health choices.
- Rapid spread of unverified information through social media channels.
These factors combine to create a scenario in which even simple preventive measures are overwhelmed by a mix of modern-day challenges and hidden complexities in communication and trust.
Alternative Treatment Approaches: The Risk of Vitamin A Misuse
Examining Controversial Supplement Practices
In recent times, a controversial practice has taken center stage alongside the virulent measles outbreaks: the promotion of vitamin A as an alternative treatment. Proponents of alternative therapies, including some public figures, have claimed that vitamin A can play a preventive or curative role in measles treatment. However, a closer look at the available evidence reveals several confusing bits that caution against relying solely on such measures.
The U.S. Department of Health and Human Services (HHS) and the CDC have both issued recommendations stating that no specific, FDA-approved antiviral therapy exists for measles. Treatments are generally limited to supportive care aimed at easing symptoms such as fever and dehydration. The use of vitamin A, while sometimes beneficial in areas where deficiency is prevalent, is described as a supplement to care rather than a substitute for effective vaccination. The key details provided by health experts articulate that vitamin A might be administered under controlled conditions—but its unsupervised use can be overwhelming and even harmful.
Below are some of the risks associated with inappropriate use of vitamin A in treating measles and related conditions:
- Potential damage to the liver and central nervous system.
- Harmful effects on the skin and bones.
- Increased risk of severe birth defects in pregnant women.
- Instances of acute toxicity leading to hospitalization, as seen in some Texas cases.
When people start to poke around for alternative solutions, they may overlook the fine details of dosage, proper administration, and the lack of robust scientific backing for these alternative methods. Instead, they might gravitate towards unamply supported claims that measure up more to the allure of a quick fix than to actual, tested medical practice.
Public Health Implications and International Oversight
Limited Tools for Direct Measles Treatment
Measles is primarily a viral infection that presents with symptoms ranging from a simple rash and fever to more serious complications such as pneumonia and encephalitis. The limited available tools for treating measles directly underscore the importance of preventive measures. Since antibiotics are ineffective against viruses and there is no specific antiviral agent approved by the FDA, the super important focus remains on supportive care and, above all, vaccination.
Health authorities such as the World Health Organization (WHO) have expressed alarm at the current rates of infection in the Americas. With over 2,318 confirmed cases and an alarming rise from the previous year, the situation is indicative of not only domestic shortcomings but also international challenges in ensuring safe, effective vaccination programs.
Table 2 below provides a snapshot of the current outbreak statistics by country, painting a vivid picture of the challenges international public health officials face:
| Country | Confirmed Measles Cases | Notable Comments |
|---|---|---|
| Canada | 1,069+ | High incidence relative to population, indicating pockets of low immunization. |
| Mexico | 421+ | Shows mixed results where some regions maintain high levels while others lag. |
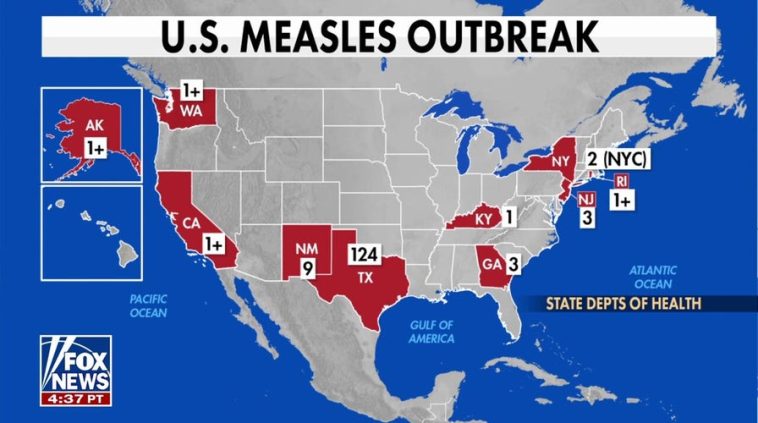
| United States | 1,001+ confirmed (with many suspected) | Outbreaks mainly in states with declining vaccination coverage. |
| Other Countries in the Americas | Rising numbers | Collective response is in early stages; more data needed. |
This snapshot shows the nerve-racking nature of the current outbreak. With such rapid growth in cases and many quiet carriers of the disease, the public health community finds itself pressed to find your way through strategies that can simultaneously manage local outbreaks and apply international safeguards.
Need for Concerted Global Action: Modern Medicine and Community Health
Key Steps to Rebuild Vaccination Trust and Improve Community Resilience
The emergence of this measles outbreak should serve as a wake-up call that modern medicine must not only address the immediate health crisis but also mend the community ties and trust that have frayed over recent times. The present issues are not on edge simply because of the virus’s inherent contagiousness; instead, they are on edge due to the many conflicting messages conveyed by various health authorities, alternative treatment advocates, and media outlets.
To manage your way through this situation, it is important to focus on several key areas:
- Improved Communication and Education: Clear and accessible information should be distributed widely to explain why vaccination is the most effective preventive measure, and why alternative practices, such as unsupervised vitamin A administration, are not substitutes for immunization.
- Enhanced Policy Interventions: Governments and public health agencies must update their strategies to compensate for the distorted messaging promoted by some groups. This includes reinforcing the credibility of scientific research and providing community-based education sessions.
- Community Involvement and Local Outreach: Local health centers should work closely with community leaders to ensure that cultural and socio-economic factors are taken into account. Tailor-made messaging that digs into the local concerns can go a long way toward rebuilding trust.
- International Collaboration: Given that diseases know no borders, it is essential that countries in the Americas and beyond coordinate their public health strategies, share timely data, and align their immunization and outbreak response policies.
Each of these measures is super important and must be executed with care, understanding the little twists that complicate the path towards a unified public health response. This is a multifaceted challenge that requires coordinated action from government bodies, healthcare providers, and the community at large.
Searching for Solutions Amidst the Confusing Bits of Treatment Options
Balancing Alternative Views with Evidence-Based Medical Practices
When faced with overwhelming health threats, people are often inclined to look for quick fixes. This tendency has given space to alternative treatments and off-putting recommendations—like the promotion of vitamin A for treating measles—despite the serious risks documented in various studies.
Critics argue that vitamin A, while potentially beneficial in specific contexts, should not be seen as a replacement for the tried-and-tested preventive measure of vaccination. The small distinctions between supportive care and direct curative intervention must be laid out clearly so that patients and their families can make informed decisions. It’s crucial to remember that:
- Supportive Care vs. Active Treatment: Symptom management with fluids and fever reducers is different from actively fighting a virus with targeted antiviral drugs—which, in the case of measles, do not currently exist.
- Risk vs. Reward: The benefits provided by a solid vaccination program far outweigh the potential dangers associated with unsupervised high-dosage vitamin A usage.
- Scientific Consensus: Peer-reviewed literature and public health guidelines have repeatedly confirmed that no alternative supplement can replace the protective effects of the measles vaccine.
To sort out these issues, policymakers and healthcare providers need to take a balanced approach that preserves traditional measures while cautiously evaluating any emerging evidence for supplementary interventions. This means that any claim of an alternative treatment must be backed by robust clinical data and administered under strict medical supervision.
In summary, the best way to make your way through the maze of treatment options is to rely on evidence-based practices. By doing so, the public avoids the pitfalls associated with enthusiastic but unsupported alternative treatments.
The Role of Policy and Public Health Messaging
Policy Recommendations and Action Plans for Measles Outbreak Management
It is clear that the current measles outbreak presents not only a medical emergency but also a challenge in public policy and communication. To build a more resilient system, several policy recommendations have emerged from experts, each aimed at addressing both the clear health risks and the subtle parts of misinformation and public distrust.
Key policy recommendations include:
- Strengthening Immunization Programs: It is essential to invest in campaigns that increase vaccination coverage. Subsidized vaccination drives, mobile vaccination units, and community outreach programs can help to ensure that immunization rates meet the super important threshold required for herd immunity.
- Regulatory Oversight on Supplemental Treatments: Health authorities should provide clear guidelines on the use of vitamin A and other potential adjunct treatments. This would mean stricter controls on unsupervised administration and educational campaigns on the risks involved.
- Clear and Consistent Public Health Messaging: Government agencies and healthcare institutions need to adopt messaging strategies that are neutral, accurate, and accessible. This includes leveraging digital platforms, social media, and community events to disseminate trustworthy information.
- International and Cross-State Collaboration: The measles outbreak does not respect borders. It is crucial that countries and states exchange data and coordinate response strategies. This can be achieved by establishing joint task forces and aligning on vaccination standards.
- Monitoring and Rapid Response Systems: Investment in surveillance systems that track vaccination rates, outbreak clusters, and the spread of misinformation can help officials figure a path early in addressing potential flare-ups.
Each of these recommendations demands thoughtful planning and consistent execution. The overall objective is to create an environment where both the general public and healthcare professionals are on the same page regarding disease prevention and outbreak management. With clear policies in place, it becomes easier to steer through the many twists and turns that currently characterize our public health landscape.
Community Empowerment and the Future of Public Health
Strengthening Local Networks and Rebuilding Trust
At the heart of the measles outbreak issue lies a broader narrative: the need to rebuild trust between the public and medical institutions. Amid widespread concerns about vaccination—and alternative suggestions such as vitamin A misuse—the real solution is to empower communities. Local health networks can play a crucial role in bridging the gap between national directives and individual beliefs.
Some strategies to enhance community-level resilience include:
- Community Forums and Town Hall Meetings: These can serve as platforms where local experts, healthcare providers, and community leaders come together to explain the importance of vaccinations and answer any questions that residents might have.
- School-Based Health Programs: Integrating health education into school curriculums helps instill early an understanding of immune health and the importance of vaccines. These programs can demystify the confusing bits of medical jargon that deter some parents from vaccinating their children.
- Partnerships with Local Influencers: Trusted community figures including religious leaders, educators, and local celebrities can aid in spreading the message that vaccination is a shared community responsibility.
- Feedback Mechanisms: Establishing hotlines, online portals, and other communication channels for community feedback can help health officials find their way through local concerns and quickly address misinformation.
By focusing on these grassroots initiatives, communities can begin to sort out the myriad issues that feed into vaccine hesitancy. Such efforts are not only essential for the immediate control of measles outbreaks but also serve as a blueprint for managing future public health challenges in an era where trust and clear communication are more important than ever.
Confronting the Overwhelming Complexity of Modern Healthcare Challenges
Balancing Evidence-Based Medicine with Alternative Health Narratives
The measles outbreak brings to the forefront a larger conversation about how modern medicine copes with competing narratives in today’s information-saturated landscape. Modern public health is continually tasked with balancing evidence-based practices with emerging alternatives championed by figures outside of the traditional medical sphere. The situation is often loaded with problems, as individuals are presented with multiple choices that can be both appealing and risky.
When alternatives such as vitamin A are promoted without comprehensive clinical oversight, the result can be as dangerous as it is confusing. To find your way through such challenges, both the medical community and the public at large must:
- Critically assess claims by seeking out peer-reviewed studies and recommendations from recognized health authorities.
- Understand that supportive care measures are not replacements for preventive measures—especially in the case of highly contagious diseases such as measles.
- Recognize that even seemingly simple preventive actions like getting vaccinated involve a series of tangled issues that go well beyond the individual decision.
This balancing act is like maneuvering through a labyrinth of scientific data, personal beliefs, and sometimes, conflicting advice. It calls for a thoughtful, informed, and patient approach where every decision is made based on an evaluation of risks and benefits.
Future Outlook: Strengthening Measles Prevention Strategies
Looking Ahead with Must-Have Preventative Measures
The current measles outbreak in the Americas is a vivid illustration of the effects of declining vaccination rates in an interconnected world. As we look to the future, it is super important to address both the medical and societal challenges that have allowed this situation to arise. The following must-have preventative measures are vital for reshaping our approach to such health crises:
- Routine Immunization Enhancement: Reinforce and modernize immunization schedules to ensure that every eligible individual is protected from measles and other vaccine-preventable diseases.
- Investing in Digital Health Communication: Support platforms that provide accurate health information. This includes combating misinformation and delivering clear messages that help individuals figure a path towards making informed health choices.
- Global Surveillance Systems: Strengthen international and cross-border disease monitoring systems to ensure rapid response in the face of emerging outbreaks. Coordinated efforts can prevent local outbreaks from escalating into regional or global health emergencies.
- Public-Private Partnerships: Encourage collaboration between government, healthcare institutions, and private organizations to drive innovation, research, and quality improvement in vaccination campaigns and outbreak management.
These strategies, if implemented efficiently, offer a way to not only halt the current spread of measles but also to fortify our defenses against future outbreaks. The stakes are high, and the timeline for action is now—every day’s delay could mean more cases, more hospitalizations, and in worst-case scenarios, more fatalities.
Conclusion: A Call for Unity and Vigilance in Public Health
Rebuilding Trust and Moving Forward Together
In conclusion, the expanding measles outbreak in the Americas should serve as a wake-up call and an opportune moment for reflection. The situation is an intricate weave of modern medical challenges, community mistrust, and the sometimes off-putting allure of alternative treatments. While the virus continues to spread amid declining vaccination rates and the confusing bits of competing narratives, the solution remains clear: robust, evidence-based vaccination programs complemented by clear public health messaging and community engagement.
As we take the wheel in combating this outbreak, it is essential that our responses are multi-pronged. We need to re-establish trust in modern medicine, support high immunization coverage, and ensure that preventative measures are both practical and backed by rigorous science. With concerted efforts from policymakers, healthcare providers, and communities around the globe, it is possible to overcome the intimidating challenges posed by contagious diseases like measles.
This opinion editorial is a call for unity—a reminder that while alternative approaches have their place, they should never overshadow the proven benefits of scientifically validated methods. Now more than ever, it is critical to steer through the tangled issues of misinformation and complacency and reaffirm our commitment to safeguarding public health.
Only by working together can we hope to manage your way through the delicate, yet critical, fine points of modern healthcare and ensure a safer, healthier future for all. Let us not allow the resurgence of an old enemy like measles to define our era. Instead, let it remind us of the must-have qualities—trust, clarity, and science—that will always be essential in the battle against infectious diseases.
In the coming years, as global mobility increases and the challenges of public health multiply, we must remain vigilant. The measles outbreak is not merely a transient problem but a signal that our struggles with vaccine hesitancy, misinformation, and alternative treatment risks are far from over. By maintaining focus on the tried-and-true methods alongside careful evaluation of new treatments, we can navigate the rapid twists and turns of modern healthcare challenges.
Let this editorial be both a reflection on the past and a roadmap for the future: one where public health policies are data-driven, communities are well-informed, and every individual understands that the small distinctions between science and pseudoscience can have profound consequences. Together, with action-oriented policies and unified efforts, we can overcome the intimidating obstacles of modern medicine and set a precedent for solving public health issues in a world where every voice counts.
The time to act is now. Let us commit, as a society, to prioritizing the super important task of vaccinating our communities, encouraging evidence-based healthcare practices, and ensuring that no single individual is left vulnerable to a preventable disease. In the end, whether through advanced modern techniques or through the careful adoption of supplemental strategies under strict medical supervision, our goal must remain clear: protecting life and fostering an environment where healthy choices are the easy choices.
As we move forward, may this renewed focus on vaccination and community trust pave the way for an era in which outbreaks are a rare occurrence rather than a recurring crisis. Let us take this experience, with all its tangled issues and challenging bits, and transform it into a lesson on the indomitable power of unity, science, and proactive public health measures. Only then can we ensure a future where we truly safeguard the health of every individual in our interconnected world.
Originally Post From https://www.labroots.com/trending/microbiology/28978/updates-expanding-measles-outbreak-americas
Read more about this topic at
Measles Cases and Outbreaks
Measles Outbreak – May 9, 2025 | Texas DSHS