The Dawn of AI in Prostate Cancer Care: A New Era in Diagnosis and Treatment
The rapid evolution of artificial intelligence (AI) in modern healthcare is opening a remarkable new chapter in the fight against prostate cancer. Once considered an intimidating and off-putting challenge due to the tangled issues associated with early detection and treatment planning, prostate cancer care is now experiencing a transformation, thanks in large part to the innovative application of AI. This opinion editorial takes a closer look at the enormous potential of AI in prostate cancer diagnosis and treatment planning, while also probing into some of the more confusing bits of its integration into the conventional healthcare system.
As clinicians, researchers, and healthcare administrators work together to figure a path through these new developments, there is a growing consensus that the integration of AI is not merely a passing trend but a pivotal factor in the evolution of personalized medicine. AI is steadily emerging, from its early days as a promising tool, to a key component that can enhance clinical capabilities and ultimately improve patient outcomes.
AI-Powered Diagnosis: Transforming Prostate Cancer Detection
One of the essential breakthroughs in the fight against prostate cancer is the incorporation of AI in the detection process. Advanced machine learning algorithms have been designed to analyze intricate imaging data and other diagnostic information with an accuracy that often surpasses conventional methods.
Furthermore, a prominent UCLA-led study demonstrated that AI could predict seminal vesicle invasion—a critical indicator of disease severity—thus helping to determine the aggressiveness of a patient’s condition. This breakthrough can be seen as following:
- Faster Detection: AI algorithms can examine medical images and detect subtle indicators of prostate cancer that might skip over human observation.
- Increased Accuracy: By learning from vast datasets, AI systems greatly improve the consistency and precision of diagnoses.
- Better Patient Outcomes: When diagnosis is achieved early and accurately, treatment can be more timely and effective.
These advances are not without their challenges. The tricky parts involve ensuring that the data used to train these algorithms are diverse and representative, so that the predictions are accurate across different patient populations. In addition, integrating these systems into standard clinical practices without disrupting the current workflow remains a complicated piece of the puzzle.
Personalized Treatment Strategies Enhanced by AI Insights
Beyond early detection, AI is playing an increasingly crucial role in crafting personalized treatment strategies. Clinicians are now looking at AI as a partner that helps them personalize treatment algorithms by taking into account the little details of each unique case, rather than solely relying on general clinical expertise.
Dr. Soroush Rais-Bahrami of Wake Forest University School of Medicine has remarked on how AI aids in personalizing both treatment options and patient counseling. AI systems do this by taking a closer look at patient profiles—including genetic markers, tumor characteristics, and even the individual’s lifestyle—to design treatment plans that are more effective and better tailored to the patient’s needs.
This method is particularly useful in managing the twists and turns associated with treatment selection. By relying on AI, clinicians can:
- Refine Treatment Plans: Use patient-specific data to sort out the best course of action from a wide array of possibilities.
- Plan Surgical Interventions: Integrate AI-powered imaging and robotic systems to improve the precision of surgery.
- Monitor Ongoing Therapy: Regularly adjust therapy based on new data and AI-driven predictions.
Although these advances have not eliminated all of the confusing bits that come with modern medicine, many experts believe that personalized AI-assisted treatment strategies are a must-have component of future prostate cancer care.
Addressing Data Privacy and Security Issues in AI Applications
While the incorporation of AI into prostate cancer care can revolutionize clinical outcomes, it is also loaded with issues regarding data privacy and security. The collection and processing of vast amounts of patient data are necessary for AI to learn and become accurate. However, ensuring that patient privacy is not compromised is a critical concern.
There are several measures that healthcare providers and AI developers are putting in place to protect patient data:
- Robust Encryption: All data transmitted and stored is highly encrypted to prevent unauthorized access.
- Strict Access Controls: Only selected professionals have access to sensitive patient data, ensuring that the information is used solely for its intended purpose.
- Regular Audits: Conducting routine audits helps in identifying any potential vulnerabilities early on.
The goal is to balance the need for state-of-the-art diagnostic and treatment planning tools with the responsibility of safeguarding sensitive personal data. As these systems become a core element of clinical practice, continuing to work through these nerve-racking issues is essential for maintaining trust between patients and healthcare providers.
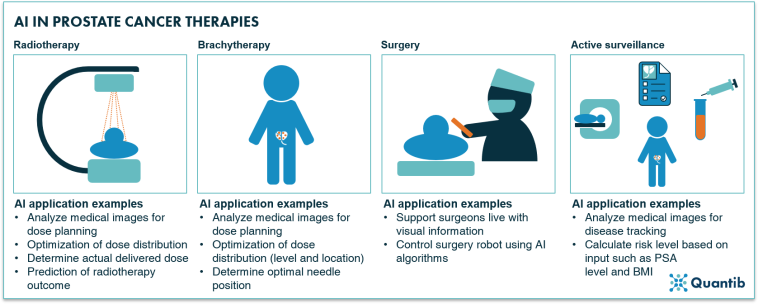
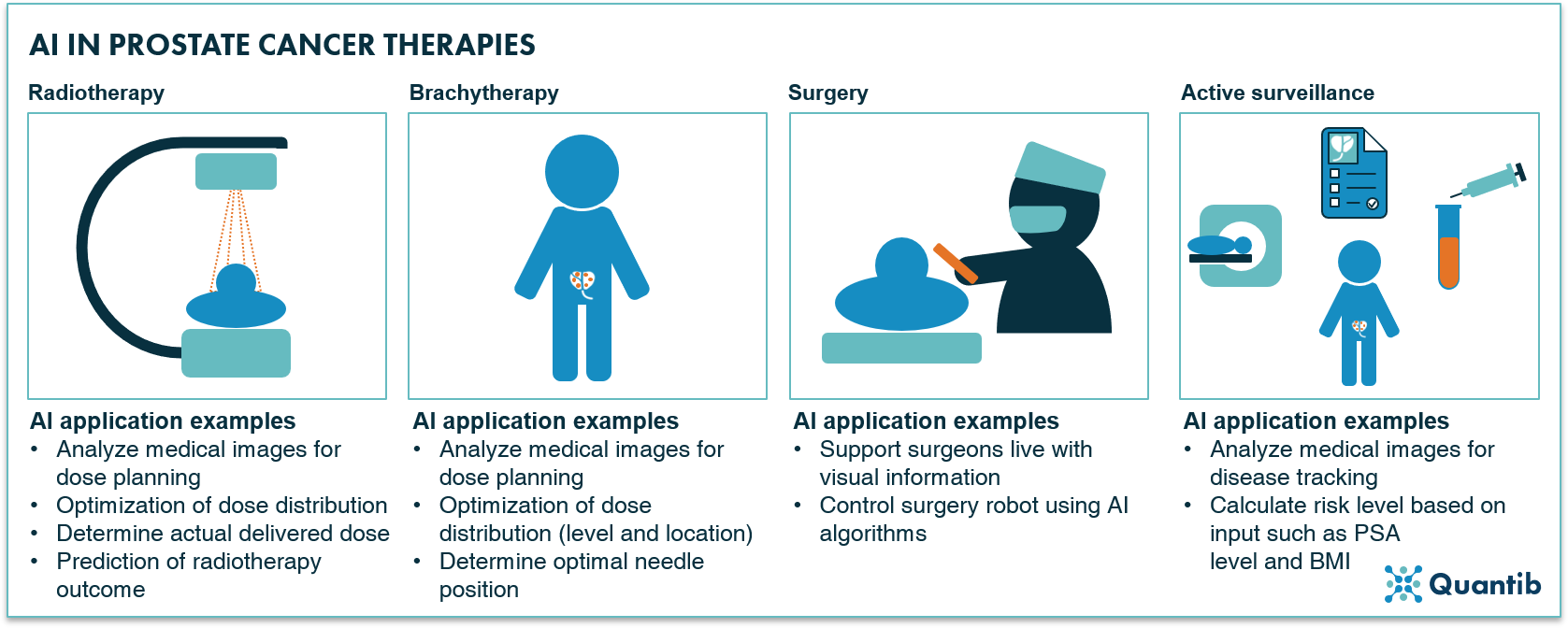
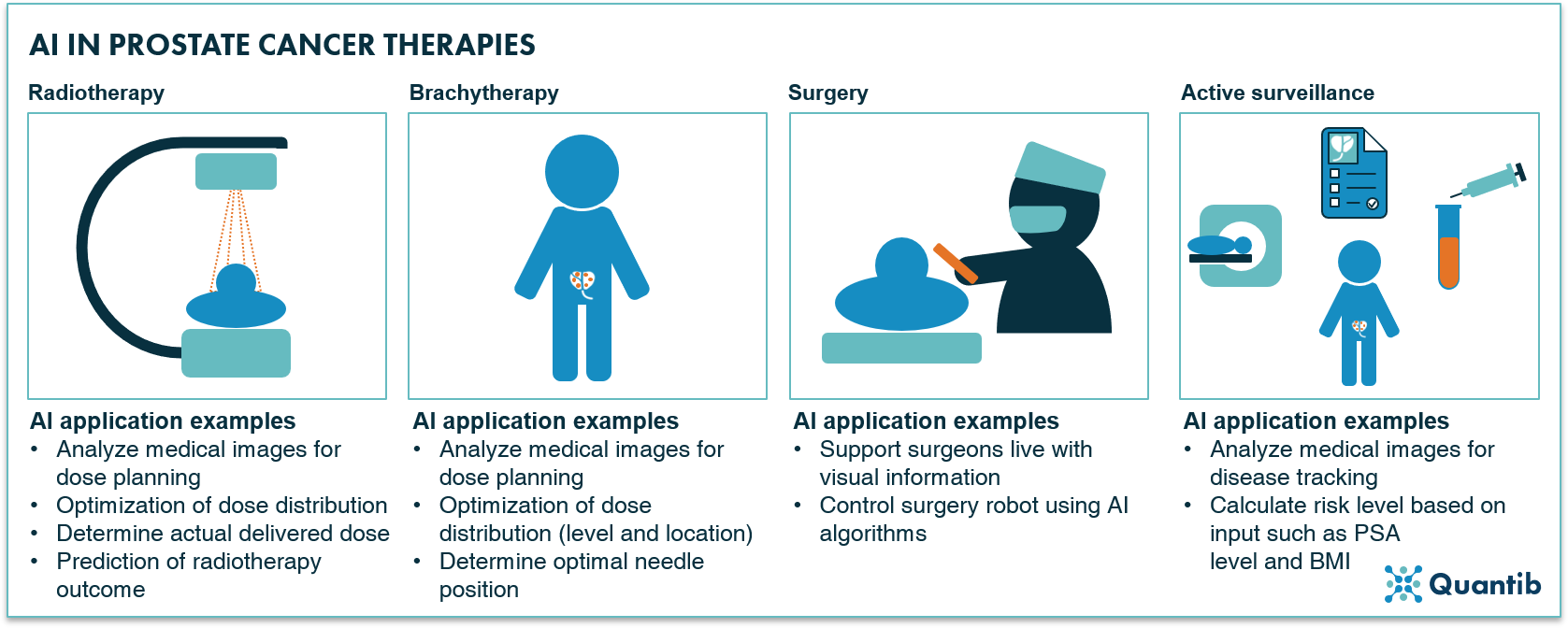
The Role of AI in Refining Surgical Precision and Robotic-Assisted Procedures
Surgical procedures have benefited enormously from the integration of AI, particularly when it comes to robotic-assisted surgeries. With prostate cancer operations considered as having many tricky parts, introducing AI into the surgical setting offers surgeons a sophisticated toolset for increasing precision.
Robotic surgery systems, which are now equipped with AI capabilities, help in honing surgical accuracy by providing real-time, data-driven feedback during an operation. These specialized systems assist in:
- Mapping Anatomy: AI-enhanced imaging tools help in identifying and preserving critical structures around the prostate.
- Targeting Tumors Accurately: By highlighting cancerous tissue, AI enables surgeons to remove tumors with greater certainty while minimizing collateral damage.
- Improving Recovery Rates: Enhanced precision in surgery can reduce complications and speed up recovery time.
Although it is not without its own set of confusing bits—as every new technology brings—this collaboration between human skill and machine precision is a promising indicator of the future direction of prostate cancer care.
Integrating AI into the Clinical Workflow: Overcoming the Tangled Issues
Even with all its evident benefits, AI integration into clinical workflows poses several challenges that are full of problems. Healthcare professionals need to balance between embracing cutting-edge technology and adapting to the tangible limitations of modern healthcare infrastructures.
Some of the key tangled issues include:
| Challenge | Potential Solutions |
|---|---|
| Data Standardization | Implementing industry-wide data formats and protocols can help ensure consistency. |
| Workflow Integration | Developing user-friendly interfaces that blend smoothly with existing clinical systems. |
| Training and Adoption | Offering comprehensive training programs and continuous support for healthcare staff. |
| Ethical Considerations | Establishing clear ethical guidelines regarding patient privacy and data usage. |
Addressing these tricky parts is critical, as the benefits of AI are only fully realized when the integration is as seamless and efficient as possible. This means not only investing in technology but also in training and support for clinicians who are tasked with using these novel systems daily.
Reflecting on Recent Clinical Trials and FDA Approvals in Genitourinary Cancers
While AI is reshaping prostate cancer care, it is also making its mark in other areas of genitourinary oncology. Recent clinical trials and FDA approvals are indicative of a broader trend toward personalized cancer therapy across various types.
An interesting case in point is the trial involving personalized therapeutic vaccines for kidney cancer. In this study, a subset of patients generated successful anticancer immune responses that kept them cancer free for approximately three years after treatment. Although this trial focused on kidney cancer, its implications are far-reaching, emphasizing the growing potential of personalized medicine—a goal that AI supports by offering precise diagnostic inputs and treatment suggestions.
Another noteworthy development discussed in leading conferences has been the FDA’s insights regarding muscle-invasive bladder cancer. Experts, like Dr. Chandler Park from Norton Cancer Institute, have pointed out that neoadjuvant and adjuvant therapies are becoming super important for adult patients dealing with this aggressive form of cancer. These therapies, increasingly aided by AI guidance, are transforming treatment plans by allowing a more tailored approach based on each patient’s specific condition.
The interplay between traditional clinical expertise and AI-driven data analysis is providing clinicians with a clearer, more detailed map of the cancer journey. Given these developments in the broader field of genitourinary cancers, it is not far-fetched to imagine that the experiences gained in one area might soon inform standards of care in another.
Enhancing Clinical Decision-Making with AI-Driven Data Analysis
Relying on AI’s capability to analyze extensive datasets, doctors can now work through the subtle details behind each clinical case. As AI tools digest and interpret data spanning imaging results, genetic profiles, and laboratory values, they offer clinicians a powerful means to figure a path through a maze of treatment alternatives.
This type of deep data analysis is proving especially helpful when it comes to handling the many twists and turns of treatment planning. For instance:
- Risk Assessment: By integrating patient history with current diagnostic data, AI helps estimate the risk of metastasis or disease recurrence.
- Tailoring Treatment: From hormone therapy to targeted interventions, AI can help fine-tune treatment modalities to match individual pathology.
- Predictive Analytics: Forecasting patient responses to different therapies, thereby enabling proactive treatment modifications.
The result is a more informed, data-backed approach that transforms decision-making from a process based solely on clinical judgment to one augmented by precise, algorithmic insights. This nuanced collaboration between technology and clinical experience is expected to continue evolving, offering a measure of reassurance in what once was considered a nerve-racking landscape.
Deliberating the Fine Points of Implementing AI in Everyday Clinical Practice
Implementing AI in daily medical practice involves not only the purchase of new software and equipment but also a fundamental shift in how clinical teams work. It means streamlining processes and making it easier to get around complicated pieces of regulatory and technical hurdles. Overcoming these challenges requires excellent communication, continuous training, and a deeper understanding of both the technology and its potential pitfalls.
Clinicians are beginning to observe some small distinctions as they integrate AI systems into their routines:
- Workflow Adaptation: The need to adjust clinical schedules and protocols to accommodate the system’s learning curve.
- Interdisciplinary Coordination: Collaboration between IT experts, data scientists, and healthcare professionals to resolve any technical glitches.
- Patient Communication: Explaining the role of AI in their care helps patients feel more comfortable and less overwhelmed by the technology.
This collaborative approach is not only making healthcare teams more resilient in the face of technological change but also fostering an environment where continuous improvement is part of the everyday workflow. In a field where every little twist can have significant implications, this process of working together on AI integration is a super important step in modernizing patient care.
Improving Patient Outcomes: The Real-World Impact of AI in Prostate Cancer Care
The ultimate measure of any technological innovation is its real-world impact on patient outcomes. Early evidence strongly suggests that AI is making a meaningful difference in improving survival rates and overall quality of life for men diagnosed with prostate cancer.
AI’s benefits in clinical settings include:
- Faster and More Accurate Diagnoses: Lowering the chances of misdiagnosis by identifying subtle abnormalities missed by standard screening methods.
- Optimized Treatment Plans: Allowing more proactive and tailored therapy that considers the patient’s overall clinical picture.
- Enhanced Monitoring and Follow-Up: Integrating data from continuous monitoring devices can alert clinicians to changes sooner than ever before.
Patients can thereby enjoy a clearer path toward recovery, with treatment strategies that are continuously refined as new data becomes available. The use of AI in this context is a shining example of how modern medicine adapts to leverage technology for tangible health benefits.
Charting the Future of AI in Prostate and Genitourinary Cancer Care
Looking ahead, the integration of AI is likely to extend much further into the realm of genitourinary oncology. While prostate cancer care currently leads the way, there is growing interest in applying AI techniques to other related cancers, such as kidney and bladder cancer. Combining insights gleaned from multiple clinical trials and early adoption of AI for surgical guidance, healthcare providers are on track to influence treatment plans across a variety of cancer types.
Some of the future directions anticipated include:
- Broader Integration with Personalized Medicine: As algorithms become more refined, every aspect—from risk assessment to treatment monitoring—will carry the distinctive advantage of a personalized approach.
- Enhanced Biopsy and Imaging Techniques: Future AI systems might further reduce the time needed for analyzing biopsy samples and imaging, delivering more precise results with fewer needle passes or invasive techniques.
- Real-Time Decision Support: Imagine an AI system that can update treatment options in real time as a patient’s response to therapy unfolds, ensuring that every decision made is as informed as possible.
These forward-looking strategies, while full of problems related to data privacy and the technical integration into everyday practice, also represent our best hope for improving patient outcomes. With each advance, clinicians are increasingly confident that AI will continue to yield a safer, more precise, and more personalized approach to cancer care.
Collaborative Efforts Between Clinicians, Technologists, and Researchers
The true success of AI in prostate cancer care hinges on a collaborative effort between various stakeholders. Surgeons, oncologists, data scientists, and IT professionals must work together to manage the many nerve-racking implementation challenges and ensure that the technology is both effective and secure.
Key areas of collaboration include:
- Data Sharing Protocols: Building secure frameworks for sharing clinical data that allow AI systems to learn without compromising privacy.
- Joint Training Programs: Designing training initiatives that help clinicians understand the capabilities, limitations, and optimal use cases of AI tools.
- Continuous Research and Feedback: Maintaining a loop of feedback from real-world clinical experiences that can be used to further refine AI algorithms.
By finding your way through these collaborative channels, the healthcare community is likely to see even more rapid progress in the application of AI, ensuring that technology serves as an effective partner in the ongoing fight against prostate and other genitourinary cancers.
Addressing Regulatory and Ethical Considerations in AI Adoption
Every significant shift in medical technology brings with it its own set of ethical and regulatory challenges. Although the benefits of AI in prostate cancer care are clear, embracing it on a large scale requires thorough consideration of regulations, including guidelines set out by agencies such as the FDA.
Some of the off-putting yet essential considerations include:
- Regulatory Approval Processes: Ensuring that AI algorithms meet high standards of safety and efficacy before they become a mainstream part of clinical practice.
- Ethical Consent and Transparency: Patients must be adequately informed about how AI systems are used in their treatment, as well as the right to opt out if they so choose.
- Long-Term Monitoring: Continuously gathering data on the outcomes from AI-assisted treatments to secure ongoing approvals and improve system performance.
By tackling these issues head on, healthcare providers can ensure that AI not only continues to be a game changer but does so in a manner that is both ethical and legally sound. This balanced approach is key to building lasting trust in AI-driven treatment methodologies.
Final Reflections: Embracing the Future of AI in Prostate Cancer Care
After surveying the current landscape and peeking into the future, it is apparent that AI is set to revolutionize how prostate cancer is understood and treated. The integration of advanced algorithms into everyday clinical practice is already lifting the burden associated with early, off-putting challenges and is showing tremendous promise in refining diagnosis, personalizing treatment, and ultimately enhancing patient outcomes.
The journey, however, is not without its confusing bits and overwhelming challenges. From data privacy concerns to the intricacies of integrating AI with existing systems, the path forward is one that demands careful thought, collaborative effort, and a commitment to continuous improvement.
Nonetheless, the potential benefits—faster diagnoses, more personalized treatment strategies, enhanced surgical precision, and better overall outcomes—speak to a future where cancer care is not merely reactive but proactive, tailored, and cutting-edge.
For patients, clinicians, and researchers alike, this new era of AI-powered prostate cancer care means working together to figure a path through these tangled issues and reaping the rewards of a technology that transforms uncertainty into opportunity. With ongoing research, regulatory support, and a collaborative spirit, the promise of AI in healthcare is both exciting and encouraging, offering hope where once there was apprehension.
As we continue to take a closer look at the role of AI in navigating the many challenges of modern cancer care, one thing remains clear: technology, when effectively integrated, does not replace the human touch but rather enhances it—making the mission to cure cancer a more attainable goal each day.
In conclusion, the revolution driven by AI in prostate cancer care is not just a technological upgrade—it is a comprehensive transformation that brings together the finest aspects of modern medicine, research, and personalized patient care. By embracing these advancements and working through the nerve-racking issues with a balanced and thoughtful approach, the healthcare community is setting the stage for a future where every patient can enjoy a more precise, effective, and reassuring journey through cancer care.
Let us remain hopeful and vigilant as we continue to watch this exciting field grow, ensuring that innovation always goes hand in hand with compassion, ethics, and the unwavering commitment to improving lives.
Originally Post From https://www.curetoday.com/view/the-dawn-of-ai-in-prostate-cancer-care
Read more about this topic at
This New Treatment Is Transforming Prostate Cancer Care
‘Life-Changing’ New Treatment for Enlarged Prostate