Climate Change and Respiratory Health: A Growing Concern
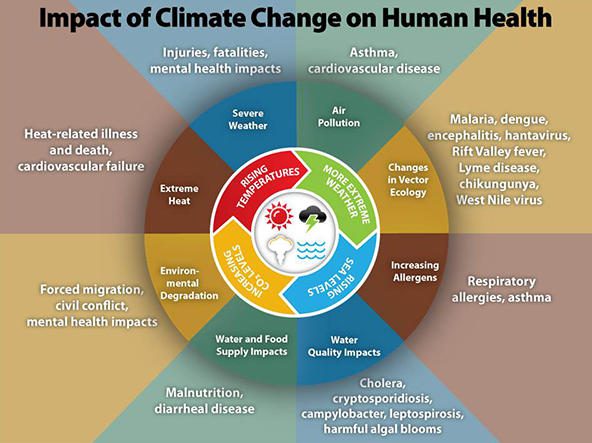
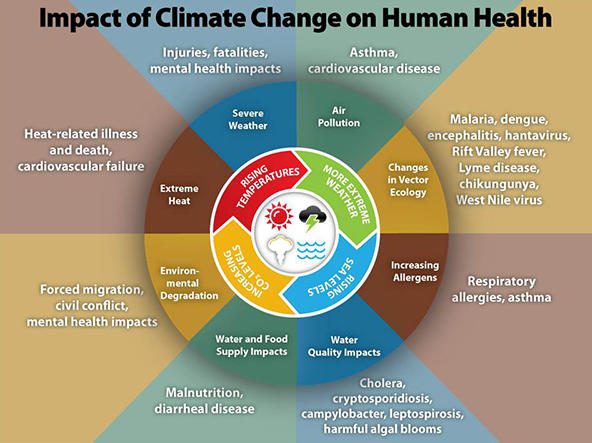
Our world is changing, and with it, the air we breathe appears to be getting trickier. Many experts now agree that human activities, especially the burning of fossil fuels, are causing not only global temperature shifts but also a host of environmental events that intensify conditions for respiratory diseases such as asthma and allergies. Over the past few years, spikes in extreme weather events and a rise in persistent pollutants have made the air more loaded with issues, making it crucial that we take a closer look at what these changes mean for public health.
Recent studies have linked dramatic climate changes – including wildfires, floods, heat waves, and thunderstorms – to a significant increase in allergic conditions and asthma attacks. When combined with the presence of persistent substances like per-and polyfluoroalkyl substances (PFAS) and microplastics, these events create an environment that challenges our understanding of respiratory health. In this opinion editorial, we will dive in to explore the various aspects of this evolving situation, examine the influence of each environmental trigger, and outline potential pathways for research and intervention.
Impact of Extreme Weather Events on Respiratory Conditions
Extreme weather events are no longer isolated or occasional. Instead, we are witnessing more frequent and intense occurrences of heat waves, floods, wildfires, and thunderstorms – each contributing in its own way to respiratory distress. The following sections shed light on how these events play into heightened levels of asthma and allergies.
Heat Waves and Their Role in Exacerbating Asthma
Heat waves represent a super important piece of the overall puzzle. With rising temperatures, the intensity and duration of heat waves are growing, leaving a lasting impact on respiratory systems. Research shows that increased ambient temperatures can lead to heat stress, which in turn causes inflation of airways, enhanced mucus production, and an overall increase in respiratory inflammation.
Some of the tricky parts related to heat-induced respiratory issues include:
- Activation of sensory fibers in the respiratory tract
- Disruption of epithelial barriers within the airway system
- Altering cytokine expression and T helper cell ratios
- Triggering bronchoconstriction
These tangled issues not only make asthma attacks more common but also put vulnerable populations – such as children, older adults, and pregnant individuals – at a higher risk of severe complications. With heat waves continuing to increase both in frequency and intensity, it is clear that more research is needed to get into the nitty-gritty of how temperature extremes directly contribute to respiratory distress.
Thunderstorm Asthma: A Scary Aftermath of Storm Conditions
Thunderstorm asthma is a well-documented phenomenon where a storm can trigger sudden, widespread asthma attacks. The process is thought to involve high levels of aeroallergens like ryegrass pollen, which are lifted high into the air and then ruptured by the force of the rain. This releases tiny, easily inhalable particles that reach deep into the lungs, provoking severe asthma attacks.
Key factors involved in thunderstorm asthma include:
- Heavy rainfall causing pollen to break down into smaller parts
- Concentration of allergens at ground level during storm conditions
- Environmental triggers that combine to produce overwhelming respiratory responses
While the direct link between fungal spores and thunderstorm asthma remains a subject for additional study, there is clear evidence that this weather phenomenon can lead to nerve-racking spikes in emergency visits and hospitalizations. As our climate continues to shift, understanding these subtle details becomes even more important in order to develop appropriate early-warning systems and treatment protocols.
Wildfires: A Menace Beyond the Flames
The intensity, frequency, and spread of wildfires have grown alongside climate change. These fires are especially problematic because they emit a variety of hazardous substances – including carbon monoxide, carbon dioxide (CO₂), nitric oxide, ozone, particulate matter, volatile organic compounds (VOCs), and polycyclic aromatic hydrocarbons – that directly affect respiratory health.
Wildfire smoke can be particularly detrimental for those already suffering from asthma or allergic conditions. Its toxic components not only trigger immediate symptoms such as coughing, wheezing, and shortness of breath but also contribute to longer-term respiratory complications. Here are some of the most concerning issues:
- Increased emergency department visits for respiratory issues
- Heightened risk of respiratory illnesses and even mortality
- Potential epigenetic changes that could predispose children to developmental respiratory problems
- Complex mixtures of pollutants—including both natural biomass and synthetic material from urban interfaces—leading to a distinct toxicity profile
Communities located near the wildland-urban interface are at a particularly high risk of experiencing these problematic effects. As developments creep closer to wildlands, the risk of ignited wildfires grows, along with the simultaneous combustion of homes, vehicles, and other synthetic materials. This combination creates a unique set of respiratory hazards that demand a concerted public health response.
Persistent Pollutants: A Stealthy Threat to Respiratory Health
Beyond the more visible environmental triggers such as heat waves and wildfires, there exists a subtler but equally worrying set of challenges: persistent pollutants like PFAS and microplastics. These substances are present in many consumer goods and are released during environmental events, lingering in the air, water, and soil.
PFAS and Their Elusive Impact
PFAS, or per-and polyfluoroalkyl substances, are a group of chemical compounds known for their nonstick properties and resistance to decomposition due to strong carbon-fluorine bonds. Because of their persistence, PFAS accumulate in the environment and eventually in the human body, exposing us through ingestion, inhalation, or skin absorption.
The subtle parts of PFAS-related health issues include:
- Long-term alteration of lung immune responses via inflammasome function
- Potential interactions with other environmental triggers leading to compound respiratory effects
- The challenge in setting comprehensive regulatory limits due to their pervasiveness in everyday products
- The need for increased public awareness about everyday exposure routes
Even though PFAS have been used extensively for decades, the full extent of their impact on respiratory health is only now coming into focus. Experts stress that research should focus on both establishing clear legislative guidelines and exploring innovative interventions to reduce exposure among the most vulnerable sections of society.
Microplastics: The Little Particles That Pack a Punch
Microplastics represent another area of emerging concern in the discussion of respiratory health. With climate change accelerating the degradation of larger plastic waste into smaller particles, these microplastics are becoming a widespread issue in the environment and human bodies alike.
Key concerns related to microplastics include:
- The ability of microplastics to bind to other pollutants, thereby carrying additional toxic substances into the respiratory system
- Direct links to respiratory irritations, interstitial lung disease, and persistent inflammation
- The challenges in defining safe exposure levels due to their hydrophobic surfaces and complex behavior within biological systems
- A pressing need to understand their biological effects, including exposure routes and internal transport mechanisms
The persistence of microplastics in the environment means that even if emissions and waste production are curtailed, these tiny particles will continue to affect respiratory health for decades. This situation calls for coordinated efforts in both research and environmental management to lessen their impact.
Environmental Triggers in Modern Respiratory Diseases
The interplay of extreme weather events, persistent pollutants, and other climate-driven changes creates a scenario where multiple stressors converge on human health. When we consider respiratory conditions such as asthma, allergic rhinitis, and eczema, it becomes evident that environmental triggers substantially complicate their management.
Allergic Rhinitis, Eczema, and Food Allergies in a Changing Climate
Approximately one in three adults and one in four children in the United States report conditions such as allergic rhinitis, eczema, or food allergies. Researchers have started to notice that the extended pollen seasons — caused by warmer temperatures and changing precipitation patterns — are introducing new allergenic species into our environment. This means that individuals battling these conditions now face a much longer and heightened exposure to allergens.
Some notable observations include:
- Longer and more intense pollen seasons leading to increased allergen load
- Early snowmelt and hotter spring conditions that accelerate the growth cycles of plants
- A rising incidence of allergic inflammation that can compound eczema and food allergies
- The need for new therapies tailored to these prolonged exposure scenarios
The combined stress of elevated temperatures, prolonged allergen exposure, and the presence of additional environmental toxins makes managing these conditions a nerve-racking challenge. Patients and healthcare providers alike are finding it increasingly important to monitor environmental conditions and adjust treatment plans accordingly.
Floods and the Growth of Mold: A Hidden Respiratory Menace
Floods, whether from sea surges or inland water overflows, bring with them a host of respiratory concerns that are as tricky as they are persistent. When buildings and homes are flooded, the resulting mold and microbial growth not only damages property but also creates a proinflammatory environment that can trigger respiratory ailments.
The toll of flood-induced respiratory issues includes:
- Heightened risk of respiratory infections and asthma exacerbations primarily due to mold spore exposure
- Increased levels of allergic rhinitis and other allergic conditions among those living in damp environments
- Emerging challenges in identifying which specific mold or fungal strains are responsible for triggering these responses
- A need for more detailed research on chronic respiratory issues resulting from prolonged flood exposure
This topic raises some of the more confusing bits in the debate on environmental health. While immediate exposure effects can be measured and observed, the longer-term consequences of mold exposure in flooded environments require more comprehensive study. As floods are likely to become more common due to climate change, understanding and mitigating these health risks is crucial.
Interacting Environmental Stressors: A Compound Risk Analysis
One of the most challenging aspects of managing respiratory health in the context of climate change is the way different environmental stressors add up. Unlike isolated events, these factors often interact in ways that are more than the sum of their parts, weaving a web of intertwined exposure risks.
Key Combined Effects of Environmental Triggers on Respiratory Health
When discussing the combined impacts of extreme weather events and persistent pollutants, several key points emerge:
| Environmental Trigger | Respiratory Impact | Associated Challenges |
|---|---|---|
| Heat Waves | Increased inflammation, mucus hypersecretion, bronchoconstriction | Disruption of airway proteins, vulnerable population risk |
| Thunderstorms | Spike in airborne allergens from ruptured pollen grains | Rapid onset of asthma attacks, overwhelming emergency services |
| Wildfires | Exposure to toxic mixtures, exacerbated asthma symptoms | Long-term respiratory issues, distinct toxicity from synthetic materials |
| Floods | Mold growth leading to allergic inflammation | Difficulty in pinpointing exact microbial culprits, chronic respiratory complications |
| Persistent Pollutants (PFAS, Microplastics) | Prolonged respiratory irritations and immune dysregulation | Complex interaction with other pollutants, tough degradation properties |
This table provides a snapshot of how varying environmental factors produce a myriad of effects on the respiratory system. The interactions are not straightforward; rather, they present a series of mixed signals that complicate both diagnosis and treatment. Professionals in environmental medicine and pulmonology are urged to dig into these details to design better, multi-faceted prevention and intervention strategies.
The Need for Comprehensive Research and Public Health Measures
Given the multitude of factors that contribute to respiratory ailments in our changing world, future research must adopt a holistic approach. Meta-analyses that quantify the health effects following natural disasters and extreme weather events could be invaluable in informing public health measures. The following are key areas that require further exploration:
- Quantifying the additive or synergistic roles of heat, pollutants, and allergens
- Studying the subtle effects of prolonged exposure to low doses of persistent chemicals such as PFAS and microplastics
- Exploring intervention and mitigation techniques tailored to different demographic groups considering their unique vulnerabilities
- Developing early-warning systems to help communities brace for extreme weather events with a high allergen or pollutant load
In short, tackling these tricky issues head-on would not only aid in preparing our healthcare system for future challenges but could also provide crucial insights into how best to protect vulnerable populations during times of environmental upheaval.
Public Health Implications and the Need for Policy Change
It is not just individual health at stake here – systemic policy change is essential to safeguard collective welfare. Governments, regulatory bodies, and public health organizations have a super important role to play in regulating emissions, managing waste, and initiating research into alternative materials that might reduce PFAS and microplastic pollution.
Implementing Stronger Environmental Regulations
Policymakers must consider the long-term consequences of environmental triggers on public health. Some measures that could help steer through these challenges include:
- Stricter limits on industrial emissions and waste management practices to curb the release of persistent pollutants
- Investment in green technologies and renewable energy sources to reduce reliance on fossil fuels
- Enhanced guidelines around land use in wildland-urban interfaces to minimize the risk of large-scale wildfires
- Improved infrastructure to better handle extreme weather events like floods, thereby reducing conditions that lead to mold and microbial growth
These policy measures, while at times off-putting due to economic and political challenges, are absolutely essential for ensuring a healthier future. Only by addressing the root causes of these environmental issues can we hope to reduce the burden of respiratory diseases on our society.
Community Awareness and Preventative Actions
While policy changes are essential, there is also a significant role for community-level actions. Increasing public awareness about the environmental triggers of respiratory disease can help individuals better manage and monitor their exposure. Some community-driven solutions that can support these efforts include:
- Local educational campaigns highlighting the importance of air quality and ways to minimize exposure to allergens and pollutants
- Development of community response plans for extreme weather events and local advisories about wildfire smoke or high pollen days
- Enhanced access to healthcare and screening for vulnerable populations during periods of extreme environmental stress
- Collaboration between local governments and environmental agencies to improve monitoring systems for PFAS, microplastics, and other persistent pollutants
These grassroots initiatives may be one of the best ways to manage the nerve-racking, unpredictable outcomes of our changing climate’s influence on respiratory health. By finding your way through the maze of available resources, communities can help buffer the public health impact while broader systemic changes take effect.
Digging Deeper into Prevention Methods and Treatment Options
The environment we live in is a constant reminder that prevention is more efficient than reaction. There are several approaches to reducing the overall inflammatory burden caused by environmental stressors that exacerbate asthma, allergies, and other respiratory conditions.
Innovative Medical Interventions and Research Opportunities
Recent studies have shown encouraging advances in how we might approach treatment and prevention of respiratory issues triggered by environmental factors. For example, proactive management of seasonal allergies could potentially reduce cumulative inflammation, thereby lessening the neuroinflammation that might also impact mental health. In the wake of extreme weather events, early intervention can be crucial.
Some promising avenues include:
- Developing immunotherapies that specifically target allergens introduced or enhanced by climate change
- Researching new pharmacological treatments that can better manage inflammation induced by heat stress and pollution
- Integrating environmental data into clinical practice, so healthcare providers can provide immediate guidance during episodes of extreme weather or high pollution
- Exploring the potential of digital health platforms to monitor respiratory symptoms and provide real-time advice on minimizing harmful exposures
By taking a closer look at these options, the medical community can pave the way for improved care that is both proactive and responsive to the unpredictable twists and turns thrown up by climate change.
Strategies for Personal Health Management
On an individual level, there are some simple steps that people can adopt to reduce their risk of respiratory distress during periods of extreme environmental stress:
- Monitor local air quality and weather forecasts regularly to know when conditions might spike
- Invest in high-quality air purifiers or masks during times of wildfire smoke or high pollen days
- Maintain regular check-ups with healthcare providers to adjust treatment plans based on seasonal or regional environmental trends
- Pay attention to indoor air quality, particularly after events like floods where mold growth is likely
These steps, while they might seem like small distinctions in daily routines, can add up to make a significant impact in managing respiratory health. Both patients and practitioners should work together to figure a path through these challenges by keeping informed and prepared.
Looking to the Future: An Integrated Approach to Respiratory Health
As we cast our eyes toward the future, it is clear that managing respiratory health in the face of climate change is a full-of-problems challenge that requires a combined effort from multiple sectors. From public policy and community initiatives to cutting-edge medical research, addressing the respiratory consequences of environmental stressors is a task that must be tackled from every angle.
Integrating Environmental Data with Healthcare Practices
A holistic approach that links environmental monitoring with healthcare delivery could revolutionize how we respond to respiratory crises. Imagine if local weather data, air quality indices, and pollutant levels were all seamlessly integrated into healthcare systems. Such integration could allow healthcare providers to:
- Issue timely advisories tailored for patients with respiratory conditions
- Modify treatment protocols based on forecasted environmental exposures
- Advise on personalized prevention strategies in response to local conditions
- Enhance data collection for research aiming to understand the finer points of environmental impacts
It is essential to develop digital tools and interactive platforms that can help both patients and clinicians get a better grip on these intertwined issues. Collaborative efforts in this area will be key to reducing the overall healthcare cost, improving quality of life, and ensuring that prevention remains a super important aspect of care.
Addressing Gaps in Current Research
There are still several confusing bits and tangled issues in our current understanding of how environmental factors interact with respiratory health. COVID-19, for instance, has already demonstrated that airborne pollutants and respiratory diseases can combine to create an overwhelming public health challenge. Now, as we face the specific threats posed by climate change, further research is needed to address questions such as:
- How do low-level exposures to PFAS and microplastics interact with other environmental triggers?
- What are the long-term health consequences of repeated exposure to wildfire smoke, especially in children?
- How can early intervention strategies be tailored to mitigate the staggered impacts of prolonged allergen seasons?
- What community-level measures can be implemented to reduce exposure to mold and microbial growth after floods?
By engaging in meta-analyses and large-scale observational studies, researchers can unlock the hidden complexities of these interactions. A better understanding of these factors will, in turn, pave the way for more effective prevention and intervention strategies in the years to come.
Final Thoughts: Charting a Course Through Environmental Challenges
There is no doubt that the environmental changes driven by climate change and human activity present a series of nerve-racking challenges for respiratory health. From extreme weather conditions like heat waves, thunderstorms, and wildfires to the subtle but persistent threats posed by PFAS and microplastics, our air is increasingly loaded with triggers that complicate both health and treatment.
However, rather than being overwhelmed by these developments, it is essential that we take an active role in sorting out the tangled issues before us. With a combination of smart public policy, targeted research, and community education, it is possible to develop a robust response that protects vulnerable populations and reduces the burden of respiratory diseases.
As we move forward, it is clear that the responsibility to get into the nitty-gritty of these environmental challenges lies with both the scientific community and policymakers. By refining our understanding of each environmental trigger and its role in respiratory disease, we can work towards more effective preventative measures and better treatment protocols.
Ultimately, the task ahead demands that we figure a path that integrates innovative medical interventions with strong regulatory frameworks and empowered, informed communities. Only then can we hope to achieve a healthier future where respiratory conditions are managed more effectively, and the air we all share is a bit cleaner.
Key Recommendations for Moving Forward
To summarize, here are some of the key recommendations for tackling the impact of climate change on respiratory health:
- Enhance Monitoring Systems: Integrate environmental data with healthcare practices to offer real-time advisories and intervention strategies.
- Invest in Research: Prioritize studies that explore the combined effects of extreme weather events, persistent pollutants, and prolonged allergen exposure.
- Implement Policy Changes: Strengthen environmental regulations to minimize emissions, manage waste, and protect vulnerable regions.
- Increase Public Awareness: Launch community initiatives that educate citizens about the risks of environmental triggers and provide practical prevention methods.
- Foster Collaborative Efforts: Encourage partnerships between public health organizations, policymakers, and the scientific community to develop integrated responses.
These recommendations are not merely suggestions but must-have strategies in a time when the air we breathe is being reshaped by both nature and human activity. Only through coordinated, proactive measures can we hope to mitigate the multiple threats our environment poses.
Conclusion: Embracing a Multi-Pronged Strategy for Healthier Air
In conclusion, the landscape of respiratory health is becoming more loaded with issues as the climate continues to change. Whether it is the increased duration of pollen seasons, the rising frequency of heat waves and wildfires, or the expanding presence of persistent pollutants like PFAS and microplastics, each factor presents its own set of tricky parts that require careful handling.
It is a time for the scientific community, policymakers, healthcare providers, and individuals alike to find your way through this maze of environmental triggers. By taking proactive measures—ranging from enhanced monitoring and research to community education and regulatory reforms—we can bridge the small distinctions between current challenges and future solutions.
While the journey ahead may be overwhelming and full of surprises, it is absolutely critical to remember that every small step taken in reducing exposure and improving treatment strategies has the potential to make a significant difference in the lives of millions. As we continue to work through these environmental challenges, a concerted, multi-pronged strategy is essential to ensure not only healthier air but also a brighter, more sustainable future for all.
Originally Post From https://www.ajmc.com/view/allergies-and-asthma-prevalence-rise-with-climate-change-extremes-and-pollutants
Read more about this topic at
Climate change is supercharging pollen and making …
Climate change and allergic diseases: An overview – PMC