Rethinking Nutrition for Head and Neck Cancer: Addressing the Tricky Parts
Head and neck cancer has long been recognized as not only a formidable disease but also a condition that brings along a host of tangled issues. One of the most concerning challenges is the significant nutritional deficit that many patients experience throughout their treatment. This op-ed takes a closer look at how the twists and turns of cancer treatment create complicated pieces for patients and calls for innovative strategies, robust research, and sensible policy changes to enhance nutritional care.
Even before treatment begins, individuals diagnosed with cancers of the mouth, throat, or voice box often face nerve-racking side effects that make eating difficult. For many, these nutritional challenges are more than just a side note—they are a central component that affects treatment outcomes, quality of life, and overall survival. In this discussion, we will get into the nitty-gritty of the issue, explore the tangled issues that hinder optimal nutrition, and emphasize why improved support from registered dietitians is essential.
The Challenges and Tangled Issues of Nutrition in Head and Neck Cancer
Cancer in the head and neck region can trigger a cascade of problems, from difficulty swallowing and chewing to severe changes in taste. These issues are often compounded by treatments such as surgery, radiation, and chemotherapy, which themselves bring overwhelming side effects. The pathway to ensuring adequate nutrition becomes riddled with tension as patients struggle with symptoms like dry mouth, nausea, and painful mouth ulceration. These small distinctions—often the fine points of how one maintains sufficient protein and calorie intake—prove to be a super important concern during every stage of the treatment journey.
The tumor itself can be more than just a physical mass; it can lead to real knocking effects in day-to-day nutritional care. The confusing bits of treatment side effects—such as taste changes and gastrointestinal disturbances—make it nerve-racking for patients to secure enough calories. In many respects, tackling these issues calls for a reassessment of how we consider nutrition as part of cancer therapy rather than a secondary concern.
Understanding the Interplay Between Cancer Treatment and Diet: A Dive into the Nitty-Gritty
When managing head and neck cancer, dietary concerns do not exist in isolation. Instead, they are closely linked with treatment outcomes and the general well-being of patients. Surgical resections, for example, can dramatically alter the anatomy involved in eating, while radiation therapy may lead to a persistently dry mouth that hinders not just swallowing but also the enjoyment and nutritional value of food. These changes often lead to a decrease in the overall quality of life and, in extreme cases, even influence the patient’s ability to stay on treatment.
In many instances, treatment strategies that are designed to clear the tumor inadvertently impose complications on the patient’s nutrition. It becomes essential to get into the fine points of how nutritional therapy is deployed in these scenarios. The physical and emotional strain combined with the awkward side effects of treatment make proper nutritional strategies feel almost out of reach for many. To ensure a better prognosis, patients need more than just clinical treatment—they need guided support in managing their diets to match their new and challenging nutritional requirements.
Barriers to Accessing Registered Dietitian Support: Overwhelming Gaps in Care
One of the most problematic issues in cancer care today is the glaring gap in access to registered dietitians. Registered dietitians play a key role in helping patients manage tricky parts of nutrition, from creating high-protein meal plans to advising on alternative liquid diets when solid foods become too challenging. Despite these efforts being crucial for enhancing nutritional status, many United States cancer centers have not been able to provide adequate dietitian support for each patient.
A recent report has highlighted that the ratio of a dietitian to cancer patient is as sparse as one dietitian per 2,308 patients—a ratio that is clearly insufficient to meet the growing needs. In many cases, medical nutrition therapy is not covered by insurance, which further limits patient access to these services. As a result, even when patients are faced with off-putting side effects that jeopardize their nutritional intake, the appropriate professional support may not be available.
This lack of support creates a domino effect: without proper nutritional guidance, patients are more likely to experience muscle wasting, prolonged recovery, and increased mortality. It is incumbent on the healthcare system to invest in more robust nutritional support, not only for better patient outcomes but for a more sustainable, patient-centered care model.
Call for Integrated Research: Poking Around for Effective Nutritional Interventions
A notable call to action has recently emerged from researchers who have raised concerns about the insufficient research in the realm of head and neck cancer nutrition. A multidisciplinary team, including experts from institutions such as KU Medical Center and the Moffitt Cancer Center & Research Institute, recently published an article in Lancet Oncology that emphasizes the need for prioritized research in this area. This study outlines a roadmap of eight actionable items designed to clear the confusing bits that stymie progress in nutritional care for these cancer patients.
Some of the key recommendations include:
- Improving access to medical nutrition therapy provided by registered dietitians
- Establishing clear reimbursement policies for these essential services
- Addressing the nutritional care needs of long-term cancer survivors
- Creating consensus on criteria for the use of feeding tubes
- Enhancing nutrition literacy among patients diagnosed with head and neck cancer
- Increasing access to psychological screenings and support services
- Closing gaps in speech-language pathology care to help with swallowing and communication difficulties
- Promoting active, supervised participation in tailored exercise programming
These recommendations are not only timely; they represent a systematic plan to work through the little twists and high-stakes issues that hinder patient recovery.
Tackling the Controversies: A Table Highlighting Challenges and Proposed Solutions in Nutrition Therapy
Complex challenges require a clear presentation of both the problematic areas and the suggested strategies. The table below provides an overview of the main issues tied to head and neck cancer nutrition and the corresponding recommendations to overcome these hurdles.
| Tricky Parts in Nutrition Therapy | Proposed Solutions and Strategies |
|---|---|
| Difficulty swallowing and chewing due to tumors and surgeries |
|
| Taste changes and dry mouth from radiation and chemotherapies |
|
| Limited access to registered dietitians due to inadequate staffing and insurance coverage |
|
| Lack of standardized protocols for nutritional interventions |
|
| Poor nutrition literacy among patients |
|
This table illustrates a step-by-step roadmap that underscores the necessity of a synchronized effort between research, clinical practice, and policy advocacy. The aim is to clear away the overwhelming issues that make it so challenging for patients to make their way through these nutritional problems.
Policy Recommendations: A Path Forward for Nutritional Care in Cancer Treatment
It is one thing to recognize the tangled issues within cancer nutrition, but it is quite another to implement practical policy changes that can lead to measurable improvements. Policy makers are now being called upon to address several off-putting gaps in care, including:
- Reimbursement Policies: Establishing medical nutrition therapy reimbursement policies would ensure that more patients receive the expert guidance they need, without incurring crippling out-of-pocket expenses.
- Insurance Coverage: Expanding insurance coverage for registered dietitian services is critical. When nutrition therapy is fully integrated into cancer care plans, recovery and quality of life for patients are bound to improve.
- Standardized Intervention Protocols: Clear, evidence-based guidelines can help clinicians figure a path through the labyrinth of different intervention strategies by ensuring consistency and reliability when it comes to patient care.
The implications of adopting these policies are far-reaching. Enhanced nutrition not only contributes to increased survival rates, but it also boosts overall treatment tolerance and improves both physical strength and mental well-being. By providing the infrastructure needed for better nutritional support, we pave the way for holistic recovery.
Integrating Multidisciplinary Approaches: Practical Steps for Community Outreach and Patient Support
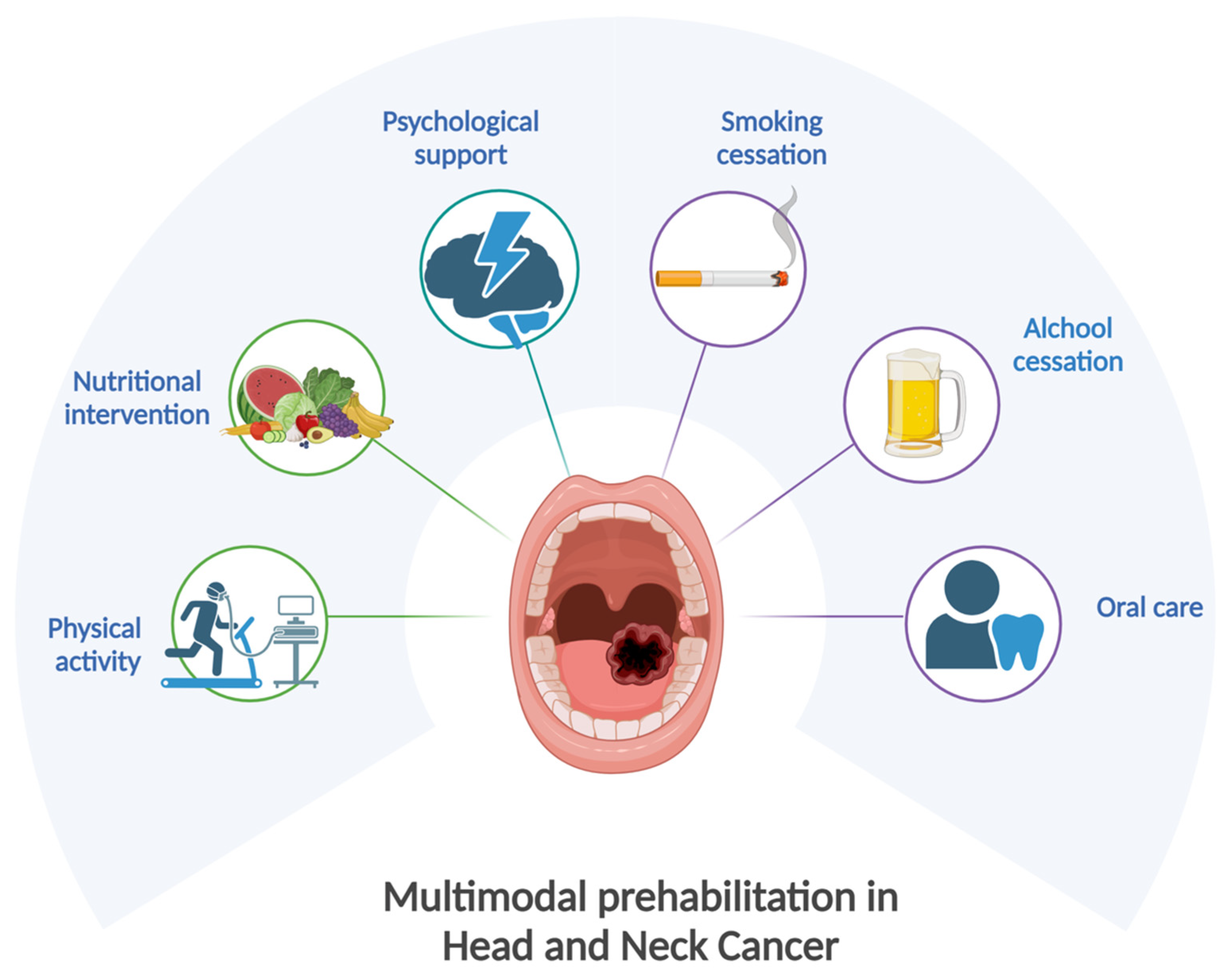
Addressing head and neck cancer nutrition requires more than just clinical interventions. It calls for a multidisciplinary approach that wraps around the patient like a safety net. From nutritional experts and speech-language pathologists to psychologists and exercise physiologists, a diverse team of professionals can help patients manage the nerve-racking side effects that impair healthy eating.
Community outreach programs have a role to play here too. By organizing workshops, seminars, and support groups, healthcare providers can impart practical tips to manage the subtle parts of nutrition issues. These community-based initiatives offer a space for patients to exchange experiences and practical advice, effectively complementing the clinical efforts. Such programs can ensure that even long-term survivors receive ongoing nutrition counseling and support, making the journey from diagnosis to remission less intimidating.
The Role of Patient Empowerment and Education: Getting into the Fine Points of Nutrition Literacy
Patient empowerment is key when tackling the pervasive nutritional issues faced by those with head and neck cancer. Many patients often feel overwhelmed by the nerve-racking side effects and the profound alterations to their normal eating habits. However, initiatives designed to improve nutrition literacy can help them regain a sense of control.
Empowering patients means not only providing them with easy-to-understand information about their nutritional needs but also ensuring that they have access to experts who can help sort out the fine details. Educational programs, prepared with a focus on clear and practical guidance, can cover topics such as:
- How to modify food choices to accommodate a sensitive throat or altered taste perception
- Creative recipes for liquid or softened diets that retain nutritional value
- Simple strategies for reading food labels and identifying high-calorie, high-protein options
- Tips on managing side effects like nausea and dry mouth through dietary adjustments
Furthermore, patient education plays a significant role in dispelling fear and uncertainty related to nutrition. When patients are informed about the available nutritional strategies and resources, they are more likely to take an active role in their own care. This increased involvement can lead to better treatment tolerance and overall well-being.
Community and Economic Impact: Broader Implications Beyond Clinical Settings
Beyond the immediate clinical benefits, improved nutritional care for head and neck cancer patients resonates with broader community and economic implications. When patients receive proper nutritional support, they are generally more resilient during treatment, which can translate to shorter hospital stays and lowered healthcare costs. This positive ripple effect extends into local communities, where reduced complications mean that patients can return to their daily lives sooner.
Fostering better nutritional outcomes can also stimulate community wellness programs that provide ongoing education and support. Local organizations, hospitals, and even nutrition-focused gyms can join forces to support cancer survivors, ensuring that every patient has a network of resources at their disposal. In doing so, the community not only aids in recovery but also fosters an environment where proactive health management becomes a collective endeavor.
From an economic standpoint, preventing severe malnutrition can reduce the overall burden on healthcare systems. Insufficient nutrition is directly linked to increased mortality and lower tolerance to aggressive therapies—factors that often lead to additional treatments and extended hospital stays. By investing in better nutritional care, policymakers and healthcare providers can eventually see a decrease in long-term healthcare costs and an improvement in survival rates.
Expert Voices Speak: Insights from Dietetics and Cancer Care Practitioners
Among the voices leading this critical conversation is Anna Arthur, Ph.D., MPH, an associate professor of dietetics and nutrition who has worked closely with head and neck cancer patients. In her many years of clinical practice, Arthur has observed firsthand the overwhelming challenges that patients face—not only from their tumor-induced symptoms but also from the subsequent impacts of intense treatment regimens.
Arthur explains that while there is a wealth of knowledge about the physical interventions required to combat the tumor, there remains a severe deficit in evidence-based nutritional strategies. The subtle parts of nutrition intervention—such as determining the most appropriate liquid diets, adjusting meal textures, and timing nutritional interventions around treatment cycles—are still largely tossed aside. According to her observations, even though registered dietitians play a crucial role in guiding patients, their services are hampered by inadequate insurance coverages and staffing shortages.
In a recent consensus paper published in Lancet Oncology, Arthur’s multidisciplinary team laid out a clear agenda for future research and clinical application. This document is much more than an academic exercise; it is a call to action urging institutions, policymakers, and the broader research community to work together in addressing the myriad issues that continue to plague nutritional therapy in head and neck cancer treatment.
Her insights underscore a simple yet powerful truth: robust and integrated nutritional support not only combats the physical complications of head and neck cancers but also bolsters patient morale, supports families, and lessens the emotional burden that comes with a serious diagnosis. When patients are given the right tools and comprehensive guidance, they are better equipped to manage their health proactively.
Final Thoughts: A Collective Responsibility to Improve Health Outcomes
As we step back and consider the many nerve-racking challenges that head and neck cancer patients face, it becomes clear that nutritional therapy is far more than a supplementary component of cancer treatment—it is a central pillar of overall care. The tiny yet critical details of nutritional planning, when managed correctly, can make the difference between a patient who thrives during treatment and one who is overwhelmed by the side effects.
In light of the evidence and expert opinions presented, it is essential for the medical community, policymakers, and society at large to take a stand. We must clear the labyrinth of confusing bits in nutritional care by fostering better research, empowering patients through education, and enacting policies that support comprehensive dietary services. By working through these fine points together, we have an opportunity to transform the current landscape of head and neck cancer care.
This transformation is not an isolated benefit. It promises to reduce the overall strain on our healthcare systems and improve the quality of life for countless individuals who face a daunting diagnosis every day. Improved access to registered dietitians and evidence-based nutrition strategies can serve as a catalyst for better treatment outcomes, enhanced recovery, and, ultimately, more lives saved.
In summary, the road toward better nutritional care for head and neck cancer patients is lined with both challenges and opportunities. The journey may be filled with tangled issues and nerve-racking moments, but every positive change in policy, research funding, and community outreach offers a new ray of hope. As we work to get around these challenging parts, each step forward will not only ease the burden on patients but also inspire a broader movement towards patient-centered, comprehensive healthcare.
It is upon all stakeholders—from healthcare providers and researchers to government officials and patient advocates—to find their way through these twists and turns. With a concerted effort, the future holds the promise of not just prolonged survival, but a marked improvement in the quality of life for those facing head and neck cancer.
Let us commit to this cause, invest in proper nutritional strategies, and make our way toward a future where every patient is empowered and every meal is a step toward recovery. Only through integrated action can we hope to turn the tide against the overwhelming nutritional challenges that lie in the path of head and neck cancer care.
In the end, the clear message is one of collective responsibility. It is not enough to simply treat the tumor; we must also treat the whole patient. The fine details of nutritional management can no longer be relegated to the background. They are, in every sense, super important to ensuring that our patients survive—and truly thrive.
Originally Post From https://www.kumc.edu/about/news/news-archive/head-and-neck-cancer-nutrition.html
Read more about this topic at
Nutrition During Cancer – NCI
Nutrition for the Person Getting Cancer Treatment
