Revolutionizing Breast Cancer Screening with AI Integration
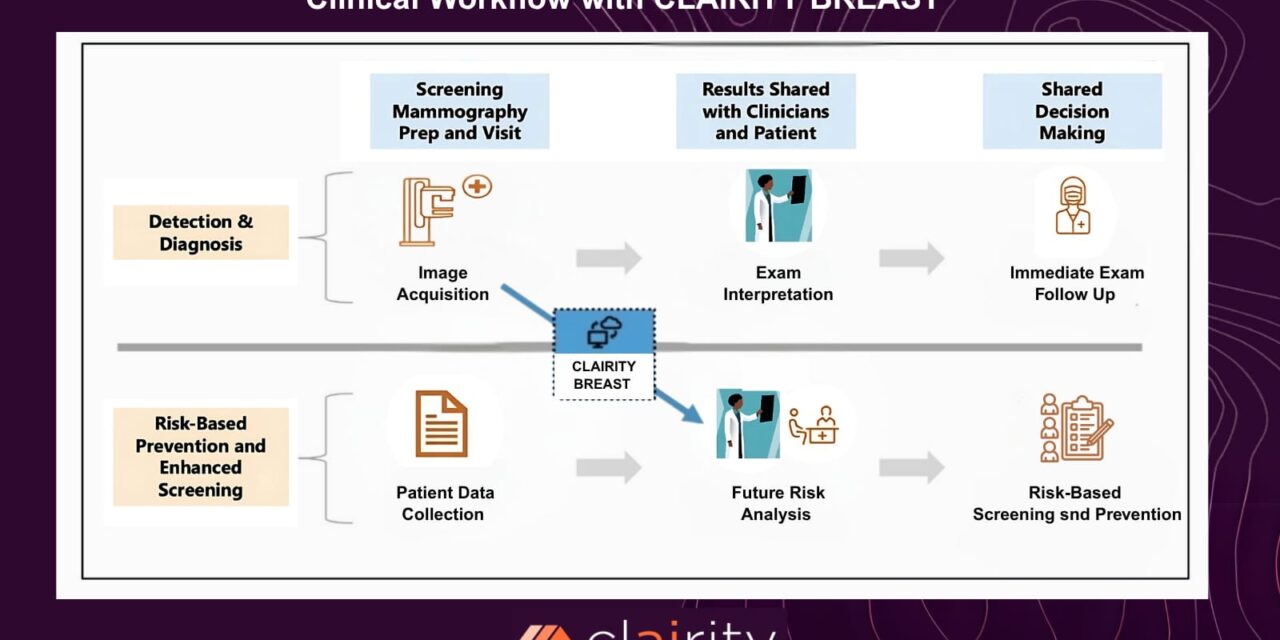
The recent authorization by the FDA of an AI platform to predict breast cancer risk marks a turning point in breast health care. This innovative system, known as CLAIRITY BREAST or Allix5, uses routine screening mammograms to generate a validated five-year risk score. In this opinion editorial, we take a closer look at the science behind this breakthrough, the subtle parts of its development, and the future implications for personalized medicine and early detection strategies.
For over 60 years, mammograms have played an essential role in catching early-stage cancers, helping save countless lives. Today, with advances in artificial intelligence and computer vision, we are beginning to uncover hidden clues in these routine images—clues that are often invisible to the human eye. This AI-driven approach aims to identify tricky parts of breast cancer risk that traditional methods may overlook, thereby providing a more detailed risk profile and enabling earlier, personalized interventions.
Unpacking the AI Model Behind CLAIRITY BREAST
The AI model that powers CLAIRITY BREAST was built and refined using millions of mammographic images. It was further validated with over 77,000 mammograms from diverse patient populations across five geographically distinct screening centers. This extensive dataset not only reinforces the model’s accuracy but also ensures that its predictions remain representative across a wide spectrum of individuals.
By analyzing minute details within mammograms, the platform can provide a risk score that considers subtle parts of the imaging data—those fine details that are often tangled issues in traditional screening. This model digests the nitty-gritty of mammographic features and correlates them with a woman’s future risk of developing breast cancer over the next five years.
Key Components of the AI System
- Data Aggregation: Millions of images from routine screenings ensure robust training.
- Validation Process: Over 77,000 patient images from different regions support diverse population risk assessment.
- Personalized Risk Score: The AI outputs a validated five-year risk prediction that helps healthcare professionals tailor further screening methods.
Using tables to simplify the broad scope of data analysis, we can outline the process as follows:
| Stage | Details |
|---|---|
| Data Collection | Gathering millions of routine mammogram images from diverse sources. |
| Training Phase | Feeding images into the AI system to teach it the subtle parts correlated with cancer risk. |
| Validation & Testing | Using a large validation set from five geographically distinct centers to ensure accuracy. |
| Risk Score Output | Producing a validated five-year risk score delivered via existing clinical systems. |
AI-Driven Risk Assessment: Impact on Personalized Care
One of the greatest promises of CLAIRITY BREAST is its support for more personalized, risk-based screening. Since each patient carries a unique risk profile, an AI system that provides a tailored risk score can help clinicians figure a path to better care. The personalized approach makes it possible to decide if patients might benefit from additional screening methods like MRI or other supplemental tests.
Personalized care is especially key in the context of breast cancer, where early detection dramatically increases the chances for a successful outcome. In identifying women with higher risk, the platform promises a more proactive engagement with patient care. Healthcare providers can now work through a strategy that includes more frequent follow-ups or even preventative measures for those who need it most.
Benefits of Personalized AI-Driven Screening
- Early Identification: The five-year risk score enables a head-start in the fight against cancer by catching potential signs early.
- Targeted Interventions: Those at a higher risk can be directed toward more intensive screening, such as MRI, thereby potentially catching the disease sooner.
- Reduction in Over-Screening: Lower-risk patients are less likely to undergo unnecessary, nerve-racking procedures, reducing stress and health care costs.
- Optimized Resources: Health systems can allocate resources more wisely and effectively, focusing where they are most needed.
Challenges and Considerations in Implementing AI in Medicine
Integrating artificial intelligence into routine medical screening is not without its own set of tricky parts. There are several challenging bits that both healthcare professionals and patients need to consider when it comes to adopting new technology in medicine.
One of the common concerns involves trust and reliability. When it comes to any new technology, especially one in a field as critical as oncology, ensuring that the science is sound is paramount. Developers have worked hard to ensure that the system is not only accurate but also equitable across different demographics. However, there still exists a level of hesitancy among some professionals who worry that the system’s deep learning algorithm might miss certain risk indicators endemic to particular population groups.
Another challenge revolves around the implementation of the system in existing clinical workflows. The platform is designed to work seamlessly with current imaging and reporting software, but learning to find your way around and effectively integrating the risk score into existing protocols takes time and commitment from all stakeholders in the medical community.
Common Obstacles When Adopting AI in Healthcare
- Data Privacy: Ensuring that patient data is handled with the upmost care is critical.
- Integration with Existing Systems: Aligning AI outputs with traditional imaging systems can be overwhelming and requires careful planning.
- Training for Healthcare Providers: Physicians and radiologists need sufficient training to effectively interpret and use AI-generated data.
- Ethical Considerations: Fairness and equity in AI predictions are essential to avoid inadvertent biases.
These issues, though intimidating, should not overshadow the potential benefits of such AI-driven initiatives. Instead, they suggest areas where further work is needed. As with many technological advancements, the benefits may outweigh the challenges provided that efforts are made to address these problematic areas head-on.
The Broader Context of AI in Cancer Detection
CLAIRITY BREAST represents one of several AI innovations in the field of oncology. AI’s role in cancer detection is rapidly growing as more data becomes available and computational power increases. In a field riddled with tension about early detection and outcome improvements, tools like this one allow us to better understand and manage the small distinctions that make a big difference in patient care.
Even beyond breast cancer, AI platforms are beginning to make inroads in assessing risk and identifying early signs of other types of cancers. Using machine learning algorithms to interpret medical imaging, genetic profiles, and patient history offers hope for a more proactive approach to medicine—a shift from merely treating disease to preventing it.
Comparative Analysis: Before and After AI Integration
| Aspect | Traditional Screening | AI-Enhanced Screening |
|---|---|---|
| Data Analysis | Based on visual interpretation by radiologists | Uses machine learning to detect subtle features invisible to the eye |
| Risk Prediction | General risk assessed from conventional criteria | Personalized risk score calculated from millions of data points |
| Implementation Time | Decisions based on periodic check-ups | Real-time risk feedback integrated into clinical systems |
| Follow-up Methods | Standardized screening frequency | Tailored follow-up scheduling based on risk outcomes |
This table highlights the fine shades of differences between conventional approaches and the new AI-enhanced methods. It is clear that personalized risk assessment may offer a more responsive framework that is crucial for advancing breast cancer detection and treatment.
Ethical Implications and Patient Empowerment
Beyond the technical aspects, the integration of AI in cancer risk prediction brings with it several ethical considerations. As with any technology that handles sensitive information, ensuring that patient data is kept private and secure is paramount. In an age where data breaches and misuse of information can be as nerve-racking as any medical procedure, there is a critical need for robust security protocols and ethical guidelines.
This platform was designed with transparency in mind. By ensuring that risk assessments are validated and equitable, innovators are helping to create an environment where AI can be trusted. Moreover, this approach empowers patients by giving them access to more comprehensive information about their health, enabling them to make more informed decisions. In doing so, patients are no longer passive recipients of care—they become active participants in their health journey.
Key Ethical Points to Consider
- Consent and Data Use: Patients must be informed about how their data is used in training and validating the AI model.
- Fairness in Predictions: Ensuring that risk assessments do not favor one group over another is super important for healthcare equity.
- Transparency: Clear communication about how the AI works and what the risk scores mean builds trust.
- Patient Empowerment: Empowered patients are more likely to engage in early detection and prevention strategies.
These ethical issues, while full of problems and challenging bits, also present an opportunity. They allow us to rethink how healthcare data is managed and how modern technology can be used not only to predict disease but to foster a deeper, more cooperative relationship between patients and providers.
Personalizing Preventive Strategies and Follow-Up Protocols
One of the transformative impacts of an AI-enabled risk prediction model is its potential to tailor preventive care. Traditionally, many patients undergo a one-size-fits-all screening protocol, which can lead to both over-screening and under-screening. With CLAIRITY BREAST, healthcare providers are granted a tool to sort out patients into more nuanced risk categories, thereby allowing for a truly personalized approach.
This proactive form of care ensures that patients with higher risk scores are not only monitored more stringently but also counseled about lifestyle choices and preventive actions that could help mitigate their risk. The ability to get into these subtle parts of a patient’s risk profile means that doctors have the chance to intervene earlier than ever before.
Customized Preventive Measures
- Enhanced Screening Frequency: Patients with higher scores might be recommended for supplemental imaging or follow-up examinations sooner.
- Lifestyle Counseling: Diet, exercise, and other preventive measures become a part of a tailored care plan for those at increased risk.
- Medication and Preventive Therapies: In some cases, preventive medication or hormone-related therapies may be advised based on the risk level.
- Genetic Counseling: Higher risk scores may prompt further investigation into a patient’s genetic predisposition to breast cancer.
These customized measures are designed to help patients steer through the twists and turns of their healthcare journey with greater confidence and clarity. By providing detailed risk information, doctors and patients together can choose interventions that are best suited to the individual’s needs.
Enhancing Clinical Decision-Making Through AI Insights
Integrating AI into clinical workflows does more than just adjust screening frequencies—it enhances the overall decision-making process. When faced with tricky parts and confusing bits of a patient’s history or imaging data, AI offers an extra layer of insight. It serves as a decision support tool that augments the expertise of healthcare providers, leading to a more comprehensive evaluation of risk factors.
For example, with a validated five-year risk score in hand, doctors can more effectively stratify patients by risk profile, resulting in faster and more accurate decisions. It also helps identify cases that might require immediate attention, reducing delays between diagnosis and treatment. This is especially important given the nerve-racking pace at which cancer can progress in some individuals.
Benefits in Clinical Decision-Making
- Improved Accuracy: AI algorithms can detect subtle features in imaging data that might be missed by the human eye.
- Time Efficiency: With a rapid risk score available, clinicians can make swifter decisions on follow-up care.
- Resource Optimization: By focusing additional tests and follow-ups only on higher-risk patients, healthcare resources are used more efficiently.
- Enhanced Collaboration: The risk score facilitates more productive discussions between radiologists, oncologists, and primary care providers regarding management strategies.
This layered approach not only boosts the confidence of healthcare providers but also reassures patients that their care plan is built on a solid foundation of both traditional medical expertise and cutting-edge technology.
Adapting to Rapid Technological Changes in Healthcare
The introduction of AI into routine cancer screening is a part of a much larger technological shift in healthcare. With digital health solutions making it easier to collect, analyze, and share patient data, the entire medical landscape is evolving at a fast pace. While these changes come with their own set of tricky parts and complicated pieces, they also offer vast potential for improving outcomes and personalizing patient care.
Clinicians, healthcare institutions, and patients must all figure a path to adapt to these new technologies. This means not only incorporating the latest tools into daily practice but also engaging in continuous education to stay current with technological advances. The shift toward a more AI-driven approach is both a challenge and an opportunity—a chance to redefine how preventive and diagnostic strategies work hand in hand.
Strategies for Adapting to AI in Healthcare
- Continuing Education and Training: Professionals must be provided with training programs that highlight the fine points of using AI tools responsibly.
- Interdisciplinary Collaboration: Bringing together experts from radiology, oncology, IT, and ethics can help streamline the integration process.
- Patient Outreach: Educating patients about the benefits and limitations of AI in screening fosters trust and understanding.
- Policy Development: Healthcare institutions need to develop clear policies to guide the use of AI while maintaining data privacy and ethical standards.
Adopting these strategies can ease the transition for all involved and help ensure that the promising benefits of AI are fully harnessed to improve patient care without exacerbating any hidden complexities.
Looking Ahead: The Future of AI in Breast Cancer Prediction
The FDA’s authorization of the first AI platform for breast cancer risk prediction is more than just a regulatory milestone—it is a signal that AI is rapidly becoming an integral part of modern healthcare. As CLAIRITY BREAST begins to find its way into clinical practice, we can expect further refinements in risk models, integration with other health data sources, and a broader application across various demographic groups.
In the coming years, it is likely that AI-driven predictive models will evolve to address even more of the twists and turns involved in cancer risk assessment. Future platforms might integrate genetic information, lifestyle factors, and even environmental data to produce even more finely tuned risk assessments. This convergence of technologies will not only help in framing personalized treatment plans but may also pave the way for preemptive interventions that could drastically reduce the incidence of breast cancer.
Potential Developments on the Horizon
- Integration with Genetic Profiling: Combining AI risk scores with genetic data to provide an even more personalized risk assessment.
- Real-Time Data Analysis: Improved algorithms that can provide immediate feedback during imaging sessions, leading to on-the-spot decisions.
- Expanded Demographic Analysis: Enhanced models that cater to underrepresented groups, reducing biases and ensuring fairness in risk prediction.
- Preventative Health Strategies: Greater emphasis on early intervention measures guided by real-time risk assessments, ultimately aiming to lower breast cancer incidence rates.
These advancements, although still in development, promise to reduce the overwhelming task of screening large populations by tailoring care based on individual risk profiles. The need for a highly responsive, personalized approach is more evident than ever as breast cancer incidences continue to rise globally.
Impact on Healthcare Systems and Policy
The introduction of CLAIRITY BREAST also necessitates adjustments at the policy level. As healthcare systems begin to incorporate AI-driven tools into routine practice, administrators and policymakers will need to tackle several nerve-racking challenges. These include establishing new standards for data management, revising protocols for screening, and ensuring that all practitioners are equipped with the necessary training to interpret AI outputs accurately.
Furthermore, insurance policies and reimbursement models may need to be updated to reflect the additional costs and benefits associated with these advanced screening techniques. By working together, regulatory agencies, healthcare providers, and industry leaders can create a sustainable framework that fully supports the integration of AI into clinical care.
Key Policy Considerations
- Standardization of AI Protocols: Developing uniform guidelines to ensure consistency and transparency in AI assessments.
- Data Privacy Regulations: Strengthening data protection measures to safeguard sensitive patient information.
- Training and Certification: Instituting certification programs to confirm that providers are well-versed in using AI tools.
- Insurance and Reimbursement Models: Adapting financial structures to support advanced, individualized screening methods.
With these policies in place, healthcare systems can better manage their way through the rapidly shifting landscape of medical technology, ensuring that innovative tools like CLAIRITY BREAST not only enhance patient outcomes but also reinforce the trust between patients and providers.
Patient Perspectives and Real-World Implications
The benefits of an AI-enabled breast cancer risk prediction tool extend well beyond clinical settings. For patients, receiving a personalized risk score can be both reassuring and eye-opening. Women who previously might have felt that traditional screening missed the fine points of their unique risk profiles can now gain a clearer understanding of their health status and the small distinctions that may influence their chances of developing cancer in the coming years.
Patient empowerment is at the heart of this technological advancement. Armed with concrete information about their risk, patients can steer through their healthcare choices more confidently. This can lead to more informed decisions regarding preventive care measures, lifestyle changes, and even discussions surrounding genetic counseling.
Voices from the Community
- Enhanced Awareness: Patients report feeling more secure when they understand their individual risk profiles.
- Active Engagement: Empowered patients are more proactive, seeking out further tests or consultations when necessary.
- Reduced Anxiety: Knowing that an advanced tool is being used to assess risk can alleviate some of the nerve-racking fears associated with ambiguous screening results.
- Supportive Care Decisions: With clearer risk information, patients can better discuss additional preventive strategies with their providers.
When patients are given the chance to get into the subtle parts of their risk assessments, the healthcare experience transforms from a passive, sometimes overwhelming process into one where they actively participate in their own care plan. This shift is crucial not only for individual outcomes but also for shaping public trust in new healthcare technologies.
Reflecting on the Journey: From Mammography to AI-Driven Care
Looking back on the evolution of breast cancer detection—from early mammography techniques to today’s AI-enhanced approaches—it is clear that innovation has played a critical role in improving outcomes. While deciphering the complicated pieces of traditional imaging has always been a challenge, the advent of AI now offers a more precise alternative that cuts through the confusing bits and offers a refined, personalized risk profile.
In many ways, the journey from analog to digital, from conventional screening to AI-driven prediction, mirrors broader shifts in healthcare. As we continue to integrate digital tools into everyday practice, we are not simply replacing one method with another; we are reimagining how we understand, assess, and ultimately treat disease. The transition is loaded with issues, and adapting to these changes may occasionally feel overwhelming. Nevertheless, the promise of improved early detection and reduced mortality rates provides compelling motivation to press forward.
Summing Up Key Takeaways
- Innovation in Imaging: AI is unlocking the hidden complexities of mammographic data, offering a new layer of insight that goes beyond human interpretation.
- Personalized Screening: The ability to deliver a validated five-year risk score transforms patient management, ensuring that those at higher risk receive more tailored care.
- Ethical and Practical Challenges: While integrating AI into healthcare involves dealing with nerve-racking challenges and complicated pieces, the potential benefits to patient care make these challenges worth addressing.
- The Future is Digital: As technological advances continue, AI-driven platforms will likely become a standard part of personalized cancer screening and prevention strategies.
As we look ahead, the importance of staying abreast of these developments becomes clear. Whether you are a patient, healthcare provider, or policymaker, these advances are super important in shaping the future of preventative care, highlighting the collaborative effort needed to steer through the twists and turns of modern medicine.
Final Thoughts: Embracing a New Era in Healthcare
The FDA’s authorization of CLAIRITY BREAST is more than just a regulatory endorsement—it represents a major leap toward a future where medical care is not only reactive but also highly personalized and predictive. By harnessing the power of AI, we are stepping into an era where detailed risk assessment can lead to earlier interventions, more tailored care, and, ultimately, better outcomes for women everywhere.
While there will undoubtedly be nerve-racking moments and some intimidating obstacles as we work through the integration of this new technology into everyday practice, the potential to improve early detection of breast cancer and save lives is a goal that unites all stakeholders in healthcare. The journey may be complicated, but as we dig into the fine points of AI-assisted medicine, it becomes increasingly clear that modern technology, when used responsibly, can be transformative.
Embracing tools like CLAIRITY BREAST, and similar innovations on the horizon, not only reinforces patient empowerment but also offers a clearer path toward a health care system that is adaptive, proactive, and inclusive. With each technological stride, we move closer to a system where personalized care is the norm and everyone stands a better chance of beating the odds against diseases like breast cancer.
In conclusion, integrating AI into breast cancer risk prediction is a crucial step forward in overcoming some of the tricky parts inherent in modern medical diagnostics. By combining the established effectiveness of traditional mammography with the cutting-edge precision of AI, the medical community is better equipped to tackle those hidden complexities that have long hindered our ability to forecast cancer risk accurately. While there remains work to be done in addressing the ethical, technical, and procedural challenges, the future of personalized preventive care appears brighter than ever.
As we continue on this path, it will be super important for all involved—medical professionals, technology experts, policymakers, and patients alike—to stay engaged, informed, and proactive. Together, we can ensure that advancements like CLAIRITY BREAST become a standard part of our healthcare toolkit, delivering on the promise of life-saving early detection and a more resilient, responsive health system for the future.
Originally Post From https://www.docwirenews.com/post/fda-authorizes-first-ai-platform-for-breast-cancer-risk-prediction
Read more about this topic at
5 AI Candidate Screening Methods to Add to Your Toolkit …
How AI is Transforming Resume Screening