Editorial Overview: Transforming B-Cell Malignancy Treatment Paradigms
The landscape of B-cell malignancy treatment is undergoing a marked transformation, driven by the emergence of targeted, chemo-free, and cellular therapies. Recent developments in mantle cell lymphoma (MCL), diffuse large B-cell lymphoma (DLBCL), and chronic lymphocytic leukemia (CLL) have sparked widespread discussion among healthcare professionals. In this opinion editorial, we take a closer look at the latest advances and the debates that are shaping the future of therapies for these challenging conditions. We will explore how contemporary research, clinical trials, and new drug combinations aim to address the tricky parts of traditional treatment while striving to minimize side effects and improve patient outcomes.
For many years, chemoimmunotherapy combined with autologous stem cell transplant (ASCT) has been a mainstay treatment for conditions like MCL. However, with the rise of chemo-free regimens—based on targeted therapies and cellular interventions—the traditional treatment blueprint is steadily being reimagined. Even as the oncology community embraces these new strategies, discussions continue about the optimal selection, sequencing, and combinations of therapies to address the tangled issues posed by high-risk disease features.
Emerging Chemo-Free Approaches in Mantle Cell Lymphoma
Novel regimens have begun moving into the spotlight for the treatment of mantle cell lymphoma. Historically, chemoimmunotherapy has been the default approach, but recent evidence is building a case for the benefits of abandoning traditional chemotherapy in favor of more tailored therapeutic combinations.
Shifting from Traditional Chemoimmunotherapy
The long-standing reliance on chemoimmunotherapy, often supplemented by ASCT, is being questioned by emerging data from phase 3 studies like TRIANGLE and ENRICH. These studies have provided evidence suggesting that chemo-free regimens—especially those based on BTK (Bruton’s tyrosine kinase) inhibitors—could potentially improve patient outcomes without the added toxicity inherent in chemotherapy.
Key points include:
- Chemo-free regimens offer an alternative for patients who are less likely to tolerate conventional chemotherapy.
- BTK inhibitors such as ibrutinib, acalabrutinib, and zanubrutinib are increasingly being recognized as key players outside of the traditional R-CHOP regimen.
- For patients with difficult-to-treat MCL, particularly those with high-risk features like TP53 mutations, chemotherapy may exacerbate chromosomal instability, so maintaining a chemotherapy-free approach could prove to be safer.
Advantages and Considerations of BTK Inhibitor Use
The adoption of BTK inhibitor–based regimens in frontline settings has been marked by both enthusiasm and caution. While these agents have shown promising efficacy, their performance compared to traditional combinations is still under observation in ongoing clinical trials. The shift to BTK inhibitors highlights several essential considerations:
- Treatment Suitability: Some patients, particularly those with TP53 abnormalities, may not respond well to standard chemotherapy, making targeted treatments more attractive.
- Study Limitations: Although randomized studies have shown that agents such as zanubrutinib may outperform older drugs like ibrutinib in specific scenarios, comparisons often reveal only modest differences when multiple chemoimmunotherapy regimens are considered.
- Combination Therapies: Emerging regimens include combining BTK inhibitors with agents like venetoclax and monoclonal antibodies such as obinutuzumab, which aim to exploit synergistic effects and improve overall efficacy.
Refining Treatment Strategies in Chronic Lymphocytic Leukemia (CLL)
In chronic lymphocytic leukemia, the treatment paradigm has shifted dramatically over the past decade, moving away from the chemoimmunotherapy model toward a reliance on time-limited regimens and targeted mono-therapy.
Transitioning from Chemoimmunotherapy to Targeted Agents
Decades ago, CLL treatment predominantly involved chemoimmunotherapy, which offered moderate success but at the cost of significant side effects. Today, the options are much more diversified. The introduction of venetoclax combined with obinutuzumab and the use of single-agent BTK inhibitors reflect this significant progress. The community is already witnessing that the use of traditional chemotherapy is becoming increasingly rare in the frontline setting for CLL.
Clinicians are now faced with several critical decisions when choosing the best path for each patient. The primary considerations include:
- The choice between time-limited combinations versus continuous single-agent therapy.
- The effectiveness and safety profiles of different BTK inhibitors.
- The potential to integrate emerging combinations that include novel agents alongside established therapies.
Understanding the Role of Combination Regimens
Combination therapies are helping clinicians manage the subtle parts and little details of treatment response. For example, experiences with regimens that pair acalabrutinib with venetoclax—and sometimes include obinutuzumab—are changing the way physicians approach frontline therapy in CLL. These regimens aim to harness the strengths of both cellular targeting and pathway inhibition.
In practice, the following aspects are particularly important:
- Time-Limited Therapy: Patients may benefit from shorter, more intense treatment courses that help reduce long-term exposure to drugs and potentially minimize side effects.
- Improved Efficacy: Clinical trial data suggest that a combination of targeted agents may yield better survival outcomes compared to monotherapy, though ongoing studies are needed to validate these findings in broader populations.
- Side Effect Management: Balancing the benefits with the potential issues—such as cardiovascular events or other adverse reactions—is essential, as the switch to targeted therapies brings its own set of challenges.
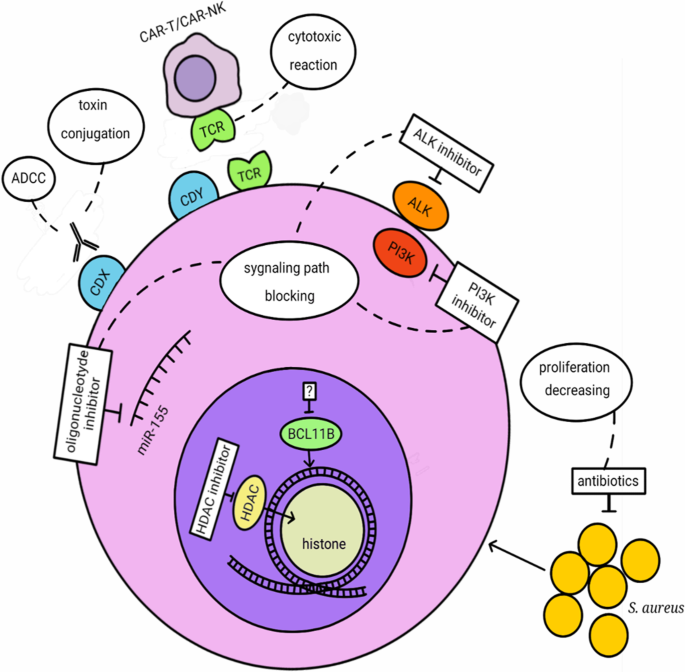
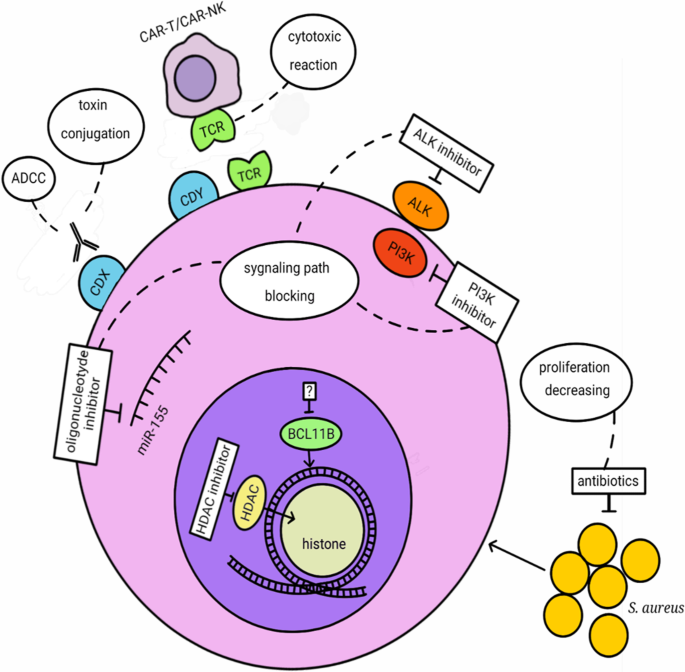
CAR T-Cell Therapies and Their Impact on Double-Refractory CLL
The recent FDA approval of lisocabtagene maraleucel (liso-cel) has added a new tool to the arsenal for treating double-refractory CLL. These are patients who have already proven resistant to both BTK inhibitors and BCL2 inhibitors like venetoclax.
Integration of Cellular Therapies in Clinical Practice
Cellular therapies, particularly CAR T-cell treatments, have long been a subject of intense research in hematologic malignancies. With liso-cel now approved, clinicians are exploring its role as a potential intervention for patients who have exhausted conventional treatments. However, using CAR T-cell therapies comes with its share of tricky parts:
- Safety Concerns: Some of the more intimidating issues include cytokine release syndrome (CRS), neurotoxic effects, and the potential for infections following treatment.
- Patient Selection: Not every patient is a candidate for such treatments. Historically, those who have undergone multiple lines of chemotherapy may have compromised immune systems, which could affect both the efficacy and safety of CAR T-cell interventions.
- Treatment Timing: Using CAR T-cell therapy earlier in the disease course could potentially result in better outcomes, as patients’ overall health might be more robust, leading to improved durability and fewer complications.
Comparing CAR T-Cell Therapy with Non-Covalent BTK Inhibitors
In the current treatment landscape for double-refractory CLL, non-covalent BTK inhibitors like pirtobrutinib remain an important consideration for doctors. Although pirtobrutinib has shown promise as an immediate option during periods of symptom management, its ability to offer a long-term cure remains uncertain—making CAR T-cell therapies an appealing option for certain patients.
The future appears promising as researchers continue to explore strategies to mitigate the side effects of CAR T-cell therapies while boosting their efficacy. For example:
- Some combination strategies pair CAR T-cell therapy with BTK inhibitors, potentially enhancing the overall therapeutic effect while easing side effect profiles.
- Preclinical studies and early-stage clinical trials are actively investigating methods to limit adverse events and to improve patients’ immune responses post-treatment.
Clinical Trials: The Cornerstone of Advancing Therapy
One undeniable theme in the evolving treatment paradigm is the critical role of clinical trials. These studies provide invaluable insights into the subtle details of the fine points of disease management in B-cell malignancies. With the experimental landscape continuously evolving, clinical trials serve as the proving ground where innovative ideas are tested and refined.
Understanding Trial Designs and Their Impact
Clinical trials such as the phase 1/2 and phase 3 studies are crucial for building robust evidence about the efficacy and safety of chemotherapy-free and targeted regimens. Researchers and clinicians rely on these studies to figure a path through the confusing bits and nerve-racking uncertainties that arise when introducing any new treatment method.
Some of the trial designs that have had a major impact include:
| Study Name | Phase | Focus | Notable Findings |
|---|---|---|---|
| TRIANGLE | Phase 3 | MCL Chemo-Free Regimens | Demonstrated efficacy of chemoimmunotherapy-free approaches |
| ENRICH | Phase 3 | Comparison of Ibrutinib-Based vs. Chemoimmunotherapy | Highlighted benefits in specific control arms but also revealed modest differences |
| TRANSCEND CLL 004 | Phase 1/2 | CAR T-Cell Therapy in CLL | Provided initial insights into safety and effectiveness, albeit in heavily pretreated patients |
Benefits of Innovative Therapeutic Combinations in Trial Settings
Combining targeted agents in clinical trials helps to unpack the twisted issues inherent in treating B-cell malignancies. For instance, studies that incorporate a mix of BTK inhibitors, BCL2 inhibitors, and monoclonal antibodies are now offering hope for more effective and personalized therapies. Results from these trials are crucial for:
- Establishing standardized treatment protocols that reduce reliance on toxic chemotherapies
- Explaining the hidden complexities of treatment resistance and how to overcome them
- Providing data for regulatory approval and clinical guideline updates
Dealing with the Tricky Parts of Adopting New Therapeutic Protocols
The journey to implementing these novel treatments is far from straightforward. Physicians and care teams must work through a myriad of confusing bits and nerve-racking challenges when integrating new protocols into everyday practice. Given the constantly shifting narrative in oncology, certain key considerations remain front and center:
Managing Treatment Selection in High-Risk MCL
For high-risk mantle cell lymphoma patients, the decision-making process is loaded with challenges. Many experts argue that patients with high-risk features—such as TP53 mutations—should be steered away from conventional chemoimmunotherapy. Instead, these patients might be better served by enrolling in clinical trials or opting for regimens that combine novel targeted agents.
Key factors to consider include:
- Risk of Chromosomal Instability: Chemotherapy, while effective in many cases, can sometimes spur additional genetic mutations, a particularly worrying prospect for patients with genetically unstable tumors.
- Access to Trials: Not all treatment centers have equal access to innovative clinical trials. However, centers with robust research programs are often at the forefront of offering life-changing therapeutic alternatives.
- Individual Patient Profiles: Decisions must be personalized, considering both the patient’s overall health and the specific characteristics of their malignancy.
Optimizing BTK Inhibitor Use in CLL Regimens
In CLL, the evolution toward targeted therapies means that BTK inhibitors have become a critical pillar of treatment strategy. With three different agents currently approved—ibrutinib, acalabrutinib, and zanubrutinib—the choice often hinges on subtle differences in efficacy and safety profiles.
Points to keep in mind include:
- Selective Inhibition: Newer agents like acalabrutinib and zanubrutinib offer more selective inhibition, potentially reducing off-target effects and making it easier for patients to tolerate long-term treatment.
- Comparative Efficacy: Randomized study data suggest that while ibrutinib is still used, its role is diminishing in favor of agents with better performance metrics. Data from head-to-head studies are increasingly steering prescribers towards the latter.
- Combination Strategies: Emerging studies that pair BTK inhibitors with agents such as venetoclax are promising. Early results hint at improved outcomes when these drugs are deployed together rather than alone.
Addressing the Challenges of an Expanding Therapeutic Armamentarium
The modern oncology field is witnessing an explosion in treatment options for B-cell malignancies, yet this burgeoning variety brings its own set of tangled issues and daunting decisions. Both clinicians and patients are navigating a treatment landscape where every new agent or combination protocol must be balanced against potential side effects and long-term outcomes.
The Role of Multidisciplinary Collaboration
Given the nerve-racking nature of the evolving treatment scene, one of the best ways to figure a path through these challenges is via multidisciplinary collaboration. Oncologists, hematologists, clinical trial specialists, and supportive care providers must come together to discuss and analyze:
- Patient-Centric Treatment Plans: How best to integrate new therapies in a way that maximizes quality of life while maintaining disease control.
- Managing Side Effects: Understanding and pre-emptively treating adverse reactions, from CRS in CAR T-cell therapies to cardiovascular effects in BTK inhibitor use.
- Future Research Directions: Identification of areas where current treatments fall short, such as for patients with double-refractory disease or with specific genetic instabilities, to inform future clinical trial design.
Educational Initiatives and Patient Outreach
As treatment protocols become more complex, both the medical community and patients alike need resources to help make informed decisions. Educational initiatives that dissect the fine shades of new therapies can be extraordinarily helpful. These initiatives aim to:
- Explain the subtle details behind treatment choice and sequencing.
- Offer updated, accessible data on the latest clinical trial findings.
- Provide clear guidance on managing side effects and expectations regarding treatment outcomes.
Such efforts are essential for ensuring that both clinicians and patients feel empowered to make well-informed decisions, even as the treatment landscape continues to evolve with unforeseen twists and turns.
Future Directions: Where Do We Go From Here?
Looking ahead, the future of B-cell malignancy treatment is full of promise, yet it is also packed with many challenges that require ongoing vigilance. As our understanding deepens through clinical trials and real-world evidence, there is optimism that therapies will be even more personalized, with decisions tailored to individual genetic profiles and disease characteristics.
The Promise of Personalized Medicine
Personalized medicine is emerging as a super important aspect of cancer care. In B-cell malignancies, where each patient’s disease can show small distinctions, a one-size-fits-all approach is clearly not ideal. Instead, the future will likely involve:
- Genetic Profiling: Enhanced molecular diagnostics will allow for the selection of therapies that are best suited to the patient’s specific genetic makeup, whether that involves targeted inhibitors, immunotherapy, or cellular therapies.
- Adaptive Trial Designs: Innovative trial designs that respond in real time to patient responses offer the potential for more dynamic treatment planning, with adjustments made as new data comes in.
- Combination Therapies: The blending of targeted agents with immunotherapy or even cellular approaches is expected to yield synergies that further improve patient outcomes.
Strategies for Reducing Treatment-Related Risks
Reducing the risks associated with new treatments, particularly in vulnerable patient populations, remains a critical focus. As the use of cellular therapies and targeted agents becomes more widespread, strategies to minimize side effects will include:
- Prophylactic Measures: Implementation of preventive measures to reduce risks such as CRS and neurotoxic effects associated with CAR T-cell therapy.
- Combination Approaches: Pairing agents in ways that allow overlapping toxicities to be managed more effectively, ensuring a smoother treatment course for patients.
- Enhanced Monitoring: The use of advanced monitoring technologies and biomarkers to quickly assess treatment response and prompt early intervention when side effects occur.
Conclusion: Working Through the Twists and Turns of B-Cell Malignancy Treatment
The evolving treatment landscape for B-cell malignancies offers hope for patients and their families, even as the path forward is full of tangled issues and intimidating decisions. The contemporary shift away from traditional chemotherapy towards targeted, chemo-free, and cellular therapies represents a significant milestone in modern medicine. As clinical trials continue to refine these approaches and as multidisciplinary teams work together to customize treatment plans, the future looks super important for the advancement of personalized cancer care.
Physicians, researchers, and healthcare providers must continue to figure a path amid the nerve-racking challenges of integrating emerging therapies. Each new study and every clinical trial result provides essential information that helps build a more complete picture of the risks and rewards associated with these innovative treatments.
In a field where minute details can mean the difference between success and setbacks, it is the collaborative effort of the global oncology community that will ultimately shape the best paths forward. Through rigorous clinical research, ongoing education, and direct patient engagement, the complex pieces of B-cell malignancy care will gradually come together into a coherent, patient-focused treatment paradigm.
As we look ahead, embracing these novel therapeutic strategies while continuing to thoughtfully assess their real-world impact will be a critical part of advancing cancer care. The goal remains clear: to offer patients safer, more effective treatment options that not only prolong survival but also improve quality of life. In this era of rapidly evolving cancer care, it is the determination to work through every twist and turn—no matter how intimidating—that will ultimately lead to a brighter future for those facing B-cell malignancies.
Ultimately, the promise of these emerging therapies lies in their potential to redefine what is achievable in cancer treatment today. By staying at the forefront of research and continuing to learn from every clinical experience, the oncology community can remain agile in the face of change. The hurdles ahead are many, but the collective expertise and dedication within the field provide strong reasons to be hopeful. As more innovative treatments become available, the ongoing discussions, studies, and patient outcomes will continue to shape the future of B-cell malignancy treatment in profoundly positive ways.
In closing, while the journey toward fully chemo-free and personalized therapy regimens is still ongoing, recent breakthroughs have opened up a new chapter in cancer care. It is our responsibility—as clinicians, researchers, and patients—to embrace these changes with the open-minded curiosity needed to conquer the troubled bits of traditional therapy. With a keen eye on future developments and a commitment to data-driven care, the oncology community is well positioned to redefine success in the fight against B-cell malignancies.
As this evolving story unfolds, one thing remains certain: the era of personalized, targeted cancer therapy is here, and it is transforming not merely the way we treat cancer, but the very nature of hope in modern medicine.
Originally Post From https://www.onclive.com/view/novel-targeted-chemo-free-and-cellular-therapies-are-poised-to-transform-treatment-paradigms-in-b-cell-malignancies
Read more about this topic at
unleashing the potential of B cell-derived exosomes
Revolutionizing cancer treatment: the emerging potential …