Reduced Opioid Prescribing and the Rising Pain Crises in Advanced Cancer: An Opinion Editorial
The shifting landscape of pain management in advanced cancer has emerged as a topic loaded with issues for patients, clinicians, and policymakers alike. Recent study findings suggest that the well-meaning efforts to curb opioid overprescribing may be accompanied by unintended consequences for older adults living with metastatic cancer. In this editorial, we take a closer look at the evolving policies, the tricky parts of pain treatment, and the need for a balanced approach that not only addresses drug misuse concerns but also ensures effective pain relief.
Impact of Reduced Opioid Prescription Guidelines on Advanced Cancer
Understanding the Shifts in Pain Management Approaches
The study under discussion analyzed a broad range of data from Medicare enrollees between 2012 and 2017, comparing patients with metastatic solid tumors to control patients without cancer. The results point to a modest drop in opioid prescriptions, compensated by a rise in the use of gabapentinoids, yet simultaneously showing a rise in emergency department visits and opioid-related encounters among advanced cancer patients. These results ask us to figure a path through the twists and turns of modern pain management strategies.
While regulatory measures were designed to tackle opioid misuse, they have also inadvertently affected those in dire need of pain relief. With the emphasis shifting from a simple reduction in opioids to a cautious management of all analgesic strategies, the consequences are anything but straightforward. Increased reliance on alternatives like gabapentinoids and the mix of patient-specific factors have generated a scenario that is both nerve-racking and on edge.
Tricky Parts of Regulating Pain Treatments in Advanced Cancer
One cannot ignore the tangle of issues that arise when policy meets practice. Clinicians now have to balance the drive to reduce opioid prescriptions with the pressing need to provide adequate pain control to advanced cancer patients. This balancing act is further complicated by several factors:
- Older patients may have multiple comorbid conditions that require careful pain management.
- The stigma surrounding opioids forces many patients and providers to question whether reducing prescriptions might worsening pain crises.
- The increasing use of alternatives such as gabapentinoids has yet to be fully understood in terms of long-term effectiveness and potential side effects.
- Regulatory pressures mean that clinicians face additional administrative tasks, making it tougher to find your way through the subtle parts of individual patient needs.
These issues are not merely academic. They involve everyday decisions made by providers who must contend with both the little details of patient care and the broader regulatory framework, which sometimes seems more on edge than supportive.
Consequences of Modified Opioid Prescribing Policies
Emergency Department Visits and Their Implications
A striking finding from the study was the significant increase in pain-related emergency department (ED) visits among advanced cancer patients. This rise in ED visits—from 23.3% to 29.0% over the study period—highlights the unintended results of decreasing opioid availability. For patients already grappling with overwhelming pain, having to seek emergency care can be both intimidating and off-putting.
ED visits for pain-related issues not only indicate gaps in effective outpatient pain management but also lead to a cascade of further complications. Short-term fixes provided in emergency settings rarely substitute the cumulative need for sustained pain control. This situation raises several questions for healthcare providers and policymakers:
- Are current dosing guidelines and restrictions too rigid for the unique needs of cancer patients?
- How does the stress of using emergency services affect the overall well-being of those already coping with advanced disease?
- Would a more patient-centered approach, which considers the individual’s history of opioid use and pain severity, lead to better outcomes?
When emergency services become a crutch rather than a temporary solution, it is clear that the current policies might need rethinking. Instead of a one-size-fits-all approach, the situation calls for nuanced guidelines that are capable of adapting to the fine shades of pain management in advanced cancer care.
Increased Opioid-Related Encounters in a Shifting Prescribing Landscape
The study also demonstrated a sixfold increase in opioid-related encounters—from 0.7% to 4.2%—among advanced cancer patients. These encounters include adverse events and complications arising from opioid use, which may be partly linked to lower availability and, consequently, the risky use of accumulated or non-prescribed doses.
It is crucial to remember that while opioids have their own set of tricky parts, they remain an essential component of pain management for many patients with metastatic cancer. The increased encounters could be a byproduct of patients trying to achieve adequate pain relief in the face of regulatory hurdles. This raises several notable points:
- The shift towards controlled opioid use can leave patients with no viable alternative for managing severe pain.
- Healthcare providers might be forced to prescribe opioids in a reactive way—only after a crisis has occurred, rather than in a controlled, monitored manner.
- Poor communication between patients and providers about pain management goals can contribute to inconsistencies in opioid use and monitoring.
This scenario underscores the need for improved mechanisms to track and manage opioid use in a way that both reduces misuse and ensures patient comfort. The delicate balance demanded here requires stakeholders to carefully figure a path that ensures patient safety without sacrificing pain relief.
Subgroup Disparities: Racial and Socioeconomic Factors
An additional layer of complexity emerges when examining racial and socioeconomic factors. The study found that Black patients and those with bone metastases experienced disproportionately higher increases in both pain-related ED visits and opioid-related encounters. These imbalances are small distinctions that point towards broader systemic issues in healthcare delivery.
Several factors could be contributing to these disparities:
| Factor | Potential Impact |
|---|---|
| Socioeconomic Status | Patients in lower income areas may have less access to comprehensive pain management clinics. |
| Racial Bias | Historical and ongoing racial disparities may result in undertreatment of pain in Black patients. |
| Coexisting Conditions | Higher rates of comorbid conditions can complicate pain management strategies. |
| Provider Communication | Lack of culturally sensitive communication can exacerbate the fine points of treatment planning. |
Addressing these subtle details is super important. Healthcare systems need to work on strategies that reduce such disparities while maintaining a high standard of care for every patient, regardless of background or income level. Only then can we hope to usher in a more equitable era in pain management for advanced cancer.
Balancing Safety and Effective Pain Relief
Opioid Analgesics in the Context of Advanced Cancer
Opioid analgesics have long been the mainstay for treating severe pain in advanced cancer. Despite the alarming potential for misuse and the various tangled issues associated with opioids, they remain a cornerstone of effective pain relief. The recent decreases in opioid prescriptions have resulted in growing concerns about whether patients are receiving the pain management they need.
In evaluating these treatment options, several key factors come into play:
- Patient History: Prior opioid use and history of pain management are critical data points that should influence prescribing decisions.
- Individual Needs: Advanced cancer patients tend to have multifaceted pain requirements that might not be met by substituting opioids with a single alternative.
- Safety Profiles: While gabapentinoids offer another route, there remains uncertainty about their long-term effectiveness compared to opioids.
These points emphasize that the reduction in opioid use is not solely a matter of statistics but a reflection of the complicated pieces of each patient’s journey through advanced illness. Effective pain management in this group is as critical as it is challenging, and the need for individualized care has never been more clear.
Alternative Pain Management Strategies for Advanced Cancer
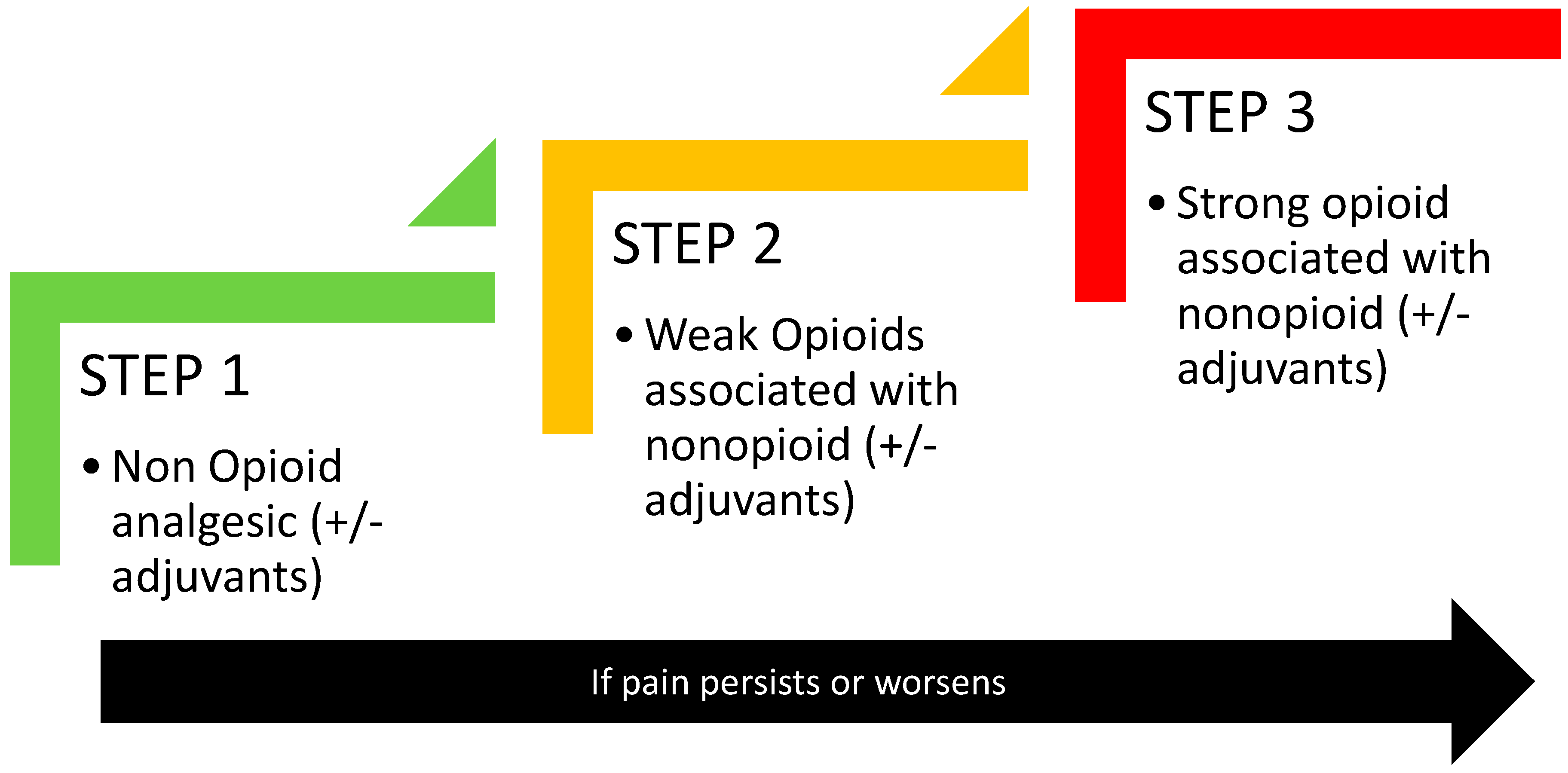
In light of regulatory pressures and the ongoing risk of opioid misuse, alternative pain management strategies have gained traction. These alternatives range from non-opioid medications to complementary therapies, and they come with their own set of benefits and tricky parts.
Some of the popular alternatives include:
- Gabapentinoids: As reported in the study, there has been a noted increase in gabapentinoid use. These drugs can help manage nerve-based pain but might not be suitable for all patients.
- Non-steroidal Anti-inflammatory Drugs (NSAIDs): Widely used for mild to moderate pain, NSAIDs can sometimes fill the gap left by reduced opioid prescriptions, though their effectiveness in severe cancer pain is limited.
- Complementary and Alternative Medicine (CAM): Techniques such as acupuncture, mindfulness, and physical therapy can provide supportive care for patients, especially when traditional pharmacotherapy falls short.
- Interventional Procedures: Nerve blocks and other procedures may offer targeted pain relief, reducing the overall need for systemic medications.
Each of these alternatives has its own set of subtle parts and requires careful integration into the overall treatment plan. The right balance is crucial, as what works for one patient might not be the answer for another. Integrating alternative treatments demands input from multidisciplinary teams who can work together to figure a path that meets the individual needs of advanced cancer patients.
Policy Considerations and Future Research
Fine Points in Policy Making and Regulatory Oversight
Policy decisions surrounding opioid prescribing have long been under the microscope. Recent trends indicate that well-intentioned regulations have created an environment that inadvertently strains the delicate balance between safety and symptomatic relief. The current regulatory framework is full of problems and likely needs refining to better serve the population of advanced cancer patients.
There are several policy considerations to keep in mind:
- Flexibility in Guidelines: Current prescribing guidelines could benefit from built-in flexibilities that recognize the unique pain challenges faced by cancer patients.
- Enhanced Monitoring: Expanding monitoring systems to include data from hospice and inpatient care settings would provide a more accurate picture of analgesic exposure among patients.
- Tailored Regulations: Rather than a blanket reduction in opioid prescribing, regulations should consider patient-specific factors, such as previous opioid use, comorbidity profiles, and socioeconomic status.
- Stakeholder Engagement: Bringing together clinicians, patient advocates, and policymakers can help create regulations that are both stringent and supportive.
Each of these measures should be weighed carefully, appreciating that any policy change is a result of countless little twists that can have significant impacts on patients’ lives. In essence, the goal is to work through these tricky parts without leaving anyone to bear the brunt of inadequate pain management.
Clinical Practices That Must Be Adapted Amid Changing Guidelines
As policies evolve, so too must clinical practices. Healthcare providers need to adjust their approach to pain management in response to emerging challenges. Some key steps include:
- Enhanced Education: Providers must remain up to date with changing guidelines and emerging evidence to make educated decisions on pain management.
- Interdisciplinary Collaboration: Effective pain management often requires input from multiple specialties including oncology, palliative care, and pain medicine. Such collaboration helps in weaving together the many layers of patient care.
- Patient Education: Educating patients about the potential side effects and benefits of all pain management options—including opioids and alternatives—can help mitigate the stigma and confusion surrounding their use.
- Continuous Review: Regular assessments of pain management outcomes and prescription trends can provide valuable feedback, ensuring that clinical practices are flexible and responsive to patient needs.
These actionable steps are key to ensuring that the healthcare system does not stall in offering effective treatments to those who need them the most. Providers must find their way through the tangle of shifting recommendations, balancing safety with the need for robust pain relief.
Conclusion: Charting a Course Through Confusing Driving Trends in Pain Management
The evolution of opioid prescribing policies is a clear example of how trying to tackle one problem can inadvertently stir up other challenges. The recent findings demonstrating a decrease in opioid prescriptions coupled with an increase in pain-related ED visits and opioid-related encounters among advanced cancer patients serve as a call to reexamine our approach to pain management.
Advanced cancer patients deserve an approach to pain that respects their unique challenges and conditions. A one-size-fits-all policy, however well intended, is insufficient when the stakes are so high. The current scenario is loaded with issues—from the increased reliance on gabapentinoids to the disproportionate impact on certain racial and socioeconomic groups. For these patients, balancing the needs of effective pain relief with the safety aspects of opioid use is a real and nerve-racking challenge.
As we move forward, both policymakers and clinicians must work hand in hand to fashion a regulatory environment capable of addressing the many tangled issues of pain management while ensuring that every patient receives the care they truly need. In rethinking and reengineering our approach, we must:
- Adopt flexible and responsive guidelines that recognize individual patient requirements.
- Invest in comprehensive monitoring systems covering all care settings to capture the complete picture.
- Emphasize interdisciplinary collaboration so that the multifaceted nature of advanced cancer pain can be addressed holistically.
- Consider the subtle details of racial and socioeconomic disparities to ensure equitable care for all patients regardless of background.
The data clearly indicate that while reduced opioid prescribing may have been a necessary step to counter opioid misuse, it has also created an environment where pain crises in advanced cancer patients are on the rise. With a commitment to revising policies and clinical practices, we can strike a better balance between reducing the risks of opioid overuse and maintaining essential pain relief.
Ultimately, the challenge lies in steering through these complicated pieces with care, sensitivity, and innovation. Healthcare providers must figure a path that acknowledges the hidden complexities of each patient’s situation and adjusts treatment plans accordingly. As we take a closer look at current trends and prepare for future shifts, it is super important that we foster a dialogue between researchers, clinicians, and policymakers to safeguard the well-being of patients facing one of the most overwhelming battles of their lives.
In coming years, further research will be necessary to determine how best to refine our approach. Studies should continue to evaluate the long-term impacts of shifting prescription practices while also exploring new avenues for pain management. The lessons learned from advanced cancer care can also offer insights into managing other chronic and severe pain conditions, ensuring that no patient is left without effective, compassionate treatment.
In conclusion, while the path forward might seem tangled with issues, the ultimate goal remains clear: to provide advanced cancer patients with pain management strategies that are both safe and effective. Addressing the current challenges with openness and innovation will not only improve the quality of life for these individuals but also set a precedent for a more adaptable and patient-focused healthcare system. It is high time that we find the balance whereby regulatory oversight does not impede but rather enhances the quality of care that these patients deserve.
As stakeholders continue to dig into the data and survey the clinical landscape, let us remain steadfast in our commitment to placing patient care at the center of every decision. The journey may be filled with twists and turns, but together, we can work through the confusing bits and ensure that every patient receives the attention, compassion, and effective treatment they need in their fight against advanced cancer.
In the end, rethinking our opioid prescribing policies with a focus on flexibility, comprehensive monitoring, and individualized treatment is not just a regulatory necessity—it is a moral imperative. Only by integrating these strategies into our clinical practice can we ensure that the advances in cancer treatment are not overshadowed by preventable pain crises and emergency visits.
This editorial underlines that while no single solution will resolve all the challenges, the cumulative effort to align policies with real-world clinical needs will pave the way for a more responsive and compassionate healthcare system. The road is full of tangled issues and nerve-racking uncertainties, but meaningful change is on the horizon when we work together with the shared goal of alleviating pain and improving quality of life for all patients battling advanced cancer.
Originally Post From https://www.renalandurologynews.com/news/opioid-prescribing-cuts-linked-to-rising-pain-crises-in-advanced-cancer/
Read more about this topic at
How the opioid crackdown is backfiring
Prescriber perspectives on low-value …