Precision Medicine in Cancer Management: Promise and Realities
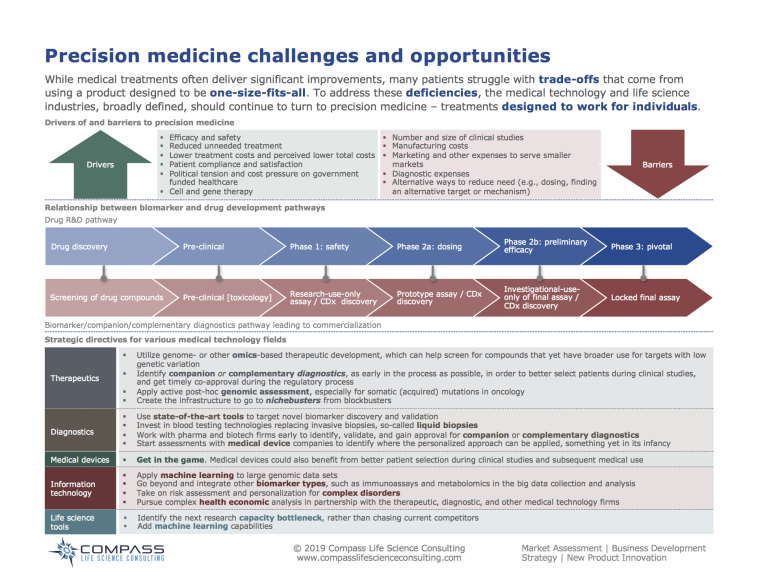
The rapid evolution of precision cancer care has sparked both excitement and concern among healthcare professionals and the broader public alike. In recent years, precision medicine has been celebrated for its potential to customize treatments based on the unique molecular data of an individual’s tumor, promising tailored therapies that could improve survival rates and quality of life. However, as with any emerging field, there are several twisted issues that deserve our careful attention. In this editorial, I take a closer look at the current state of precision medicine, its potential benefits, and the tricky parts that could impact broader public health initiatives.
Understanding the Core of Precision Medicine
Precision medicine, which focuses on the detailed examination of the genetic and molecular profiles of cancer, has become a super important pillar of oncology. It involves obtaining data from both tumor and germline sources, a process that is not only transformative in individual care but also a promising path for the future of cancer drug development. In many ways, this targeted strategy has already started to revolutionize patient outcomes, effectively reshaping the treatment landscape by moving away from traditional “one-size-fits-all” approaches.
Many proponents of precision medicine argue that the key to optimal cancer management is understanding the subtle details of each patient’s condition. With the advent of new technologies such as next-generation sequencing (NGS), healthcare providers can now identify actionable genomic biomarkers that often indicate a patient’s eligibility for targeted treatment or immunotherapy. This shift towards a more personalized approach holds the promise of not only extending survival but also enhancing the overall quality of life for many patients.
Drilling Down into the Key Advances
The following advancements illustrate how precision medicine is reshaping cancer care:
- Molecular Profiling: A clear focus on molecular data, enabling clinicians to pick the most suitable therapeutic strategy for the individual.
- Targeted Therapies: Approved treatments based on identified biomarkers allow for more specific cancer-fighting approaches.
- Screening and Prevention: Even the planning of preventive measures and screening strategies now benefits from genetic insights, broadening the scope of precision medicine beyond treatment alone.
However, while these advancements are impressive in their right, they also invite us to get into some of the tangled issues surrounding resource allocation and health policy. After all, if a large portion of healthcare funding is directed toward individualized treatments, what implications does this carry for broader public health strategies aimed at prevention and early detection?
Balancing Research Funding: Precision Medicine Versus Broader Public Health Strategies
The allure of precision medicine can often overshadow other equally essential approaches in cancer management, particularly those focusing on preventing cancer in the first place. It is important to note that while molecular-based treatments have garnered significant attention, public health measures such as reducing tobacco use, promoting human papillomavirus vaccinations, and implementing effective cancer screening remain critical in reducing the overall burden of malignant diseases.
Every healthcare system has limited financial and personnel resources. As such, it is nerve-racking to examine whether the prioritization of precision treatments might siphon off funds that would otherwise support vital public health initiatives. This situation isn’t about choosing one strategy over the other. Instead, it calls for a balanced approach where both precision-based treatments and population-based preventive measures work hand in hand.
Key Considerations in Funding Allocation
When balancing research funding, several subtle details need to be considered:
- Priority Setting: Agencies must thoughtfully prioritize funding to ensure that both innovative treatments and essential public health measures receive support.
- Cost-Benefit Analysis: With precision medicine often coming at a high cost, healthcare systems need to analyze whether these investments yield benefits that justify the reallocation of resources from prevention programs.
- Long-Term Impact: While immediate benefits of targeted therapies are highly visible in some cases, the long-term impact on cancer prevention and overall public health remains a critical factor in funding decisions.
This conversation is reminiscent of the cautionary insights provided by thinkers like James Tabery, who point out that many forces—be they technological, political, or economic—are pushing forward the agenda of personalized medicine. As profits and speed of research progress take precedence over a broader understanding of environmental factors, we risk creating a scenario where environmental determinants of health do not receive the same level of scrutiny and support.
Financial Implications and the High Cost of Molecular Diagnostics
While precision medicine holds enormous promise for those with advanced cancers, it is not without its nerve-racking financial challenges. One of the most significant obstacles is the high cost associated with molecular diagnostics, including next-generation sequencing tests. The tangible benefits of these tests are undeniable, yet they are underutilized in everyday clinical practice due to these very cost concerns.
A recent study highlighted that when comprehensive NGS testing was provided free of charge under a research protocol, a substantial number of patients benefitted from actionable biomarker detection. However, one must ask: How many patients are denied these potential benefits due to insufficient insurance coverage or third-party payment rejections?
Understanding the Economic Burden
Let’s take a closer look at several financial challenges:
- High Test Costs: Molecular diagnostics are expensive, and these costs can be overwhelming for many healthcare systems and patients alike.
- Insurance Reimbursement Issues: If insurers do not fully cover the cost of precision tests, doctors might be reluctant to order them, potentially denying patients life-saving targeted therapies.
- Disparities in Access: There is a real risk of creating a two-tiered system where only those with high economic means gain access to the latest precision medicine innovations while others rely solely on conventional care strategies.
These financial challenges underscore the need for decision-support tools that can help clinicians figure a path through the administrative and logistical hurdles associated with advanced testing. Without these tools, the full potential of precision medicine remains underexploited in routine clinical practice. As these costs and challenges loom, both physicians and patients are caught in a frustrating cycle that could hinder access to next-generation therapies.
The Underutilization of Molecular Diagnostic Tools
In many healthcare settings, the adoption of advanced molecular diagnostics such as NGS has not kept pace with its potential clinical benefits. Despite robust evidence supporting the effectiveness of molecular profiling in identifying actionable targets for cancer treatment, its routine utilization remains limited. This is largely due to the high cost of testing, coupled with an absence of user-friendly decision-support systems for clinicians.
Consider the following scenario: A robust system is in place where every patient with an advanced tumor undergoes immediate molecular profiling at diagnosis. In one such case study, nearly half the patients were found to have at least one actionable genetic marker that pointed toward a targeted treatment or was eligible for a clinical trial. For those patients tracked over six months, treatment with precision cancer therapeutics translated into notably better survival outcomes compared with conventional chemotherapy.
Barriers That Limit Routine Testing
Below are some of the tortured ways clinicians find it tough to integrate molecular testing into everyday practice:
- Lack of Decision-Support Tools: Many physicians struggle to interpret complex genomic data due to the absence of simplified, user-friendly analysis platforms.
- Cost Concerns: With testing expenses reaching critical levels, many clinicians hesitate to recommend these expensive procedures unless absolutely necessary.
- Reimbursement Worries: Even when evidence supports testing, physicians are often deterred by the potential challenges in securing third-party payment, leaving at-risk patients without access to this advanced testing.
- Time Constraints: The process of ordering, receiving, and analyzing genomic data can be intimidating and time-consuming, especially in busy clinical settings.
In summary, while precision diagnostic tools are gaining traction, the reality is that their widespread adoption is still hampered by financial and logistical barriers. This underutilization could mean that many patients who might benefit from personalized treatments are left without the opportunity for effective intervention until later stages of their disease.
Public Health Prevention and Precision Medicine: Complementary, Not Competitive
Amid the remarkable advances in precision medicine, the importance of mass-scale public health initiatives for cancer prevention must not be overlooked. Many public health strategies such as reducing tobacco consumption, increasing vaccination rates, and fostering healthy lifestyles continue to be essential building blocks in the fight against cancer. These preventative measures are not only effective but also cost-efficient when implemented at the population level.
The worry is that a heavy bias toward precision medicine could inadvertently lead to a shortage of funds and resources needed for prevention and early detection programs. For instance, while the development of CRISPR-based personalized treatments and other innovative therapies attracts significant attention (and hefty price tags), vital public health initiatives already proving their worth might end up on the back burner.
Key Points of Caution in Public Health Investment
It might be helpful to consider the following points when weighing investments between precision medicine and public health:
- Resource Allocation: It is essential for policymakers to ensure that funding is fairly distributed so that not only advanced therapies but also basic public health measures are sufficiently supported.
- Long-Term Preventive Value: Enhancing efforts in vaccination, tobacco cessation, cancer screening, and obesity management can lower the incidence of cancer, directly reducing treatment costs in the long run.
- Integration of Data: There is an opportunity to bridge the gap between precision medicine and public health by using molecular data to also inform population-wide screening and early detection strategies.
These points emphasize that the relationship between precision medicine and public health should be viewed as complementary rather than competitive. Understanding and investing in both areas can ultimately lead to an integrated approach that not only treats cancer more effectively but also reduces its incidence.
Real-World Challenges in Integrating Precision Medicine
Implementing precision medicine into clinical practice is full of problems that extend beyond the laboratory. While research settings have achieved significant breakthroughs—often because tests are provided at no cost—the real-world scenario is frequently more complicated. Clinicians frequently encounter practical hurdles that can delay or altogether prevent the adoption of precision technologies in everyday cancer care.
One of the most concerning challenges is that medical practitioners sometimes lack the proper infrastructure or support to manage the additional load associated with genomic testing. The financial, administrative, and even technical demands can feel overwhelming, especially in community and non-academic settings where resources are limited.
Challenges Faced in Routine Practice
Some of the twisted issues include:
- Financial Hurdles: The significant cost of genomic tests, factors that can make third-party payers hesitant, and an overall lack of reimbursement clarity.
- Administrative Complexities: Navigating the maze of insurance claims, verifying coverage eligibility, and managing patient expectations can be nerve-wracking tasks.
- Lack of Expert Guidance: Without the presence of dedicated decision-support tools or multi-disciplinary teams, many clinicians may struggle to interpret the nitty-gritty of genomic data.
- Variability in Health Systems: Not all healthcare institutions have the same level of access to advanced technology or specialized staff, leading to inconsistencies in patient care.
A deep dive into these challenges helps shed light on why many potentially life-saving tests are not performed routinely in everyday practice. It is therefore critical that health systems build robust support networks, fostering closer collaborations among oncologists, pathologists, and genetic counselors to ensure that the benefits of precision medicine are realized widely.
Addressing the Cost-Benefit Dilemma: A Call for Balanced Policies
The allocation of healthcare resources is, and always will be, a delicate balancing act. With precision medicine attracting considerable attention, there lies a real danger that resources might be disproportionately funneled into personalized therapies at the expense of broader, preventive initiatives. To avoid this outcome, it is crucial that policymakers work to steer through these challenges by crafting funding policies that embrace both innovative and traditional public health approaches.
For instance, ensuring that reimbursement systems are aligned with current clinical practices could help reduce the existing gap between the promise of precision diagnostics and their practical implementation in routine oncology care. Moreover, revisiting policies to offer better support for broad-based public health initiatives is equally important. In sum, policies need to be designed to complement the benefits of precision medicine with the unwavering importance of prevention strategies.
Strategies for Equitable Funding
Below are some strategies that could help manage the allocation of funds between precision medicine and traditional public health approaches:
- Integrated Funding Schemes: Establishing funds that are specifically allocated to projects that bridge precision medicine with population health initiatives.
- Subsidizing High-Cost Diagnostics: Government or public-private partnerships could help defray the costs of molecular tests, ensuring that all patients benefit rather than only those with robust insurance plans.
- Incentivizing Preventive Measures: Offering grants and funding towards innovative public health campaigns, including vaccination drives and early cancer screening, to ensure these programs receive the necessary support.
- Regular Assessment: Instituting regular reviews of resource allocation to ensure that both advanced genetic research and time-tested public health measures receive fair investment.
These strategies, when implemented effectively, can help create a balanced approach to tackling cancer—one that does not pit the promise of cutting-edge science against the pragmatic need for widespread prevention and early intervention.
Lessons from Research and Clinical Practice
Reports from various healthcare organizations have shown that when molecular diagnostics are seamlessly integrated into clinical pathways, patient outcomes can markedly improve. For instance, institutions that have set up protocols for immediate genomic testing at the time of a cancer diagnosis frequently report that nearly half of the patient population exhibits actionable genetic markers. These markers not only guide treatment decisions but also suggest eligibility for emerging clinical trials.
Furthermore, patients who have received molecularly targeted therapies often have seen improvements in overall survival compared with those who undergo conventional chemotherapy. Although these positive outcomes are encouraging, it is important to note that many of these studies are performed in controlled research environments where the costs of testing are not a barrier. In everyday practice, the nerve-wracking concern over who will foot the bill for these tests remains a significant hurdle.
Take-Away Points from Clinical Experience
It is useful to summarize the real-world lessons from integrating precision medicine into cancer care:
- Enhanced Survival Outcomes: When genomic testing is implemented, patients often benefit from personalized treatments leading to better survival statistics.
- Access Challenges: Despite the promise, the high cost and administrative issues result in uneven adoption of these tests across various healthcare settings.
- Systematic Investments Needed: Broadening the accessibility of NGS tests would require systematic changes including better reimbursement policies and the development of accessible decision-support tools.
- Holistic Healthcare Approach: A complementary strategy that combines the advanced precision approaches with effective public health interventions appears to be the most beneficial model.
The Way Forward: Integrating Innovation with Public Health
Given the significant potential of precision medicine in advancing cancer care, it is crucial to strike an effective balance between investing in innovative treatments and supporting long-established public health strategies. Instead of viewing these approaches as mutually exclusive, the goal should be to merge them in a way that leverages their combined strengths.
For healthcare professionals, patients, and policymakers alike, the challenge is to figure a path that allows the benefits of precision medicine to be accessible to as many patients as possible while ensuring that public health interventions continue to thrive. Only by harmonizing these two strategies can we hope to reduce the overall burden of cancer in our society.
What an Integrated Model Could Look Like
An ideal patient care model might incorporate the following elements:
- Unified Diagnostic Pathways: Routine inclusion of molecular diagnostics in standard care protocols across all treatment centers.
- Collaborative Decision-Making: Multi-disciplinary teams including oncologists, genetic counselors, and public health experts working together to create patient-centered care plans.
- Flexible Health Policy: Adaptive policies that account for both the high cost of precision treatments and the low-cost preventive strategies that yield significant long-term benefits.
- Patient Education Programs: Initiatives to educate patients on the benefits and limitations of both personalized cancer therapies and traditional prevention measures, ensuring fully informed decisions.
This blended approach not only maximizes the benefits of technological and scientific breakthroughs but also reinforces the foundation of public health that has long been essential to reducing cancer incidence on a broad scale.
Concluding Reflections: A Shared Future for Cancer Care
In summary, the expanding role of precision medicine in cancer management is a double-edged sword that brings with it both the promise of personalized patient care and a set of tricky parts that need careful oversight. The high cost of advanced molecular diagnostics, disparities in patient access, and the potential for diverting funds from proven public-health measures are all issues that require continuous attention and balanced solutions.
It is clear that precision medicine has already changed the landscape of oncology, demonstrating remarkable benefits in individual patient outcomes. At the same time, ensuring that these advances do not come at the expense of population-wide preventive strategies is a challenge that future policymakers and healthcare providers must address head-on.
While there is no simple fix to these conflicting interests, the ongoing dialogue among all healthcare stakeholders—from clinicians and researchers to policymakers and patients—offers hope for a more integrated system. By fostering collaboration, understanding the hidden complexities of both individual care and public health, and making thoughtful policy decisions, we can build a future where personalized treatment and widespread prevention are not at odds but rather work as twin pillars of a comprehensive cancer care system.
Final Thoughts and the Road Ahead
In my view, the key to the future of cancer management lies in our ability to blend innovation with a strong foundation in public health. Every advancement in molecular diagnostics must be matched by initiatives that ensure equitable access and financial support for all patients, regardless of their socio-economic background. As we stand on the brink of further developments in precision oncology, the onus is on us—as a community, as healthcare providers, and as policymakers—to make sure that our pursuit of advanced treatments does not blind us to the critical importance of prevention and early detection.
In closing, while the road ahead is undoubtedly loaded with challenges and confusing bits, the potential rewards are too significant to ignore. Let us work together to build a healthcare system that not only pushes the boundaries of what personalized medicine can achieve but also remains firmly committed to the tried-and-true principles of public health. Only then can we truly say that we are addressing the full spectrum of cancer care—from innovative treatments to comprehensive prevention strategies, ensuring the best possible outcome for all patients.
Summary of Key Points
| Area of Focus | Key Challenges | Potential Solutions |
|---|---|---|
| Precision Diagnostics |
|
|
| Public Health Initiatives |
|
|
| Healthcare Policy |
|
|
By integrating such strategies and keeping an open dialogue on these important issues, the healthcare community can ensure that precision medicine does not eclipse public health efforts—each supporting the other for a truly healthier future.
As we move forward into an era characterized by both extraordinary technological advances and age-old public health challenges, it is essential that we continuously rethink, reassess, and rebalance our priorities. Whether you are a clinician, researcher, policymaker, or patient, the conversation about precision cancer care and its connection with broader public health measures is one we must all actively engage in.
Ultimately, the vision we set today for integrating precision medicine with comprehensive cancer prevention and management strategies will shape the future of oncology for generations to come. Let us take this challenge as an opportunity—to work together, to innovate responsibly, and to ensure that every patient benefits from the best of both worlds: groundbreaking personalized treatments and strong, community-based prevention programs.
Originally Post From https://www.onclive.com/view/a-closer-look-at-issues-with-the-expanding-role-of-precision-medicine-in-cancer-management
Read more about this topic at
Patients’ perspectives related to ethical issues and risks in …
Patients’ and professionals’ views related to ethical issues in …