Real-World Evidence in Prostate Cancer Therapies: A Fresh Look at Evolving Treatment Paradigms
In recent years, the medical community has been buzzing with discussions about whether clinical trials faithfully predict how prostate cancer therapies perform in everyday practice. As we get into an age where cancer treatments are advancing quickly, it’s both exciting and nerve-racking to see how new drugs stand up to the test of real-world usage. A recent study comparing randomized controlled trials with real-life outcomes for drugs approved between 2010 and 2019 provides fresh insights and lends confidence to the idea that clinical trial findings can indeed mirror real-world results.
This study has sparked a healthy dialogue among healthcare professionals, patients, and researchers alike. Experts like Dr. Stephen J. Freedland from Cedars-Sinai have shared that, while challenges remain in collecting long-term data, the overall effectiveness seen in clinical trials appears to translate well into everyday practice. In this opinion editorial, we will get into the workings of clinical trials, examine the tricky parts of statistical study design in measuring long-term outcomes, and offer an insider’s view of how these findings impact our understanding of evolving prostate cancer therapies.
Clinical Trials vs. Everyday Drug Performance: Weighing the Evidence
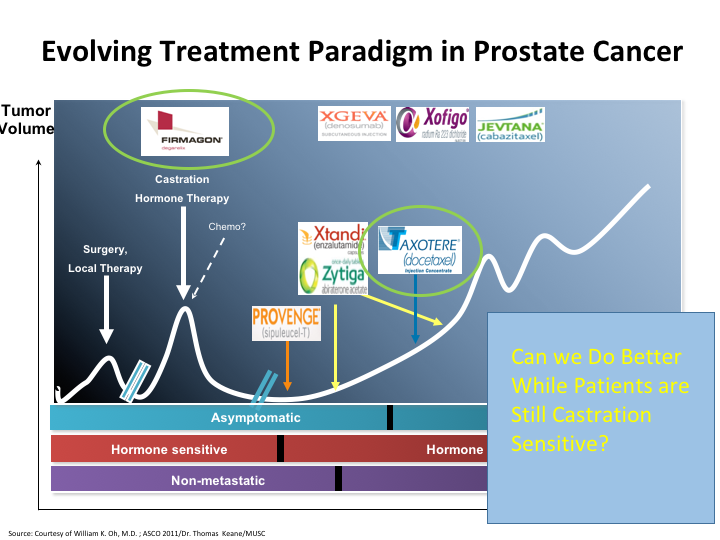
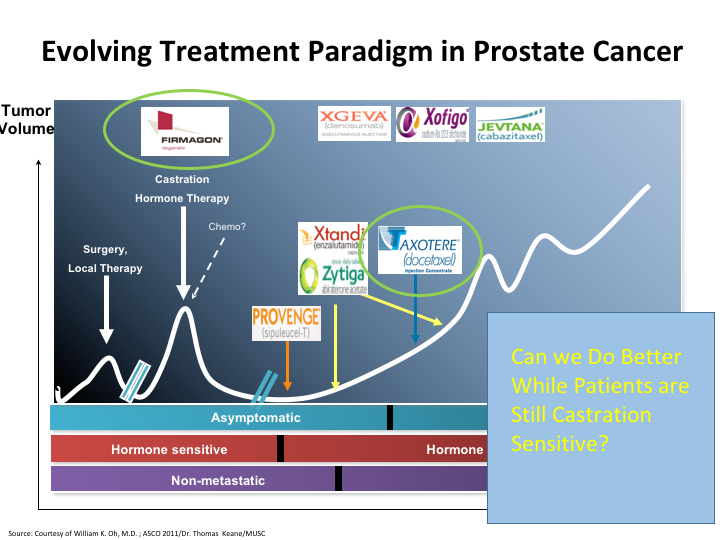
A central point raised by recent research is that treatments showing promise in clinical trials continue to demonstrate similar or even better performance in the real world. While a controlled study environment may appear isolated compared to everyday clinical settings, the real-life application of these therapies often reveals additional benefits. Dr. Freedland pointed out that the study looked at drugs with three distinctly different mechanisms of action: androgen-targeted therapies, radiopharmaceuticals, and immunotherapy. Each of these approaches showed comparable or improved outcomes in day-to-day clinical use.
The study’s findings are critical because they provide reassurance that the drugs developed through rigorous trial protocols are not just effective on paper but also in the complex, unpredictable environment of patient care. This evidence is not only encouraging for clinicians but also for patients who face a nerve-racking battle against prostate cancer.
Statistical Study Design: Tackling the Tricky Parts
One of the main hurdles in comparing trial results with real-world effectiveness is dealing with the tangled issues inherent to statistical study design. Studies must allow enough time after a drug’s approval to track patient outcomes, which means data might lag by a few years. This delay makes it a bit overwhelming for researchers trying to assess the true impact of a new therapy promptly.
The fine points of statistical evaluation in these studies involve:
- Ensuring a sufficient follow-up period to capture long-term outcomes
- Adjusting for variables that differ between controlled trial participants and the broader patient population
- Addressing the small distinctions in how different subgroups respond to therapy
Even with these challenges, the consistency in efficacy across various drug classes is a promising sign. It suggests that, despite the complicated pieces of statistical analysis and the nerve-racking wait for long-term data, the clinical trials are indeed a reliable predictor of a drug’s real-world performance.
Broader Implications for Drug Development and Patient Care
This emerging evidence has broad implications for drug development and patient care. If clinical trial results continue to mirror real-life outcomes, the process for bringing new treatments to market may be influenced in several key ways:
- Accelerated Approval Pathways: Regulatory bodies might consider streamlined processes for drugs that show promise in early clinical testing, given the supportive real-world data.
- Confidence in New Mechanisms: Observations that multiple drug classes perform well help alleviate some of the scary uncertainty surrounding new mechanisms of action in therapy.
- Broader Patient Inclusion: Recognizing that controlled trial settings can closely mimic everyday practice might encourage more inclusive trial designs, thereby reflecting a diverse patient population.
These points are not just academic—they affect decisions in actual patient treatments, from adjusting dosage considerations to counseling patients on what to expect from their therapy. When healthcare providers are confident in the real-life application of clinical trial data, it makes their decision-making process a bit less intimidating and offers a clearer path to effective patient care.
Understanding Mechanisms of Action: Androgen-Targeted Therapies, Radiopharmaceuticals, and Immunotherapy
One of the most compelling aspects of the recent study is its comparison of different therapeutic mechanisms. By analyzing androgen-targeted therapies alongside radiopharmaceuticals and immunotherapy, the research offers a multi-faceted view of treatment performance in the real world.
Let’s take a closer look at each approach:
Androgen-Targeted Therapies
These medications work by disrupting the role of androgens (male hormones) in the growth of prostate cancer cells. Clinical trials have long shown their efficacy in slowing the progression of the disease. The reassuring part from the study is that their real-world performance aligns quite well with the controlled trial results. This continuity suggests that androgen-targeted therapies are robust across various clinical settings.
Key factors relating to these therapies include:
- Reliable performance in reducing tumor progression
- Low incidence of unexpected side effects in everyday use
- Consistent patient outcomes over extended follow-up periods
Radiopharmaceuticals
Radiopharmaceuticals offer targeted radiation therapy to cancer cells while sparing normal tissues. They have been a subject of excitement due to their dual role in diagnosis and treatment. Real-world evidence suggests that these agents not only work as expected in clinical trials but may also provide enhanced benefits when used in routine patient care.
This class of drugs has shown promise in:
- Delivering focused treatment with manageable side effects
- Extending survival times in patients with advanced disease
- Potentially improving quality of life through targeted action
Immunotherapy
Immunotherapy harnesses the body’s immune system to fight cancer, offering a novel approach distinct from traditional chemotherapies and hormone therapies. In clinical studies, these agents have sometimes produced mixed results due to the small details of individual immune responses. However, the study at hand found that immunotherapy demonstrated similar, if not better, effectiveness outside of the trial environment.
Considerations for immunotherapy include:
- The variability in patient immune responses and the need for personalized treatment strategies
- Potential for long-term remission in a subset of patients
- The importance of identifying biomarkers that predict success
Embracing a Data-Driven Future: The Journey Ahead
As we look to the future of prostate cancer therapies, the convergence of clinical trial results and real-world outcomes offers a promising roadmap. However, it is important to remember that each new drug, each new mechanism of action, will need its own rigorous study. The real-world data we have today is a snapshot that grows more detailed with time.
Some of the challenges that lie ahead include:
- Collecting and analyzing data over longer periods to detect late-emerging effects
- Incorporating diverse patient populations into future studies to ensure broad applicability
- Refining methods to manage the fine details of statistical study design and patient follow-up
Despite these tricky parts, the overall trend is encouraging. The quality of clinical trial design and subsequent real-world results is a testament to the rigorous work done by researchers over many years. It’s an important reminder that while there are twists and turns in the road to new therapies, the destination—a world with safer, more effective treatments—is well within reach.
Integrating Modern Medicine with Patient-Centered Care
A critical piece of this evolving narrative is how real-world data reinforces the broader goals of patient-centered care. When healthcare providers see that trial results hold true in daily practice, it builds trust in the overall treatment approach. This leads to several key benefits:
- Informed Decision Making: Patients can be more confidently informed about the potential outcomes and side effects of their treatment options.
- Optimized Treatment Plans: Physicians have a clearer roadmap when adjusting dosing or combining treatments, ensuring that patient care is as effective as possible.
- Enhanced Communication: Real-world evidence provides a common ground for discussion, making the sometimes overwhelming science behind these treatments a bit more accessible for patients and their families.
As important as it is to rely on the power of clinical data, we must also remember that every patient is unique. The subtle parts of their medical history, lifestyle, and overall health can influence how well they respond to therapy. Future studies and ongoing data collection efforts should aim to account for these small distinctions, ensuring that the broad success seen in real-world populations is equally beneficial on an individual level.
Alternative Approaches and Holistic Considerations in Prostate Cancer Management
While mainstream treatments dominate the conversation, it is also worth examining how complementary strategies might play a role in managing prostate cancer. Alternative medicine, nutrition, and fitness regimes have an increasingly recognized role in supporting patients during and after treatment.
Complementary Therapies and Their Role
Many patients find that integrating complementary therapies with conventional treatments helps them handle the nerve-racking journey of cancer care. These therapies, which can include nutritional adjustments, herbal supplements, and mind-body techniques, may offer relief from treatment-related side effects and improve quality of life.
Practical suggestions for integrating complementary approaches include:
- Nutritional Guidance: Focusing on whole foods, reducing red meat intake, and increasing fruits and vegetables can help maintain overall health during treatment.
- Physical Activity: Engaging in regular, moderate exercise—be it brisk walking, yoga, or swimming—can ease some of the overwhelming physical side effects associated with cancer treatments.
- Mind-Body Techniques: Practices such as meditation, acupuncture, or gentle stretching may help manage stress and improve overall well-being.
It’s important to note that while these complementary methods might not cure cancer on their own, they serve as valuable tools for enhancing overall patient wellness. They offer patients a way to maintain balance, even as they work through the complicated pieces of cancer treatment.
Nutrition and Lifestyle: Building a Strong Foundation
Nutrition plays a super important role in how patients withstand and recover from cancer treatments. A balanced diet rich in antioxidants, fiber, and lean proteins can help stabilize energy levels and support the immune system during the treatment process. Additionally, managing weight through diet and exercise can improve outcomes by reducing the risk of treatment complications.
Key nutritional considerations include:
- Emphasizing Plant-Based Foods: A diet abundant in fruits, vegetables, and whole grains is known to provide essential vitamins and minerals.
- Reducing Processed Foods: Cutting back on processed and high-sugar foods may help reduce inflammation and support overall health.
- Staying Hydrated: Proper hydration is essential for the detoxification processes in the body and overall cellular health.
Incorporating regular physical activity, even gentle forms tailored to a patient’s individual circumstances, is another key factor. Whether it’s a short walk or a structured exercise program, staying active helps mitigate the detrimental effects of prolonged immobility often faced by patients undergoing treatment.
Patient-Centered Perspectives: Balancing Evidence with Individual Needs
Despite robust data from clinical studies and real-world evidence, the connection between research findings and individual patient experience is full of problems that require careful attention. Every patient’s journey is unique, and the path through treatment often involves navigating a maze of choices and adjustments.
Here are a few suggestions for optimizing patient-centered care in light of current evidence:
- Personalized Treatment Plans: Physicians should tailor treatment strategies based on individual characteristics rather than a one-size-fits-all approach. This means considering factors such as age, overall health, and genetic predispositions.
- Transparent Communication: Medical professionals must take a closer look at patient concerns. Open dialogue about how treatments might work in real-life settings helps reduce the confusion and the overwhelming aspects of making decisions.
- Long-Term Follow-Up: Continuous monitoring allows for adjustments that can improve both efficacy and quality of life over time. This process ensures that the fine shades of each patient’s experience are respected and addressed.
Enhancing patient-centered care with these components not only helps in finding your way through the complications of cancer treatment but also reinforces the trust between patients and their healthcare teams. This trust is essential in managing expectations and delivering care that aligns with both clinical evidence and individual lifestyle needs.
Exploring the Broader Impact of Real-World Studies on Prostate Cancer Management
The wealth of real-world evidence emerging from studies on prostate cancer therapies doesn’t just benefit clinicians and researchers—it also has significant ramifications on healthcare policy and resource allocation. As data continues to pile up, stakeholders are taking a closer look at how best to integrate these findings into everyday practice.
Some of the broader impacts include:
- Informed Health Policies: Policy makers can use real-world data to craft regulations that support effective treatments while providing flexibility for emerging therapies.
- Enhanced Reimbursement Models: Insurance providers may adjust their reimbursement strategies based on consistent real-life outcomes, ensuring that patients have access to the latest treatment options.
- Resource Allocation in Healthcare Facilities: Hospitals and clinics may reconsider how they invest in treatment infrastructure, potentially prioritizing therapies that have demonstrated solid performance beyond clinical trial settings.
This data-driven approach also opens the door to a new dialogue between regulatory bodies and the pharmaceutical industry, fostering an environment where both innovation and safety are front and center. It is a fine balance between encouraging new developments while managing the hidden complexities of long-term treatment outcomes.
Charting a Course for Future Research and Development
Looking ahead, the success of current prostate cancer therapies in both controlled trial environments and real-world settings signals a promising future—but it also underscores the need for continued research. Here are some key areas for future exploration:
- Extended Follow-Up Studies: There is a pressing need for long-term data to capture late treatment effects and accurately assess the benefits over time. Researchers should commit to extended follow-up periods that go beyond the initial years post-approval.
- Diverse Patient Populations: Future clinical trials must include a broader range of patients. Diverse study populations help ensure that the benefits seen in trials extend to everyone, including minority groups and those with coexisting conditions.
- Innovation in Statistical Methods: Developing new statistical methods to manage the fine points of real-world data analysis will be key. This includes finding new ways to account for small twists in data generated in uncontrolled settings.
It’s also worth noting that as more drugs enter the market with novel mechanisms of action, each will require its own careful study. While the current study provides a reassuring blueprint, each new therapy must be assessed on its own merits. This context not only helps refine research methods but also supports the idea that patient outcomes remain at the heart of medical advancement.
Healthcare professionals, researchers, and policy makers must work together to ensure that the progress seen in prostate cancer treatment is sustainable. By focusing on long-term effectiveness and personalized care, the medical community can build on current successes to shape therapies that are both safe and super important for patient well-being.
Comparing Real-World Outcomes: A Visual Overview
Sometimes, a clear picture is best illustrated with visual aids. The table below summarizes some of the key findings from the study and highlights how different drug classes perform in both clinical trials and real-world settings.
| Drug Class | Clinical Trial Efficacy | Real-World Outcomes | Key Observations |
|---|---|---|---|
| Androgen-Targeted Therapies | High efficacy with controlled protocols | Consistent tumor control with minimal surprises | Robust performance across varied populations |
| Radiopharmaceuticals | Effective in targeted radiation delivery | Enhanced benefits and improved quality of life | Focused treatment with manageable side effects |
| Immunotherapy | Mixed results due to variable immune responses | Similar or superior outcomes compared to trials | Potential for long-term remission in select cases |
This table helps underline the overarching theme: although each category of treatment has its own little twists and subtle parts, the general trend points to a positive translation from trial to real-world application.
Balancing Innovation with Caution in the Age of Personalized Medicine
The convergence of clinical trial evidence and real-world data is not the end of the story but rather a crucial chapter in the ongoing saga of personalized medicine. As groundbreaking treatments become the standard, clinicians must work through the small distinctions of individual patient responses to ensure the best care possible.
Innovations in targeted therapy are ushering in an era of precision medicine where therapies are designed with the patient’s unique genetic makeup and lifestyle in mind. However, this approach comes with its own set of challenging bits:
- Data Integration: Clinicians must weave together data from multiple sources—clinical trials, observational studies, and genetic assessments—to formulate optimal treatment plans.
- Individualized Monitoring: Even when a drug performs well on average, there may be hidden complexities in how different patients experience side effects or therapeutic benefits.
- Adapting to Diversity: As more diverse patient populations are included in studies, healthcare providers need to be mindful of subtle variations in drug metabolism and response.
By taking a cautious yet progressive approach, the medical community can figure a path that maximizes innovation while ensuring patient safety. It might be a bit intimidating to balance these aspects, but the emerging evidence from real-world studies offers reassurance that a thoughtful, data-driven approach is paying off.
The Role of Technology and Data Analytics in Enhancing Prostate Cancer Care
Modern technology and enhanced data analytics are playing an ever-increasing role in bridging the gap between clinical research and real-world practice. With the advent of big data, electronic health records, and real-time monitoring, clinicians now have tools that allow them to fine-tune treatments based on continuously updated information.
Key advancements include:
- Enhanced Data Collection: Digital health platforms allow for continuous monitoring of patient outcomes, ensuring that even the little twists in a patient’s response are captured and addressed.
- Predictive Analytics: Machine learning models are now being used to predict which patients are most likely to benefit from specific therapies, thereby steering through the complex bits of personalized care.
- Telemedicine Integration: Especially following lessons learned during the COVID-19 pandemic, remote monitoring and telehealth services have become an essential part of managing prostate cancer care.
This surge in technological integration not only makes it easier to track treatment success over long periods but also empowers patients to actively participate in their own care. It creates a feedback loop where both clinicians and patients benefit from timely, personalized data—making the treatment path less confusing and more supportive.
Patient Empowerment and Shared Decision-Making
In today’s evolving healthcare landscape, empowering patients has become a super important part of achieving successful outcomes. Understanding that clinical trials and real-world evidence are complementary rather than contradictory allows for a more transparent conversation between physicians and patients.
Elements that facilitate patient empowerment include:
- Clear Communication: Physicians can use real-world data to help explain treatment options in a way that’s digestible, easing the overwhelming nature of complex medical jargon.
- Shared Decision-Making: By actively involving patients in the treatment planning process, clinicians ensure that care is tailored to the individual’s unique needs and circumstances.
- Access to Information: With a growing repository of real-world studies and digital health records, patients can stay informed about the latest developments, making the overall journey less intimidating.
This collaborative approach not only enhances the trust between patient and provider but also ensures that treatment choices are made with a full understanding of both the expected benefits and potential risks. In turn, this encourages adherence to therapy and improves long-term outcomes.
Conclusion: A Promising Horizon for Prostate Cancer Therapies
As we wrap up this discussion, one thing is clear: the evolving landscape of prostate cancer treatment is characterized by both excitement and careful assessment. The current evidence, which supports that clinical trials can broadly predict real-world benefits, is a promising sign that the future of prostate cancer therapy is on a strong footing.
While there remain a number of twisted issues and challenging parts—ranging from statistical study designs to the hidden complexities of individual patient responses—the overall trend is optimistic. The convergence of solid clinical trial design with robust real-world data reiterates a message of hope and progress. Innovative therapies, when backed by detailed long-term data, can be safely integrated into routine clinical practice, giving both clinicians and patients a roadmap for managing prostate cancer with greater confidence.
Moreover, the integration of modern technology, an emphasis on alternative and supportive therapies, and a renewed focus on patient-centered care collectively ensure that the advances in prostate cancer treatment are not only scientifically sound but also practically effective. By staying attuned to the subtle details and small distinctions that define individual experiences, the medical community is better equipped to figure a path through the nerve-racking journey of cancer care.
The road ahead does involve navigating some tangled issues and coping with the intimidating wait for long-term results. Nonetheless, the research indicates that, with every new drug and each innovative mechanism, there is a measurable positive impact that transcends the controlled settings of clinical trials. As we continue to monitor and refine these therapies, the ultimate goal remains clear: to provide safer, more effective, and highly personalized care for every patient battling prostate cancer.
This blend of rigorous research, state-of-the-art technology, and compassionate patient care forms the cornerstone of modern oncology. With every study published and every new piece of real-world data analyzed, we are one step closer to transforming the tricky parts of prostate cancer treatment into a success story of innovation, resilience, and hope.
In closing, while no study can ever capture every twist and turn of real-life medicine, the substantial agreement between clinical trial data and real-world outcomes is a critical milestone. It reassures us that the framework we have built for prostate cancer therapy is not only scientifically robust but also practically reliable. As we continue to take a closer look at emerging therapies and refine our approaches, it is essential to keep the patient at the center of all decision-making.
The road may be full of confusing bits and little details that make standardization challenging, but the evidence brings a fair level of certainty when it comes to the performance of proven therapies. Ultimately, this alignment between clinical trials and everyday results helps to demystify cancer treatment, fostering an environment where the future of cancer care is both bright and compassionate.
Looking forward, continued collaboration among clinicians, researchers, policy makers, and patients will be the super important ingredient for success. By maintaining our focus on real-world evidence and adapting our protocols to address every nuance, the journey to improved outcomes for those with prostate cancer is well underway.
In this era of rapid advancements, the dialogue between trial data and practical experience will remain central to the conversation about improving lives. It is our shared responsibility to ensure that the gains made in research are fully translated into accessible, effective, and supportive treatments for all patients. This is not just the promise of modern medicine—it is a call to action for a healthier, more informed future.
Originally Post From https://www.urologytimes.com/view/study-results-affirm-effectiveness-of-evolving-prostate-cancer-therapies
Read more about this topic at
Real-World Evidence: A Primer – PMC
Real-world effectiveness of lenvatinib monotherapy among …