The Hidden Challenges of Biased Data in Healthcare AI
Artificial intelligence (AI) is reshaping our healthcare landscape by offering promising solutions in diagnosis, treatment planning, and overall patient management. However, as we dive into this revolution, it becomes clear that the systems we build are only as good as the data that fuels them. In many cases, the training data is loaded with issues, predominantly due to its heavy reliance on sources from the United States and Western Europe. This opinion editorial takes a closer look at the tricky parts of biased training data, discusses the need for global and diverse data sources, and examines how incorporating alternative treatments and community insights can improve outcomes. By understanding these tangled issues, we can work toward a more equitable, personalized, and patient-focused future in healthcare AI.
At its core, AI in healthcare promises smarter, faster, and more precise approaches to patient care. But without addressing the confusing bits of bias and limited data scope, healthcare AI risks serving a narrow segment of the global population. As the technology becomes integral in tasks ranging from early sepsis detection to automating mundane charting and billing, we must acknowledge that current training practices are steering AI toward the norms and priorities of specific healthcare systems, leaving others in the shadows.
Understanding the Tricky Parts of Biased Data in Healthcare AI
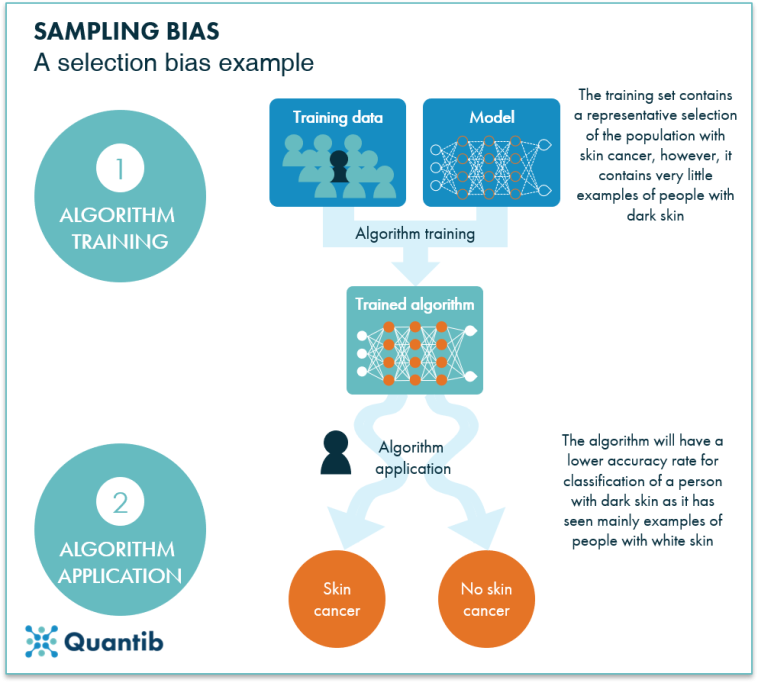
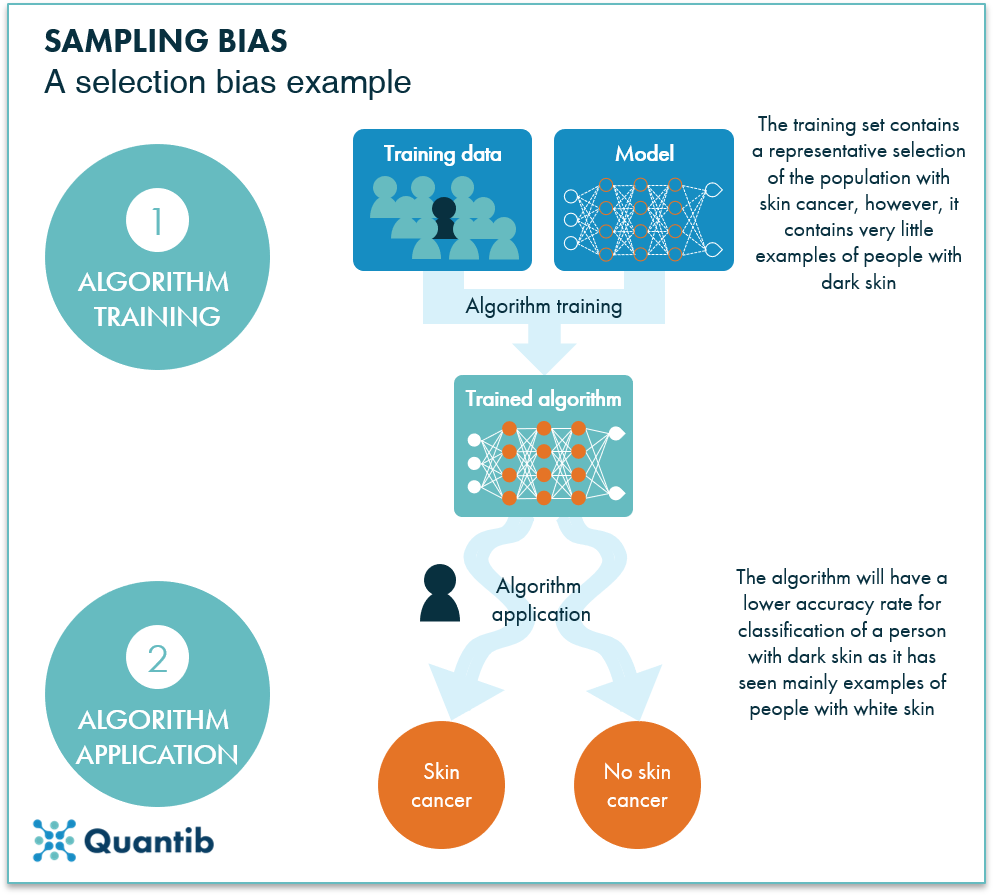
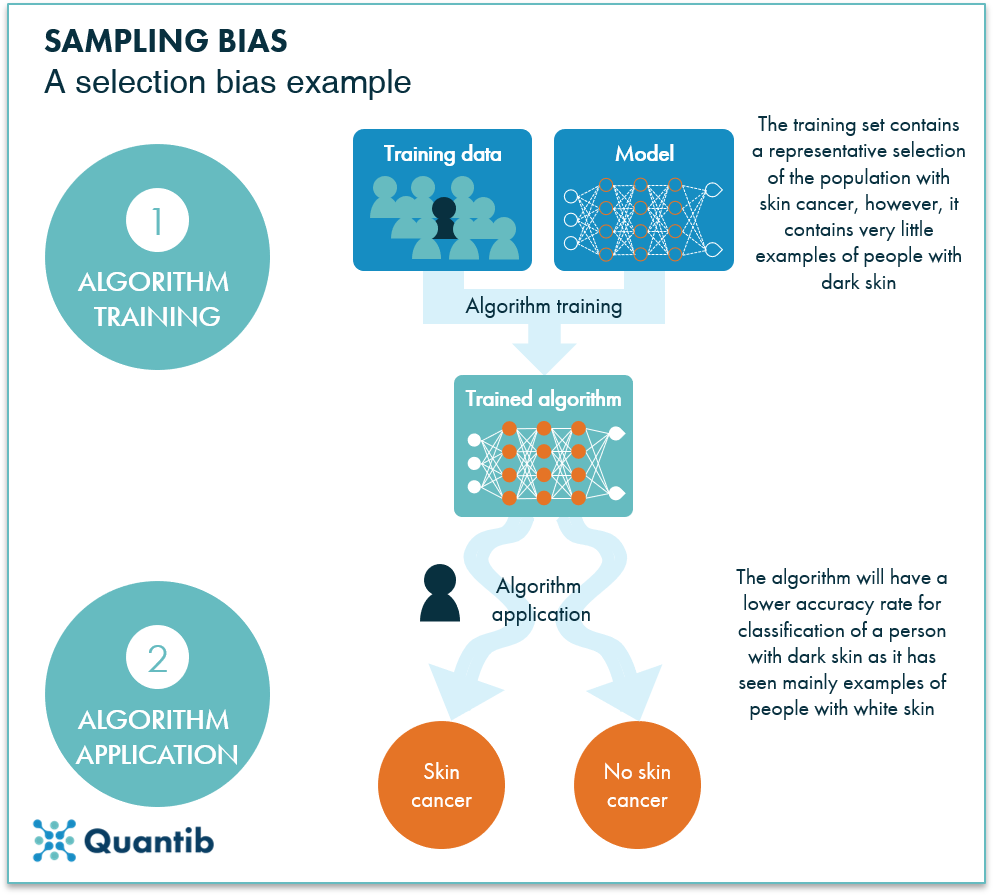
One of the most significant problems in healthcare AI is the quality and scope of its training data. For many AI models, the data primarily derives from electronic health records, insurance claims, clinical research studies, and published medical literature from affluent regions. This reliance creates a data set that is skewed toward middle-aged white patients in high-income countries. The biased nature of this data can lead to models that perform well for this group but are less effective—or even inaccurate—for underrepresented populations, including people of color, women, and individuals from low- and middle-income countries.
This situation is riddled with tension because AI models have a tendency to replicate the hidden complexities present in their training data. If the data does not represent the subtle parts of how diseases manifest across different populations or miss the little details inherent in various genetic backgrounds, the resulting algorithms could inadvertently embed systematic errors. For instance, if heart disease presentations in women are underrepresented, AI may struggle to diagnose or recommend appropriate treatments, worsening existing disparities in clinical care.
Additional studies have underscored these concerns. A study published in a leading medical journal indicated that many AI-driven clinical tools suffer from a lack of diversity in their data sources, thereby potentially reinforcing health inequities rather than alleviating them. As healthcare professionals and AI developers grapple with this issue, it is crucial to understand that without a more diverse foundation, the promise of AI may remain unrealized for many patients worldwide.
How Global Health Data Can Revolutionize Healthcare AI
There is an emerging call within the healthcare community to expand the data foundation beyond the US and Western Europe. By leveraging global health data, we stand a chance to develop AI systems that are more accurate, unbiased, and inclusive. This approach involves integrating datasets from countries with different healthcare practices, varied demographic profiles, and unique disease patterns. Doing so could enable AI to consider a broader spectrum of patient outcomes.
One clear benefit of incorporating international data is the ability to capture alternative treatment approaches that are not mainstream in the United States. For example, treatments effective in reducing vertigo symptoms in conditions like Meniere’s disease have been trialed successfully in parts of Europe but remain largely unknown in American practices, due to regulatory and financial barriers. By including international research and case studies in AI training, we may uncover effective therapies that benefit patients who have been overlooked by current models.
Expanding global data sources can also address the nerve-racking challenge of cultural and genetic diversity. When AI models are exposed to a truly global dataset, they begin to detect the fine shades and subtle details across different populations. This broader perspective not only improves diagnostic accuracy but also enriches treatment planning. A table below summarizes some of the key benefits of integrating global healthcare data into AI systems:
| Benefit | Description |
|---|---|
| Enhanced Diagnostic Accuracy | Exposure to diverse disease presentations improves the precision of AI diagnostics. |
| Broader Treatment Options | Inclusion of international research may reveal alternative therapies not widely used in the U.S. |
| Improved Patient Outcomes | Equitable data leads to AI recommendations tailored to a wider range of genetic and cultural backgrounds. |
| Reduction of Systemic Bias | Diverse datasets help minimize bias in training, leading to fairer outcomes for underrepresented groups. |
The integration of global data is not just a suggestion—it is a must-have step toward bridging the care gaps identified in current AI applications. However, making this shift requires strong international collaboration, new regulatory frameworks, and a commitment to shifting away from the one-size-fits-all approach that currently dominates healthcare research.
The Role of Genomic Data in Personalizing AI-Driven Treatments
Another critical component in improving AI systems for healthcare is the integration of genomic data. Our genetic makeup can significantly influence how we respond to medications, treatment strategies, and even disease progression. Incorporating genomic insights into AI models holds the key to unlocking truly personalized medicine.
Recent research underscores that patients who receive treatment plans based on their genetic profiles often show better responses and fewer side effects. By embedding genomic data into the training process, AI models can account for the fine points of individual variability. For instance, what may work for one genetic profile might not be as effective for another. This is especially important in conditions such as cancer and cardiovascular diseases, where genetic differences can be a deciding factor in treatment success.
Incorporating genomic data can also help steer through trickier treatment scenarios where traditional protocols fall short. Without a comprehensive understanding of the genetic underpinnings influencing patient outcomes, AI might miss out on subtle indications that could lead to better-targeted therapies. The following bullet list outlines some benefits of integrating genomics into AI healthcare models:
- Improved precision in drug selection and dosage adjustments.
- Better prediction of patient responses and side effects.
- Enhanced understanding of disease mechanisms at the molecular level.
- Opportunities for developing customized treatment plans tailored to the individual.
This personalized approach not only aligns with the ideals of patient-focused care but also helps address the missed fine shades in current AI models. It is a reminder that in healthcare, one size does not fit all, and our next generation of AI systems must mirror that diversity.
Alternative Therapies and Community-Driven Insights in AI
In an era where AI can seem overwhelming with its promise of technology-driven progress, it is essential to remember that effective patient care sometimes exists outside the bounds of conventional medicine. There is great value in considering alternative treatments and community-driven insights when developing AI systems in healthcare. Many alternative therapies, though not part of standard protocols in the United States, have shown promising results in other parts of the world.
For example, treatments focusing on holistic health, traditional medicine systems, and non-pharmaceutical interventions have been used for centuries to manage chronic conditions. These approaches, when validated through rigorous study, can offer safe and effective alternatives to patients who may not benefit from standard care pathways. Unfortunately, AI systems that are solely trained on conventional medical data are likely to overlook these innovative approaches.
Moreover, crowdsourced insights from local healthcare professionals and community health experts could be enormously beneficial in filling in the confusing bits left by formal data sources. Unlike clinical trials and big data studies, community-driven information can capture the nuances of patient experiences and local treatment variations. The following table outlines key areas where alternative therapies and community insights can add value to AI in healthcare:
| Area of Improvement | Potential Benefits |
|---|---|
| Broader Treatment Options | Inclusion of traditional and alternative approaches alongside conventional treatments. |
| Localized Healthcare Solutions | Tailoring treatment recommendations based on community practices and available resources. |
| Enhanced Patient Engagement | Leveraging community knowledge builds trust between healthcare providers and patients. |
| Innovative Approaches | Encouraging the consideration of non-standard treatment modalities that may benefit specific patient groups. |
Community-driven data sources also offer a mechanism to cross-check and verify the recommendations made by AI, functioning as a kind of fact-checking system for clinical insights. This collaborative approach ensures that the AI’s decisions are not just based on historical and often dated data, but are enriched by real-world experiences and perspectives.
Steps to Mitigate Bias for Equitable AI-Driven Healthcare
To truly harness the promise of AI in healthcare, it is essential to address the overwhelming bias at the root of current models. This requires a multi-faceted strategy that not only enhances the data inputs but also improves the mechanisms through which AI learns and adapts. Here are several super important steps that stakeholders can take:
- Diversify Data Sources: Broaden the training dataset by incorporating global health data, community-sourced information, and alternative treatment research. A more extensive dataset can help reduce the risk of developing AI systems that favor one demographic over another.
- Integrate Genomic Information: By embedding genomic data alongside traditional medical records, AI can account for individual genetic differences, leading to better-targeted therapies and reduced adverse reactions.
- Incorporate Alternative Therapies: Allow AI training to include non-conventional treatments that have proven effective in various cultural settings. This can provide a more complete picture of patient care and innovate how conditions are managed.
- Collaborate with Global Experts: Encourage partnerships between international healthcare providers, AI developers, and regulatory bodies to craft guidelines that ensure the inclusion of diversified data.
- Constant Re-Evaluation: Create feedback loops where AI recommendations are continuously validated by healthcare professionals. This helps catch any missteps early and ensures the system is always tuned to the best patient outcomes.
Following these steps is not just a technical necessity—it is an ethical imperative. We owe it to patients worldwide to develop AI systems that are as inclusive and unbiased as possible. Doing so can pave the way for a healthcare landscape in which technological progress does not come at the expense of equity.
The Future of AI in Healthcare: Building a Patient-Centered Model
While the current state of healthcare AI is promising, it is evident that there are considerable twists and turns ahead. The future of these systems hinges on a collective willingness to take a closer look at what data is being used and from whom it is being derived. Rather than continuing with a narrow focus that favors certain demographics or regions, the goal should be to create systems that mirror the diversity of the global population.
It is equally off-putting to see technology that is so advanced yet remains limited by its inability to capture the fine points of human diversity. Imagine a future in which AI models are not only smart enough to predict patient risks but are also flexible enough to factor in cultural practices, localized treatment modalities, and even non-pharmaceutical remedies. This future is within reach, but only if we commit to broadening our data landscape and continuously testing AI outcomes against real-world experiences.
The optimistic side of this journey is that many researchers, tech companies, and health organizations are beginning to adopt a more holistic approach. They are diving into initiatives that look beyond traditional data pools and explore alternative insights. Such initiatives include:
- International consortiums for sharing anonymized health data.
- Collaborative research projects that combine genomic data with clinical outcomes.
- Platforms that aggregate community insights to cross-verify AI recommendations.
- Pilot programs in low- and middle-income countries to collect and share local health data.
These steps, although they may seem like small distinctions at first, represent a key movement toward a more inclusive and patient-focused healthcare system. The ultimate aim is to forge an AI that not only recognizes but celebrates the subtle differences in patient profiles, leading to care that is as unique as each individual.
Addressing Regulatory and Ethical Considerations
As we sort out the path toward better, more inclusive healthcare AI, we must also contend with the intimidating regulatory and ethical challenges that arise. Establishing guidelines for data collection, usage, and continuous monitoring is essential to ensure that these systems are not misused or replete with outdated biases. Regulatory bodies must be involved in every step of this process to maintain transparency, fairness, and patient safety.
One possible solution to these challenges is the creation of an independent oversight committee composed of international experts. This committee could periodically review the training data, the emerging outcomes, and the overall impact of AI on patient care. Their role would be to provide actionable feedback and to recommend adjustments as needed, ensuring that AI remains a tool that serves the best interests of patients rather than industry or regulatory norms.
In addition, ethical guidelines are essential when it comes to protecting patient data and maintaining privacy. With the accumulation of vast amounts of health-related information, the risks associated with data breaches or misuse are real. Transparent data governance, informed consent processes, and secure data management practices must be super important pillars of any AI deployment in healthcare. By addressing these nerve-racking concerns head-on, we can pave the way for a more ethically sound and effective integration of AI in medical practice.
Learning from Success Stories and Ongoing Research
Several early adopters and research projects around the globe are already demonstrating how a more inclusive approach to AI training data can result in improved patient outcomes. For instance, pilot programs that integrate international data sources and genomic insights have shown promising results in areas such as oncology and cardiology. These success stories serve as a testament to the potential of AI when it is built on a rich, diverse foundation.
Furthermore, healthcare providers have begun to see the benefits of AI-powered diagnostic tools that have been fine-tuned with community insights and alternative treatment data. In many cases, these systems have identified treatment options that standard protocols might have overlooked, thus offering patients new hope and better management of chronic conditions.
A few highlights from ongoing research include:
- The use of AI to predict early signs of sepsis in hospitals that combine traditional indicators with global data trends.
- Projects that integrate genomic data to personalize cancer treatment, resulting in fewer side effects and improved survival rates.
- Collaborative AI models that routinely incorporate community feedback to adjust treatment recommendations in real time.
These examples are inspiring, yet they also emphasize the need for a sustained effort. Continuing to invest in research, international collaboration, and alternative data sources will be critical if AI is to become a transformative tool for equitable healthcare.
Overcoming Obstacles: A Call for Collaborative Action
The path forward is undoubtedly complicated, with many confusing bits to navigate and nerve-racking regulatory challenges to address. However, the global healthcare community has an unparalleled opportunity to harness the power of AI in ways that resonate with the diverse populations it aims to serve. Achieving this goal will require the collective efforts of data scientists, healthcare professionals, regulatory agencies, and community health representatives working together.
An effective strategy to overcome these obstacles includes:
- Establishing global data-sharing agreements that protect patient privacy while expanding the data pool.
- Encouraging cross-cultural collaborations that test AI models in diverse environments.
- Investing in infrastructure and training to support the collection of high-quality, representative health data worldwide.
- Promoting ethical practices and regulatory oversight to ensure that the development of AI remains patient-centric.
By taking these steps, stakeholders can figure a path through the tangled issues that currently limit AI’s full potential. The ultimate reward is a healthcare system that not only leverages advanced technology but also respects the individuality and cultural diversity of every patient it serves.
Conclusion: Building an Inclusive, Patient-Focused Future in Healthcare AI
In conclusion, the evolution of healthcare AI offers immense promise, but its success is intricately tied to the data that trains it. The overwhelming reliance on data from specific Western sources has introduced a range of tricky parts—from misdiagnoses to missed treatment options—that could widen existing healthcare disparities. By integrating global health data, genomic information, alternative therapies, and community insights, we can create AI systems that are more robust, equitable, and truly personalized.
This journey is not without its intimidating challenges. Regulatory hurdles, ethical concerns, and the ongoing need to manage your way through biased data stand as significant barriers. However, with coordinated global efforts and a commitment to diversify our data foundations, these obstacles are far from insurmountable. The healthcare industry must prioritize expanding and refining the data that informs AI, ensuring that future models are built on a rich tapestry of global insights rather than a narrow, localized view.
As we look ahead, the future of medicine is bright if we can truly leverage AI for the benefit of all patients. The key lies in constructing systems that are full of diverse perspectives—systems that understand the little twists of genetic makeup, the substantial value of community-driven insights, and the proven merit of alternative treatments. Only then can we create an AI-driven healthcare environment that is fair, responsive, and built to serve the true needs of every individual.
It is incumbent upon healthcare leaders, researchers, and policymakers to take the necessary steps. By broadening training data to include global insights, integrating genomics into standard practice, and embracing alternative therapeutic approaches, we can overcome the current limitations. In doing so, we not only enhance the accuracy and effectiveness of AI but also forge a path for a more inclusive, patient-centered future.
Healthcare AI has arrived at a crossroads. The choices made today regarding data inclusivity and diversity will shape the patient outcomes of tomorrow. Let us make a resolute commitment to build and support systems that are as diverse as the patients they serve. The transformation of healthcare is within our grasp—provided we are willing to acknowledge the confused bits in our current approach and take innovative steps toward a more equitable and accurate AI-powered future.
In the end, the potential of AI in healthcare extends far beyond the confines of any single system or region. It is about crafting a future where technology serves humanity holistically, where every diagnosis, treatment plan, and patient recommendation reflects the full spectrum of human experience. By committing to inclusivity, transparency, and continual learning, we can ensure that the promise of AI is realized in a way that is truly transformative for global healthcare.
As we take that crucial step forward, let us remember that the technology is only as strong as its data. With a broader, more inclusive data set that respects and represents our global community, healthcare AI will not only be smart enough to detect disease but will be wise enough to understand the subtle differences that make each patient unique. In that lies the true power of AI—a tool capable of delivering care that is both innovative and deeply personalized.
Originally Post From https://www.medicaleconomics.com/view/trained-to-fail-the-risk-of-biased-data-in-health-care-ai
Read more about this topic at
Diversifying Data to Beat Bias in AI
More Diverse Data Makes for Smarter AI