Combining Ruxolitinib and Supportive Care for Improved Myelofibrosis Outcomes
The landscape of treating myelofibrosis has seen significant changes over the past few years. As an editor with a keen interest in both modern and alternative therapies, I take a closer look at recent research surrounding the use of ruxolitinib combined with anemia supportive care. This opinion piece delves into the study findings, discusses the practical challenges that healthcare professionals face, and offers an overview of what these developments mean for patients and the broader medical community.
Understanding Myelofibrosis and Its Treatment Options
Myelofibrosis is a rare blood cancer characterized by scarring (fibrosis) in the bone marrow. Over time, the normal production of blood cells can be replaced by fibrous tissue—leading to symptoms such as severe fatigue, an enlarged spleen, and troublesome anemia. As we dive into the evolving treatment landscape, it becomes clear that combining targeted therapies with supportive care measures is becoming a cornerstone of managing this complex condition.
Key Challenges in Myelofibrosis Management
Physicians and patients alike are facing many tricky parts and tangled issues when it comes to managing the side effects of myelofibrosis. Some of these challenging aspects include:
- Balancing effective symptom control with the adverse effects of treatments
- Dealing with the confusing bits of dose adjustments as patients respond differently
- Addressing the overwhelming treatment side effects that can be both physically and emotionally taxing
Combining ruxolitinib with supportive care strategies, particularly for managing anemia, is one approach that aims to counter these issues head on.
The Role of Ruxolitinib in Modern Myelofibrosis Treatment
Ruxolitinib, a Janus kinase (JAK) inhibitor, has revolutionized the treatment approach for myelofibrosis by significantly reducing spleen size and alleviating associated symptoms. The drug works by modulating the abnormal signaling pathways that promote inflammation and fibrosis. It is considered a key therapy—often the first line of targeted treatment—making it a must-have option for many clinicians.
Why Targeted Therapy Matters in Blood Cancers
The introduction of targeted therapies like ruxolitinib represents a paradigm shift in oncology treatment models. Instead of adopting a one-size-fits-all approach, modern medicine embraces personalized therapies that interfere with specific pathways. While this approach has offered hope, it comes with its own set of complicated pieces:
- Determining the ideal daily dose without compromising patient safety
- Tackling the hidden complexities in the individual patient’s treatment response
- Managing off-target effects that may arise during long-term therapy
In the context of myelofibrosis, the fine points of using ruxolitinib revolve around maintaining an effective daily dose that ensures spleen and symptom control. Physicians generally aim for a dose above 25 mg daily—equivalent to more than 10 mg twice a day—to achieve desired therapeutic results.
Managing Anemia: A Closer Look at Supportive Care
Anemia remains one of the most nerve-racking and complicated issues for patients diagnosed with myelofibrosis. It challenges both the patient’s quality of life and the overall management of the disease. In today’s treatment scheme, supportive care plays as crucial a role as the primary cancer therapy itself.
Integrating Supportive Care: The Role of ESA and Danazol
Supportive care for anemia often involves the use of erythropoietin-stimulating agents (ESAs) such as epoetin or darbepoetin, and in some cases, danazol. These agents help increase hemoglobin levels and reduce the need for transfusions. A recent post-hoc analysis of the phase 3b JUMP trial provided evidence that nearly 98 out of 101 patients received these agents alongside ruxolitinib.
The findings suggest that integrating supportive care with targeted therapy can lead to a balanced approach where the good spleen and symptom outcomes seen with ruxolitinib are not compromised by worsening anemia. In fact, the data indicate that hemoglobin levels, although slightly dipping at the outset, tend to recover as treatment progresses.
Long-Term Benefits of Anemia Supportive Interventions
From the perspective of patients, the initial nerve-racking dip in hemoglobin counts may cause some concern. However, over the long term, the supportive care measures ensure that patients remain on a stable course by:
- Maintaining an effective overall dose of ruxolitinib
- Balancing the transfusion need, which initially may spike but tends to drop below baseline levels over time
- Assisting some patients in achieving transfusion independence
This dual approach not only addresses the immediate symptoms associated with myelofibrosis but also provides more sustainable disease management. When patients can avoid frequent transfusions, their overall quality of life improves, and their treatment journey is less intimidating.
Diving into the JUMP Trial: A Post-Hoc Analysis
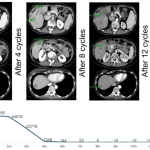
The recent post-hoc analysis of the phase 3b JUMP trial offered valuable insights into how ruxolitinib plus anemia supportive care maintained its efficacy in patients with myelofibrosis. For over a hundred patients included in the analysis, the combination therapy was carefully monitored for both efficacy and safety outcomes over a period of 48 weeks.
Study Design and Patient Demographics
To truly appreciate the study findings, it is important to understand the characteristics of the patient population:
- Out of 101 patients analyzed, nearly half had a hemoglobin level below 10—a marker for severe anemia
- Patients were mostly categorized as either intermediate-2 or high-risk, indicating more advanced disease
- There was a mix of baseline transfusion dependency, with a small group being transfusion-dependent upon entering the study
Despite these challenges, the trial demonstrated that patients were generally able to maintain a daily ruxolitinib dose around 25 mg. This consistency is crucial because it confirms that the effective therapeutic dose does not have to be sacrificed even when adding supportive care measures.
Key Findings from the Analysis
Some of the standout discoveries from the post-hoc analysis include:
- The successful maintenance of an effective ruxolitinib dose of about 25 mg per day throughout the study duration
- Comparable responses in spleen size reduction and symptom control when comparing the overall cohort to those with anemia, whether severe or moderate
- A trend showing that the hemoglobin levels, after an initial dip during the first few weeks, began leaning upward by the end of 48 weeks
- The fact that the need for blood transfusions was reduced over time, with some patients even becoming transfusion-independent
These findings are important as they highlight that the piecewise integration of anemia supportive care with ruxolitinib does not compromise the overall therapeutic benefit. Instead, it appears to bolster it, allowing for better management of both the disease and its systemic manifestations.
Understanding the Mechanics Behind Dose Management and Supportive Care
One of the key aspects of this treatment strategy is the practical management of dosing. Many clinicians encounter tricky parts when trying to figure a path through the maze of dose adjustments based on a patient’s evolving response. The analysis of the JUMP trial provided some clarity in this regard.
Effective Dose: Why 25 mg Daily Matters
For patients dealing with myelofibrosis, keeping the ruxolitinib dose at or above 25 mg daily is seen as essential. This threshold—often translating to more than 10 mg twice daily—has been broadly accepted because:
- It correlates with significant outcomes in spleen volume reduction
- It ensures adequate control of systemic symptoms such as fatigue and night sweats
- It appears to work harmoniously with supportive agents like ESAs and danazol to manage anemia
This stable dosing plays a key role in not only managing the disease but also in building confidence among both patients and clinicians that the chosen therapy is on the right track.
Tracking and Adjusting Hemoglobin and Transfusion Needs
The analysis observed that while there was an initial slightly lower ruxolitinib dose during the early weeks of treatment, this adjustment was temporary. Hemoglobin levels initially dropped—a nerve-racking detail for many—but began to recover within 4 to 8 weeks. By the end of the 48-week period, the average hemoglobin levels were slightly above baseline levels.
From a clinician’s viewpoint, this trend is crucial. It indicates that:
- Short-term fluctuations in blood counts need not deter the long-term benefits of the therapy
- Effective anemia supportive care can mitigate these early drops in hemoglobin levels
- Patients might even experience improved blood counts over prolonged treatment, offering a more sustainable outcome
This understanding helps health professionals make more informed decisions when determining the best course of action for each patient, ensuring that the treatment plan is flexible enough to adjust to individual needs.
The Practical Implications for Physicians and Patients
Beyond the numbers and statistics, the study results carry practical significance for those on the front lines of patient care. As we poke around the findings from the JUMP trial, several practical implications emerge:
Managing the Early Treatment Phase
One of the more intimidating phases of any treatment is the early period when patients are just beginning their therapy. During the initial weeks:
- Patients might see a dip in hemoglobin levels, which can be a source of concern for both patients and their families
- Clinicians need to reassure patients that this fluctuation can be temporary and part of the treatment’s natural progression
- Frequent monitoring is necessary to ensure that any early signs of worsening anemia are promptly addressed
In practical terms, clearly communicating these possibilities can help manage patient expectations and reduce the overall anxiety associated with early treatment adjustments.
Setting Realistic Expectations About Transfusions
Patients with advanced myelofibrosis often face the nerve-racking prospect of becoming dependent on blood transfusions. However, the JUMP trial analysis provides some much-needed glimpses of hope:
- There is evidence that over time, the initial increase in the transfusion requirement can reverse
- Some patients even achieve transfusion independence, a shift that can significantly improve their quality of life
- This positive shift underlines the importance of integrating anemia supportive strategies into the overall treatment plan
For physicians, these insights are instrumental in framing the conversation with patients, encouraging them to remain steadfast even during the more challenging early phases of treatment.
Diving Deeper into the Fine Points of Clinical Support and Patient Experience
While clinical trial data often provide an essential roadmap for treatment, the patient experience brings another layer of complexity. From a practitioner’s point of view, the intertwined roles of effective dosing and supportive care are central to making enduring progress in the fight against myelofibrosis.
The Importance of Steady Dosing Amid Fluctuant Blood Counts
Together, the observations suggest that maintaining an effective dose of ruxolitinib is super important—even if it means coping with short-term challenges. Many patients worry about the fine shades in their blood count readings, but the overall trend is encouraging:
- Steady dosing helps maintain control over the disease’s systemic symptoms
- Early dips in hemoglobin are often balanced out as the supportive therapies take full effect
- A focus on the big picture, rather than the small distinctions in early lab values, can help both patients and clinicians feel more optimistic about the treatment journey
This approach helps in reducing the perception of the treatment as being overly loaded with issues, instead positioning it as a balanced, strategic effort to improve patient outcomes over time.
The Emotional and Psychological Impact of Sustained Therapy
It is no secret that a diagnosis like myelofibrosis is not just physically challenging, but laden with emotional twists and turns. Patients often feel that the daily management of their therapy is overwhelming. However, knowing that the treatment protocol has robust supportive measures in place can be quite reassuring.
For instance:
- The reassurance that supportive care can mitigate early side effects helps ease anxieties
- Patients see tangible improvements in symptoms like fatigue, giving them hope and a sense of control
- The reduction in transfusion needs is a significant morale booster, as it minimizes disruptions to daily life
Ensuring that these aspects are not overlooked when discussing treatment options is key. This perspective not only enhances patient compliance but also helps them steer through the inevitable changes they encounter along the treatment journey.
How Clinical Practice Can Benefit from These Findings
For many clinicians, the path to implementing new treatment strategies is full of twists and turns. The insights gathered from the JUMP trial provide several practical takeaways for those treating myelofibrosis:
Developing a Tailored Approach for Each Patient
Not every patient will manifest the same reaction to the therapy; thus, the fine points of treatment must be adjusted on an individual basis. Some best practices include:
- Conducting frequent blood count assessments during the initial phases of treatment
- Adapting the supportive care regimen to match the evolving needs of the patient
- Communicating clearly with patients about potential early fluctuations and the long-term outlook
By using a customized approach, physicians can ensure that each patient gets a blend of aggressive therapy combined with adequate supportive measures, tailored to their unique circumstances.
Implementing a Collaborative Care Model
The management of myelofibrosis is not a one-person job. It requires a team effort where hematologists, primary care providers, and supportive care specialists work in tandem. A collaborative model can help in:
- Ensuring that all aspects of the patient’s well-being are monitored—from lab values to quality-of-life metrics
- Facilitating timely adjustments to the treatment plan when necessary
- Providing a safety net for patients during the nerve-wracking early weeks of therapy
This integrated approach means that not only the disease but also its cascading repercussions on daily life are managed with care and precision.
Addressing the Confusing Bits: The Subtle Interplay of Dosing, Support, and Outcomes
At the heart of the debate lies the question: Does the addition of anemia supportive care dilute the efficacy of ruxolitinib in myelofibrosis treatment? The data from the JUMP trial seem to suggest that it does not. Instead, the combination is capable of achieving the dual goal of symptom relief while simultaneously managing anemia—a particularly challenging aspect of the disease.
Analyzing the Transfusion Data
One of the more eye-opening insights is the change in transfusion requirements throughout the course of treatment. Early on, there is an uptick, but with time, the need for transfusions diminishes. This phenomenon is significant because:
- It shows that the body is gradually adapting to the therapy
- It underscores that short-term challenges are balanced by long-term benefits
- It provides evidence that robust supportive care can ease the nerve-racking challenges associated with severe anemia
These changes are especially important when considered from a quality-of-life standpoint. Reducing the frequency of transfusions not only lessens the physical burden but also alleviates the psychological stress associated with constant hospital visits and procedures.
The Impact on Spleen and Symptom Outcomes
Another critical observation from the trial was the sustained benefit in terms of spleen volume reduction and symptom control. Despite concerns that supportive care might interfere with the therapeutic regimen, patients maintained similar clinical outcomes compared to the overall study population. This finding is essential because:
- It emphasizes that addition of supportive care does not come at the cost of losing effective disease control
- It allows clinicians to confidently prescribe supportive therapies knowing they can complement the primary therapy
- It reinforces the idea that managing the patient’s overall condition requires addressing both the disease and its associated symptoms
This dual-benefit strategy can be seen as a blueprint for managing other hematological conditions where supportive care plays a major role alongside primary treatments.
Collating the Evidence: A Summary Table
To help visualize the key findings and their implications, consider the following summary table:
| Parameter | Observation | Implication |
|---|---|---|
| Ruxolitinib Dose | ~25 mg per day maintained | Effective dose not compromised by supportive care |
| Hemoglobin Levels | Initial dip; recovery by 4-8 weeks | Supportive care helps stabilize anemia over time |
| Transfusion Requirements | Increase in early weeks; decrease below baseline by 48 weeks | Reduced dependency over long-term treatment |
| Spleen and Symptom Response | Comparable with overall patient population | Maintains target outcomes without compromise |
Lessons Learned and the Way Forward
As we take a closer look at the findings from the recent analysis, several key lessons emerge that can help shape the future of myelofibrosis treatment:
- The combination of ruxolitinib with supportive care measures is both effective and feasible, even in patients with significant anemia.
- Maintaining an effective ruxolitinib dose is crucial for sustained symptom control and spleen reduction, even when transient fluctuations in blood counts occur.
- Robust communication between healthcare teams and patients helps in managing early treatment challenges and setting realistic expectations.
- Long-term monitoring and adaptive interventions, such as periodic dose adjustments and supportive care tweaks, are key to successful outcomes.
This evidence-based approach provides a roadmap not only for managing myelofibrosis but also for addressing similar challenges in other conditions where the interplay between primary treatment and supportive care is on edge.
Conclusion: A Promising Horizon for Myelofibrosis Therapy
In conclusion, the recent post-hoc analysis of the phase 3b JUMP trial offers a carefully measured yet optimistic view of combining ruxolitinib with anemia supportive care in myelofibrosis. The data indicates that while the initial phase of treatment may feature some nerve-wracking drops in hemoglobin and increased transfusion requirements, the overall long-term picture is positive. Spleen and symptom responses remain robust, and the improved management of anemia can ultimately enhance patient quality of life.
For clinicians, the study acts as a reminder that although the journey through dosage adjustments and the management of supportive care may be filled with tricky parts and tangled issues, the benefits can be far-reaching. The evidence suggests that maintaining a steady and effective ruxolitinib dose—around 25 mg daily—coupled with timely interventions to alleviate anemia, provides a template for successful therapy that can be fine-tuned to each patient’s needs.
The journey through myelofibrosis treatment is undeniably complex, with hidden complexities and early nerve-racking phases that can feel intimidating. However, these recent insights help allay fears by demonstrating that with careful monitoring, adaptive strategies, and collaborative care, patients can enjoy not only a reduction in disease symptoms but also improvements in daily life and overall well-being.
As research continues and more real-world data become available, the hope is that further refinements in therapy will further dig into the subtle details of patient management, ensuring that every individual receives the most effective, personalized care possible. This integrated approach—combining the best of targeted therapy and supportive measures—ushers in a promising horizon where the complex, often overwhelming treatment journey for myelofibrosis becomes a manageable, hopeful experience.
Ultimately, it is key for the medical community to keep finding its way through these complicated pieces, ensuring that every treatment decision is guided by both rigorous data and heartfelt empathy. The evolving narrative of myelofibrosis management stands as a testament to the progress we can achieve when research, clinical expertise, and patient-centered care join forces. The future remains bright, loaded with potential breakthroughs that could further revolutionize the care of patients facing this challenging disease.
For those in the healthcare industry—from clinicians managing daily cases to policy makers shaping treatment guidelines—this analysis is a reminder of the impact that well-strategized, supportive therapies can have. It reinforces the idea that even when the treatment landscape appears loaded with issues, innovative combinations can yield tangible, life-improving outcomes.
Looking ahead, continued emphasis on collaborative care, precise dosing, and ongoing monitoring will be essential. As we work through these twists and turns, the integration of supportive care with targeted therapies like ruxolitinib may emerge as the gold standard in managing myelofibrosis—offering patients a chance at a more stable, hopeful, and improved quality of life.
In this light, the findings discussed here are not just numbers on a page; they represent real advancements in the way we approach one of the more nerve-wracking challenges in hematologic care. As clinicians, researchers, and patients continue to work side by side, the experience gained from studies like the JUMP trial will undoubtedly shape a future where the treatment of myelofibrosis is as much about quality of life as it is about controlling disease progression.
As we continue to take a closer look at emerging therapies and refine our supportive care strategies, it is truly an exciting time in the field of hematology. With every new study and every patient success story, we gain a clearer picture of how best to work through the intricate maze of treatment options—ensuring that science and care combine to achieve outcomes that are both meaningful and life-affirming.
In summary, the balanced use of ruxolitinib and anemia supportive therapies marks a significant step forward. The journey is by no means without its challenges, but it is one filled with promise and potential—a promise that every patient battling myelofibrosis can look forward to a future with better-managed symptoms and an improved quality of life.
Originally Post From https://www.ajmc.com/view/ruxolitinib-plus-anemia-supportive-care-maintains-efficacy-in-myelofibrosis-pankit-vachhani-md
Read more about this topic at
Efficacy, safety, and survival with ruxolitinib in patients with …
Three-year efficacy, safety, and survival findings from …