Rectal Cancer and IBD: A Closer Look at Treatment Challenges
Recent research presented at the Digestive Disease Week 2025 Annual Meeting has shed new light on the tricky parts of treating rectal cancer in patients with inflammatory bowel disease (IBD). The findings indicate that patients facing the dual challenges of rectal cancer and IBD respond differently to standard neoadjuvant therapy compared to those with sporadic rectal cancer. This editorial will take a closer look at the study’s outcomes, discuss the potential reasons for this discrepancy, and explore the pressing need for more personalized treatment plans that take into account the tangled issues associated with IBD-related tumors.
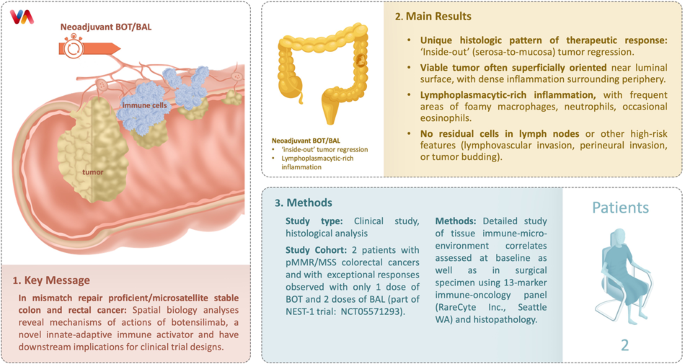
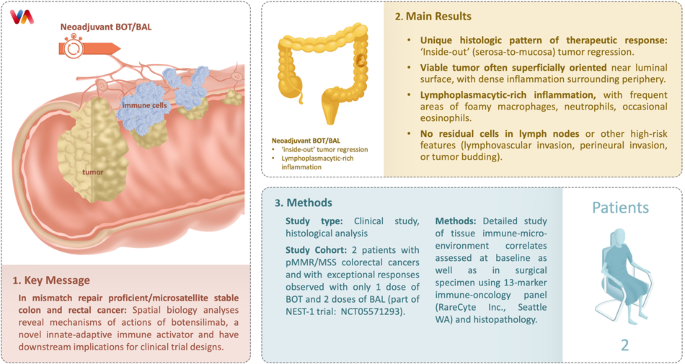
The study, which is the largest of its kind, compared outcomes between 92 IBD-rectal cancer patients and 92 matched sporadic rectal cancer patients. All study participants received some form of neoadjuvant treatment, including neoadjuvant chemoradiotherapy (CRT), short-course radiotherapy (scRT), or total neoadjuvant therapy (TNT). Although TNT has emerged as a standard of care in locally advanced rectal cancer (LARC), the research shows that its effectiveness might not be as pronounced in patients with IBD.
Treatment Responses: Comparing IBD-Associated and Sporadic Rectal Cancer
The study found that the pathologic complete response—where the tumor is undetectable after treatment—was significantly lower among IBD patients compared to those with sporadic rectal cancer (6.8% vs. 22.6%). This begs the question: why do IBD patients experience this suboptimal response? The answer could be hidden in the subtle differences of tumor biology and the impact of underlying chronic inflammation, which may render the cancer less receptive to standard treatment protocols.
It is important to remember that while the overall survival rates between the two groups were not significantly different, IBD patients did experience higher recurrence rates (37% vs. 22.8%), a factor that is loaded with clinical importance. These findings suggest that although neoadjuvant therapy is beneficial across the board, patients with IBD might require additional or alternative treatment strategies to improve outcomes.
Differences in Tumor Biology and Treatment Outcomes
One crucial element that emerged from the research is the differing tumor biology between IBD-associated rectal cancer and sporadic rectal cancer. In the study, poorly differentiated adenocarcinoma—a type of cancer with chaotic, less organized cells—was more commonly observed in IBD patients (32.7% vs. 7.4%). This suggests that the underlying biology in IBD-related cancers may be inherently more resistant to standard therapies.
The chronic inflammatory environment characteristic of IBD might lead to the development of cancer through unusual molecular pathways. These alternate pathways can result in tumors with unique, confusing bits of behavior, making them less predictable and more resistant to treatment. This observation raises the need for future research aimed at developing therapies tailored specifically to tackle these subtle differences, thereby improving the overall effectiveness of treatment in this patient group.
Personalizing Neoadjuvant Therapy for IBD Patients
The research underscores that despite the less favorable response, neoadjuvant therapy remains a critical component in the treatment strategy for IBD patients with rectal cancer. However, the probabilities of complete response indicate that we have a long way to go when it comes to optimizing treatment regimens. Personalized medicine, which aims to tailor interventions based on individual patient characteristics, holds the promise of addressing these small distinctions in tumor behavior.
Key considerations in developing personalized treatment include:
- Understanding the unique molecular profile of tumors in IBD patients
- Fine-tuning the dosage and combination of radiotherapy and chemotherapy
- Exploring novel agents that can target poorly differentiated cancer cells
- Incorporating patient-specific factors such as overall health and ECOG performance status
Recent trends in modern medicine emphasize the importance of integrating diagnostic markers, genetic profiles, and detailed imaging studies to create a more precise therapeutic approach. These small distinctions could be the key to determining which patients might benefit from alternative treatments, reducing recurrence rates while preserving quality of life.
Risk Factors and Underlying Mechanisms
The interplay between IBD and rectal cancer treatment outcomes is riddled with issues that complicate the typical approach to cancer therapy. IBD itself is characterized by chronic inflammation, which not only increases the risk of developing rectal cancer but also complicates its treatment. The study highlighted that many of these patients presented a higher baseline ECOG performance score, suggesting that their overall health might be compromised even before starting treatment.
In practical terms, the heightened risk of treatment-related complications among IBD patients cannot be overlooked. For instance, radiotherapy, a cornerstone of neoadjuvant treatment, is known to potentially exacerbate symptoms such as diarrhea or rectal bleeding. Past clinical practices have often regarded IBD as a relative contraindication for radiotherapy due to these nerve-racking side effects. Nonetheless, the promise shown in sporadic LARC patients has pushed clinicians towards using neoadjuvant therapy even in this high-risk context.
Decoding the Molecular Pathways of IBD-Associated Cancers
One of the most intriguing aspects of this study is the suggestion that the subtle differences in tumor biology are driven by the unique molecular pathways activated in the presence of IBD. The chronic inflammatory state can lead to mutations and alterations at the cellular level that are not typically encountered in sporadic rectal cancers. These hidden complexities in molecular behavior may contribute to the cancer’s resilience against conventional treatments.
A deeper understanding of these factors is super important if we are to develop more effective treatments. Ongoing research into biomarkers and genetic profiling in IBD patients stands to pave the way for novel therapeutic strategies that are capable of addressing these twisted bits of tumor behavior. Until then, clinicians have to carefully figure a path through an already challenging treatment landscape.
Potential Strategies for Overcoming Treatment Resistance
Given these findings, there is a clear need to re-examine and potentially revise the neoadjuvant treatment protocols for IBD patients. Some potential strategies that experts are considering include:
- Combination Therapies: Enhancing traditional treatment with targeted agents to overcome resistance.
- Adaptive Treatment Approaches: Modulating therapy based on a patient’s early response to treatment, allowing for course corrections.
- Immunotherapy Integration: Leveraging the body’s immune response to better target cancer cells, especially given the immune dysregulation observed in IBD.
- Dose Adjustment: Developing protocols for dose optimization in radiotherapy, reducing side effects while maintaining treatment efficacy.
Each of these approaches requires a thorough understanding of the nuanced differences between individual tumors. Multi-disciplinary collaborations between oncologists, gastroenterologists, radiologists, and even experts in alternative treatments are essential in carving a more effective treatment plan that accounts for each patient’s unique disease characteristics.
Integrating Modern Medicine with Alternative Approaches
While modern medicine provides the backbone for treating rectal cancer, the role of alternative medicine and nutritional support should not be overlooked, especially for IBD patients. These patients often face intense, nerve-racking treatment regimens that can leave their bodies severely depleted. Alternative therapies, such as acupuncture, nutritional interventions, and stress-reduction techniques, can be used adjunctively to help manage side effects and improve overall quality of life.
For patients undergoing intense therapy, diet and nutrition become key players in recovery and overall health. A diet rich in anti-inflammatory foods, antioxidants, and essential nutrients can help mitigate some of the side effects associated with cancer therapy. While these nutritional choices do not replace conventional cancer treatments, they serve as a complementary approach to bolster the immune system and aid in recovery.
Holistic Patient Management During Cancer Therapy
A holistic approach in managing patients with rectal cancer and IBD involves more than just treating the tumor. It requires careful management of the side effects, addressing the tricky parts of chronic inflammation, and optimizing overall well-being. Some strategies for holistic patient care include:
- Integrative Care Teams: Bringing together traditional oncologists, nutritionists, physical therapists, and alternative medicine practitioners to devise comprehensive treatment plans.
- Mind-Body Therapies: Implementing stress reduction techniques such as mindfulness, meditation, and yoga to help patients get around the overwhelming effects of treatment.
- Tailored Nutritional Support: Developing meal plans that focus on anti-inflammatory ingredients, ensuring that patients receive the key nutrients needed to support recovery.
- Pain and Symptom Management: Utilizing integrative therapies that consider both pharmaceutical and non-pharmaceutical interventions to ease symptoms like pain and severe gastrointestinal upset.
The integration of holistic methodologies with modern oncological care marks a promising frontier in managing the complex pieces of patient care in rectal cancer. It emphasizes that the path to recovery is not solely about eradicating the tumor but also includes steering through the adverse physical and emotional effects of intensive treatments.
Implications for Clinical Practice and Patient Counseling
The research presents several thought-provoking implications for how we counsel patients with IBD facing rectal cancer. One key takeaway is that patients with IBD should be counseled about the higher risk of recurrence and the possibility of a less robust response to standard neoadjuvant therapy. However, it is also important to emphasize that neoadjuvant therapy remains a cornerstone of treatment that still offers substantial benefits.
Patient empowerment through education is critical. When doctors take the time to explain the small distinctions between how IBD-associated tumors and sporadic tumors behave, patients can have more realistic expectations and engage actively in treatment decisions. While the numbers indicate a lower pathologic complete response rate for IBD patients, many still achieve at least a partial response, which is essential for improving long-term outcomes.
Setting Realistic Expectations with Patients
Effective patient counseling is super important, especially when discussing treatment plans that involve navigating through nerve-racking side effects and complicated treatment regimens. Here are some points to consider when engaging patients in conversation about their treatment:
- Clarify the Benefits and Limitations: Explain that while neoadjuvant therapy is beneficial for many, patients with IBD might experience outcomes that differ slightly.
- Discuss the Possibility of Recurrence: Be honest about the somewhat higher risk of cancer recurrence as evidenced by recent studies, while also highlighting strategies to manage this risk.
- Emphasize Multidisciplinary Care: Explain that a team of specialists, ranging from oncologists to nutrition experts, will be working together to create a tailored treatment plan.
- Encourage Active Participation: Empower patients to ask questions and discuss their treatment preferences, ensuring they feel involved in every step of the process.
These conversational approaches not only help set realistic expectations but also build trust between patients and healthcare providers. Ultimately, this leads to a more collaborative journey toward recovery.
Future Directions: Research and Innovative Therapies
The study’s findings underscore the need for future research aimed at tackling the subtle differences between IBD-associated rectal cancer and sporadic rectal cancer. With current data suggesting that IBD tumors might be inherently more resistant to standard therapies, researchers are called to explore novel approaches that can better target these tough-to-treat cancers.
Next-generation personalized therapies could significantly alter the landscape of treatment. Ongoing studies in genetic profiling, molecular markers, and the development of targeted agents are promising avenues that deserve further investment. By incorporating these innovative approaches, future treatment protocols could potentially provide improved responses while mitigating adverse side effects.
Pioneering New Therapeutic Avenues
The research community is increasingly recognizing that a one-size-fits-all approach to cancer therapy is no longer sufficient. With rectal cancer in IBD patients presenting unique, complicated pieces of tumor biology, there is a clear call for designing more adaptive, patient-specific treatment regimens. Some emerging avenues include:
- Genomic Profiling: Leveraging cutting-edge genetic tests to identify specific mutations in IBD-associated tumors, which can then guide the choice of targeted therapies.
- Immunotherapy: Exploring how immune checkpoint inhibitors and other immunomodulatory treatments might augment traditional neoadjuvant therapy by stimulating a more effective immune response against the tumor.
- Combination Drug Regimens: Testing combinations of chemotherapy, radiotherapy, and targeted biological agents to determine the most effective protocol for IBD patients.
- Adaptive Clinical Trials: Implementing flexible trial designs that allow adjustments to treatment protocols based on individual patient responses, ensuring that promising new interventions are rapidly validated.
As these new strategies are refined through clinical trials, it becomes increasingly important that both the research community and clinical practitioners collaborate closely. The ultimate goal is to transform findings from current studies into viable treatment options that can be readily implemented in clinical practice.
Bridging the Gap: The Role of Multidisciplinary Teams
The management of rectal cancer in patients with IBD is a clear example of where multidisciplinary collaboration is more than just desirable—it is essential. Since treatment success hinges on addressing both the disease and its associated side effects, a team-based approach that brings together diverse expertise is the most effective way to navigate through the maze of challenges.
Multidisciplinary teams typically include:
- Oncologists: Experts in cancer treatment who oversee the administration of neoadjuvant therapy, chemotherapy, and radiotherapy.
- Gastroenterologists: Specialists in IBD who manage the intricacies of chronic inflammation and its impact on the overall treatment regimen.
- Surgical Experts: Surgeons who are skilled in complex procedures such as low anterior resection and total proctocolectomy, essential for addressing the physical aspects of rectal cancer.
- Nutritionists: Professionals who assist in designing diets that can help mitigate treatment side effects and enhance healing.
- Pain and Symptom Management Specialists: Experts who work to ease the often intimidating and overwhelming side effects that come with intensive cancer treatments.
This collaborative approach not only improves the technical aspects of treatment but also ensures that patients receive holistic care that addresses both the physical and emotional challenges of facing cancer with IBD.
Improving Quality of Life Through Integrated Care
The ultimate aim of integrated care is to improve patient quality of life. By combining the expertise of multiple disciplines, healthcare providers can create treatment plans that are finely tuned to address each patient’s particular needs and circumstances. This is especially important when dealing with conditions as full of problems as rectal cancer in the setting of IBD.
Strategies to improve quality of life include:
| Focus Area | Approach |
|---|---|
| Symptom Management | Utilize integrative therapies along with conventional medicine to alleviate pain and discomfort. |
| Nutritional Support | Implement personalized meal plans rich in anti-inflammatory and antioxidant foods. |
| Mental Health | Offer counseling, stress reduction techniques, and peer support groups to help patients cope. |
| Functional Recovery | Incorporate physical therapy and other rehabilitative services to maintain physical function post-treatment. |
Each component of this integrated approach is designed to ensure that while the fight against cancer continues, patients are also supported in managing the nasty side effects, the overwhelming emotional strain, and the many tangled issues associated with long-term therapy.
The Road Ahead: Overcoming Challenges with Optimism
While the study presents some troubling data regarding the decreased efficacy of neoadjuvant therapy in IBD patients, it also offers a glimmer of hope. The fact that most IBD patients were able to complete their treatment regimen and obtain at least a partial response indicates that the current treatment protocols are not entirely off the mark. Instead, these results highlight the need for further innovation and adaptation in how we approach treatment.
There is reason to be optimistic in the future of rectal cancer management for patients with IBD. The obstacles outlined in the recent research are not insurmountable; they simply point to where adjustments must be made. Embracing the challenge of developing personalized, targeted treatments could transform the current landscape, reducing recurrence rates and leading to better long-term outcomes.
Embracing a Multifaceted Approach for Better Outcomes
It is clear that managing rectal cancer in IBD patients requires more than just a standard treatment protocol. The development of refined, personalized approaches meant to overcome the small twists in tumor biology is essential. To summarize, the road ahead involves:
- Continued Research: Funding and supporting studies aimed at understanding the unique molecular makeup of IBD-related cancers.
- Innovative Clinical Trials: Testing adaptive and combination therapies that specifically address the fine points of treatment resistance.
- Enhanced Multidisciplinary Collaboration: Leveraging the diverse expertise of various specialists to create comprehensive care plans.
- Patient-Centered Communication: Educating and empowering patients with realistic information to help them steer through their treatment journey.
Ultimately, the pressing need is not just to treat cancer but also to improve the quality of life for patients who are grappling with the added burden of IBD. A balanced approach that includes modern medicine along with supportive alternative therapies, nutritional adjustments, and psychosocial support could be the key to unlocking better outcomes.
Conclusion: A Call for Personalized, Holistic Care
The insights gained from the latest study on neoadjuvant therapy in rectal cancer patients with IBD serve as both a wake-up call and an opportunity for progress. While the response rates in IBD-associated cancers are not as encouraging as those observed in sporadic cases, there remains significant benefit in proceeding with neoadjuvant treatment. Moreover, these findings compel us to dig into the multifaceted nuances of tumor biology, emphasizing the need for a personalized, holistic approach to treatment.
For the medical community, this research underscores the importance of understanding not only the clinical outcomes but also the intricate, hidden complexities that distinguish IBD-associated cancers. It calls on healthcare providers to explore innovative treatments, improve multidisciplinary collaboration, and take a closer look at the fine details that can make a substantial difference in patient survival and quality of life.
For patients facing this challenging diagnosis, the message is one of cautious optimism. Yes, it is true that the current standard of care may not yield the same complete responses seen in sporadic rectal cancer cases. However, the ability to complete treatment and achieve partial remission is a vital step forward. With ongoing developments in personalized medicine, tailored treatment protocols, and comprehensive supportive care, the future looks increasingly promising.
As we try to get into these nerve-racking issues and figure a path towards more effective therapy, it is super important that both the research community and clinical practitioners remain committed to continuous improvement. By addressing the tiny details of each patient’s condition and embracing a holistic approach, we can pave the way for more favorable outcomes and an improved quality of life for all affected individuals.
In closing, let us remember that while the twists and turns involved in treating rectal cancer in the context of IBD are many, each effort to refine our approaches brings us closer to better survival rates and more personalized care. By staying flexible, innovative, and patient-centered, we can work together to overcome these daunting challenges and transform hope into tangible progress.
Originally Post From https://consultqd.clevelandclinic.org/rectal-cancer-patients-with-ibd-do-not-respond-as-well-to-neoadjuvant-therapy
Read more about this topic at
Inflammatory bowel disease (IBD) – Diagnosis and treatment
Inflammatory Bowel Disease (IBD)