Osteoporosis Treatment After Fragility Fracture: A Critical Step in Improving Health Span for the Elderly
The recent observational study presented at ENDO 2025 highlights that initiating osteoporosis treatment in patients aged 80 and older following a fragility fracture is associated with a significant reduction in both hospitalization and all-cause mortality over a 5-year period. As our aging population continues to grow, understanding the benefits of early intervention and the appropriate management for osteoporosis becomes increasingly essential, offering hope to millions of seniors and their families.
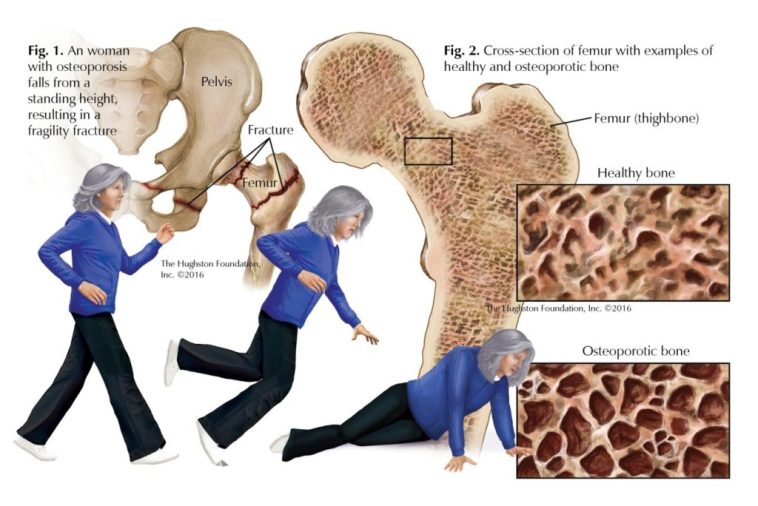
Understanding Fragility Fractures in the Elderly and Their Consequences
Fragility fractures, most commonly seen in the hip or vertebra, represent one of the most intimidating complications of osteoporosis in older adults. These fractures are not only painful but also carry the potential for long-term disability and an increased risk of premature death. The study in question examined over 130,000 patients, highlighting a scenario where the risk of hospitalization and mortality was reduced among those who started treatment immediately after a fracture. This evidence reinforces the notion that timely osteoporosis management can help address the tricky parts of post-fracture care and reduce the overall burden on both individuals and healthcare systems.
Deep Dive into the Study: How Osteoporosis Treatment Leads to Better Outcomes
The research conducted by the Cleveland Clinic using the TriNextX database offers a detailed look at how treatment protocols can influence outcomes in seniors. In this study, patients aged 80 and older who had experienced a fragility fracture were grouped into two cohorts: those who received osteoporosis treatment and those who did not. After adjusting for differences using propensity score matching—a process that helps balance out the complicated pieces of patient baseline characteristics—the results revealed statistically significant reductions in both hospitalizations and all-cause mortality in the treatment group.
This finding is important because it sheds light on how well-managed treatment regimens, including bisphosphonates, denosumab, raloxifene, and teriparatide, can make a key difference. When healthcare providers take a closer look at these drugs and their impact, they can figure a path toward reducing the overall risk of severe outcomes, making life a bit easier for elderly patients who are often facing off-putting medical challenges.
Osteoporosis Management Post-Fragility Fracture: Long-Term Benefits in the Elderly
One of the standout points from the study is the encouragement it provides for adopting early treatment strategies after a fragility fracture. In an aging population, every prevented hospitalization and saved life counts. The observational data suggests that beginning treatment as soon as possible offers a protective effect that can extend well beyond the initial recovery period.
For many seniors, the road to recovery from a fracture can be nerve-racking and overwhelming, with many tangled issues arising along the way. However, when critical osteoporosis treatment is promptly initiated, not only does it help in stabilizing the bones, but it also plays a significant role in reducing risks associated with further hospital admissions and potential complications that may lead to mortality. This study invites us all to look into the fine points of osteoporosis management and consider the long-term benefits that extend far beyond the immediate post-fracture phase.
Comparing Treatment Modalities: Bisphosphonates and Beyond
Modern osteoporosis care provides a range of treatment options tailored to individual patient needs. Clinicians have the choice among several medications with varying mechanisms of action. For example, bisphosphonates work by inhibiting bone resorption, helping to maintain bone density, whereas medications like denosumab and teriparatide take different approaches in preserving bone health. Each option comes with its own set of subtle parts that require close examination.
Below is a bullet list summarizing key treatment options:
- Bisphosphonates: Often considered the standard first-line treatment due to their effectiveness in preventing further bone loss.
- Denosumab: Works by altering the cells responsible for bone resorption, offering an alternative for those who cannot tolerate bisphosphonates.
- Raloxifene: A selective estrogen receptor modulator that not only improves bone density but may also offer cardiovascular benefits.
- Teriparatide: An anabolic agent that actually stimulates new bone formation, ideal for patients with severe osteoporosis.
Each of these medications has its own set of fine shades in terms of administration, side effects, and interactions with other conditions. The choice of treatment should therefore be built on a detailed understanding of the patient’s overall health status and risk factors. Doctors are encouraged to work through these little twists with their patients, ensuring that each step in the treatment process is clearly explained and that potential benefits are well-defined.
Observational Studies and Their Role in Guiding Clinical Practice
In today’s medical landscape, observational studies serve as an invaluable source of real-world evidence. Unlike randomized controlled trials, which can sometimes feel overwhelming and full of problems, observational research offers insights that are directly applicable to everyday clinical practice. The study presented at ENDO 2025 is a prime example of how data from a large patient registry can provide a clearer picture of treatment outcomes in a real-world setting.
The findings underscore that when the risk factors for subsequent hospitalizations and mortality are carefully managed, osteoporosis treatment can play a transformative role in extending health span. This is particularly significant for the elderly, for whom a fragility fracture can often act as a turning point in overall health deterioration. Through this observational lens, clinicians can poke around the outcomes and deduce that starting treatment is not merely a precaution but a necessity for promoting healthier aging.
Spotlight on the Elderly: When Every Day Counts
The notion of “health span” is emerging as a key goal in modern medicine, particularly in the context of an aging population. Health span refers to the number of years a person lives in good health, free from the limiting effects of chronic diseases and hospitalizations. For many seniors who are recovering from a fragility fracture, every day counts. The study’s demonstration of reduced hospitalization risk and lower mortality rates offers robust evidence supporting the proactive treatment of osteoporosis, suggesting that such measures not only prolong life but also improve the quality of life.
In this light, it is super important for healthcare providers to take into account both the immediate benefits and the long-term gains of starting osteoporosis treatment promptly. A structured protocol that focuses on early diagnosis, timely intervention, and continuous monitoring can significantly boost a patient’s ability to maintain independence and reduce the risk of further complications.
Breaking Down the Clinical Barriers: Tackling the Tricky Parts of Osteoporosis Treatment in Seniors
Despite the evidence supporting early treatment, there are still many confusing bits and tricky parts that complicate the decision-making process in elderly patients. Some of these include concerns about potential side effects, the complexity of medication regimens, and the need for routine monitoring. Often, both patients and healthcare providers can feel overwhelmed when faced with a new diagnosis or treatment regimen, especially given the nerve-racking prospect of managing multiple health issues simultaneously.
It is essential to work through these tangled issues by enhancing patient education, fostering clear communication, and employing shared decision-making. By taking the wheel and empowering patients with the right information, clinicians can help mitigate fears and highlight the long-term benefits of treatment. This balanced approach can effectively reduce hesitation, ensuring that all concerned parties understand the clear advantages of initiating treatment after a fragility fracture.
The Impact of Osteoporosis Drugs on Hospitalization and Mortality Rates: Analyzing the Data
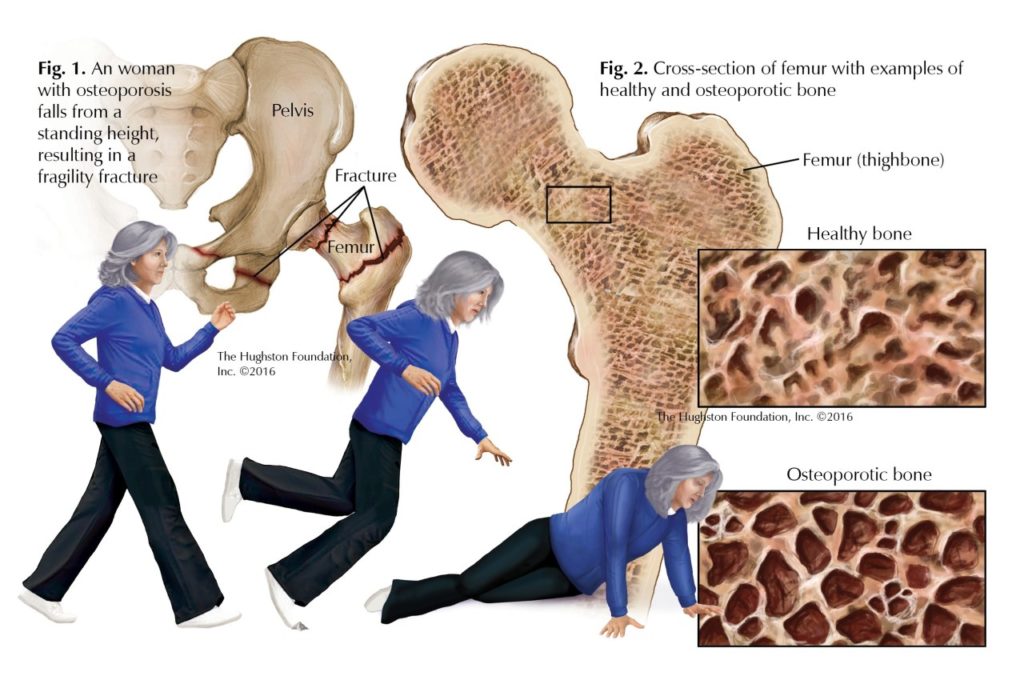
One of the most encouraging aspects of the study is the statistical association between osteoporosis treatment and reduced rates of hospitalization and mortality. Specifically, the odds ratios indicate that treated patients experienced a significant decline in the risk of hospitalization (OR, 0.814) and all-cause mortality (OR, 0.850) over a period of 5 years. These numbers provide compelling evidence for clinicians to consider immediate and consistent treatment interventions following a fracture.
This association is particularly important given the vulnerable nature of the elderly population. For many seniors, a fragility fracture can trigger a cascade of subsequent medical events that can destabilize an already delicate balance of health. By intervening early with osteoporosis treatment, healthcare providers can offer a buffer against these nerve-racking complications.
A helpful way to visualize these benefits is to consider the following table outlining key outcomes in treated versus untreated patients:
| Outcome | Treated Patients | Untreated Patients |
|---|---|---|
| Hospitalizations within 5 Years | 18,142 | 20,385 |
| All-Cause Mortality within 5 Years | 11,073 | 12,479 |
| Odds Ratio for Hospitalization | 0.814 (95% CI: 0.792-0.836) | |
| Odds Ratio for Mortality | 0.850 (95% CI: 0.825-0.876) | |
This table illustrates the clear differences in outcomes and reinforces the importance of making the decision to start treatment as soon as a fragility fracture is identified. While the numbers might appear abstract, they reflect very real benefits that translate into fewer hospital stays and, more importantly, an increased chance of survival.
Patient Perspectives: Addressing Concerns and Building Confidence in Osteoporosis Treatment
From a patient’s point of view, the prospect of additional medications after already suffering a fracture can be intimidating. Many seniors are cautious about starting a new regimen and may worry about the side effects or interactions with other medications. It is important for clinicians to sort out these hurdles through honest conversations and by providing clear, supportive information.
Transparency about the potential risks and rewards allows patients to make informed decisions. Here are some key points that practitioners can discuss with their patients when considering osteoporosis treatment:
- Understanding the Benefits: Explain that the evidence shows a significant reduction in both hospitalizations and overall mortality when treatment is started promptly.
- Side Effect Management: Address potential side effects head-on and offer solutions or monitoring strategies that ensure patient safety.
- Simplifying Medication Regimens: Work with the patient to create a simple, manageable schedule that integrates well with their daily routine.
- Continuous Monitoring: Emphasize the importance of regular follow-ups, which help to tailor the treatment plan as needed and to ensure optimal outcomes.
By handling these discussions with care and compassion, clinicians can help patients overcome the overwhelming feeling that often accompanies new treatment decisions. This approach not only builds trust but also equips patients with the confidence to stick with their treatment plan over the long haul.
Clinical Implications: How This Study Informs Future Healthcare Practices
The outcomes of this study have several important implications for clinical practice. First, they reinforce the concept that treatment need not be delayed—even in the face of difficult decisions—for the sake of reducing hospitalization and mortality risks. This message is crucial for healthcare systems worldwide, which are continually seeking ways to reduce the financial and emotional burdens associated with elderly care.
Health professionals are encouraged to take a closer look at this data, digest the fine shades of the research findings, and integrate these insights into everyday practice. By adopting a proactive rather than reactive approach, clinicians can significantly improve the quality of care delivered to elderly patients. This means incorporating osteoporosis treatment as a standard step in the management of patients after a fragility fracture, rather than waiting until complications arise.
Moreover, the study underscores the importance of patient-specific treatment planning. Not every elderly patient will have the same risk factors or respond similarly to treatment. Therefore, personalized medicine—where therapies are tailored to individual needs—remains a super important strategy. By considering factors such as a patient’s overall health, concurrent medications, and personal treatment goals, clinicians can design a treatment plan that optimally reduces risk and enhances overall health outcomes.
Addressing the Tangled Issues of Treatment Adherence and Follow-Up Care
Even with the most promising data in hand, ensuring that patients adhere to their treatment regimens remains one of the most challenging tasks in managing osteoporosis. Carefully balancing medication schedules, managing side effects, and handling regular follow-up appointments can sometimes be nerve-racking for elderly patients who might already feel bombarded by their other health issues.
To address these challenges, healthcare providers must work through several strategies that cover both medical and psychosocial aspects of care. These include:
- Patient Education Initiatives: Providing clear, simplified instructions and the reasons behind each treatment component can help patients feel less overwhelmed.
- Regular Follow-Up Reminders: Implementing reminder systems via phone calls, emails, or texts can help patients stick to their visits and keep track of their progress.
- Involving Caregivers: When family members or caregivers are involved, there is often an improved understanding and adherence to the treatment plan.
- Integrating Technology: The use of health apps and online portals allows patients to monitor their condition, thus encouraging a greater sense of responsibility and engagement.
These strategies collectively help to minimize the small distinctions in treatment adherence that might otherwise lead to suboptimal outcomes. By establishing a robust support system, patients are better positioned to manage their care and harness the full benefits of osteoporosis treatment.
Long-Term Outcomes: Improving Life Quality Beyond Hospitalization and Mortality Rates
The benefits of osteoporosis treatment extend far beyond the immediate reduction in hospital stays and mortality risk. For many seniors, being able to maintain independence and enjoy their daily activities without constant fear of another fracture is of immeasurable value. While the study quantifies the reduction in hospitalization and death, the broader impact on quality of life sheds light on additional, more subtle benefits.
Key aspects of improved quality of life include:
- Enhanced Mobility: Effective treatment helps stabilize the bones, improving mobility and reducing the risk of subsequent falls.
- Better Pain Management: With fewer fractures and complications, patients experience less chronic pain, which is often a significant barrier to daily activity.
- Greater Independence: Reduced hospitalizations mean that seniors can spend more time at home, maintaining routines and social connections that are critical for emotional well-being.
- Improved Mental Health: The reduction in the nerve-racking prospect of future fractures can alleviate anxiety and depression that often accompany chronic illness.
Ultimately, when osteoporosis treatment is implemented effectively, it can significantly contribute to a more fulfilling and independent life for older individuals. This broader perspective on health outcomes is crucial for policymakers and healthcare providers alike, as it reinforces that the decision to initiate treatment has repercussions that echo throughout everyday life—not just in the hospital corridors.
Future Directions: Enhancing Research and Personalized Osteoporosis Management
While the study discussed here provides robust evidence supporting the benefits of osteoporosis treatment in reducing hospitalizations and mortality, there are still many confusing bits and hidden complexities that remain to be explored. Future research may focus on:
- Comparative Effectiveness Studies: Research comparing the long-term outcomes among different osteoporosis drugs can provide deeper insights into which therapy might be best suited for particular patient profiles.
- Quality of Life Assessments: Further studies can explore not only the quantitative benefits in terms of survival and hospitalization rates but also the qualitative improvements in daily life.
- Pharmacogenomics: Understanding how genetic factors influence a patient’s response to specific treatments could pave the way for truly personalized osteoporosis care.
- Integrated Care Models: Research into multidisciplinary care approaches that integrate osteoporosis treatment with other aspects of elderly care could help devise strategies to manage the tangled issues of multiple comorbidities.
As we take a closer look at the future possibilities, it becomes clear that there is still much to learn about the fine points of osteoporosis treatment. However, studies like the one presented at ENDO 2025 are paving the way, offering substantial evidence that early and aggressive management can yield benefits extending well beyond the immediate post-fracture recovery period.
Bridging the Gap Between Research and Everyday Clinical Practice
The translation of research findings into everyday practice is not always straightforward. Clinicians must often figure a path through a maze of tangled issues, from insurance hurdles and patient adherence to the nerve-racking side effects of medications. Despite these challenges, the robust findings of this study indicate that the benefits are too significant to ignore.
To bridge this gap, it is essential to:
- Educate Healthcare Providers: Seminars, continuous medical education (CME) programs, and professional conferences can help update practitioners on the latest evidence-based practices.
- Streamline Clinical Guidelines: National and international guidelines should incorporate study findings to provide clear, actionable recommendations regarding the timing and nature of osteoporosis therapy after a fracture.
- Enhance Interdisciplinary Collaboration: Rheumatologists, endocrinologists, primary care physicians, and other specialists need to cooperate closely to provide coordinated care that maximizes treatment benefits.
- Engage Patients Through Shared Decision-Making: By involving patients in the decision-making process, clinicians can ensure that treatment plans align with the patient’s lifestyle preferences and overall health goals.
Ultimately, integrating these strategies into everyday clinical practice will require both systematic policy changes and a cultural shift within the healthcare community regarding the importance of timely intervention. With these steps, we can work through the confusing bits of treatment implementation, ensuring that every elderly patient has the best possible chance of a healthier future.
Embracing a Proactive Approach to Osteoporosis in an Aging Society
The study’s findings underscore a critical message: starting osteoporosis treatment immediately after a fragility fracture is more than just an option—it is an essential, proactive step toward preserving the health and independence of our seniors. In an era where the aging population is expanding rapidly, and healthcare resources are increasingly stretched, such proactive measures can ultimately help reduce the overall burden on our healthcare systems.
For healthcare providers, this means not waiting until a patient’s condition becomes overwhelming or off-putting. Instead, the focus should be on early intervention, proactive discussion, and careful monitoring. By doing so, practitioners can significantly improve long-term outcomes and ensure that seniors are not left to face the nerve-racking consequences of untreated osteoporosis.
Concluding Thoughts: A Call to Action for Healthcare Providers and Policymakers
In summary, the recent study presented at ENDO 2025 offers robust evidence that osteoporosis treatment after a fragility fracture among patients aged 80 and older is associated with reductions in both hospitalization and all-cause mortality. These findings illuminate the benefits of early intervention and highlight how a well-managed treatment strategy can improve the overall health span of our elderly population.
As clinicians, it is our responsibility to not only take these findings to heart but also to integrate them into our daily practice. By educating ourselves and our patients, streamlining treatment protocols, and working closely with interdisciplinary teams, we can manage our way through the tricky parts of post-fracture care and substantially reduce the risks associated with osteoporosis.
For policymakers and healthcare administrators, these results call for a re-examination of current treatment guidelines and the allocation of resources to ensure that every elderly patient has access to timely, high-quality osteoporosis care. Investment in education, research, and integrated care models is key to making the clinical gains of studies like this accessible to all who can benefit.
It is clear that the journey to better health for our seniors is not without its twists and turns. However, with evidence-based guidelines and a commitment to proactive patient care, we have the tools to reduce the hospitalization and mortality risks associated with osteoporosis. In doing so, we help our elderly population lead fuller, healthier lives—a goal that is both super important and heartening to embrace as we move forward in modern medicine.
Key Takeaways for Healthcare Providers:
- Immediate osteoporosis treatment following a fragility fracture significantly reduces hospitalization and mortality risks.
- A range of treatment options, including bisphosphonates, denosumab, raloxifene, and teriparatide, offer super important benefits tailored to the elderly.
- Personalized treatment planning and proactive patient education can help address the nerve-racking challenges encountered in managing osteoporosis.
- Observational studies provide real-world insights that can steer clinical practice towards more effective, patient-centered care.
- Integrating research findings into everyday clinical practice requires coordinated efforts from healthcare providers, policymakers, and educators.
In light of the evidence presented and the profound benefits observed, now is the time to take a closer look at how we manage osteoporosis in our aging population. Through targeted interventions and a commitment to improving health span, we can transform the care landscape for elderly patients, turning what was once a nerve-racking prospect into a manageable, even optimistic journey toward better health.
As we continue to work through the challenges posed by an increasingly elderly society, let us remember that every small distinction in treatment adherence and every well-informed decision can make a significant difference in patients’ lives. The study’s findings are not merely numbers on paper but a clarion call to action—one that we must heed for the sake of our seniors and for the future of compassionate, effective healthcare.
Ultimately, by embracing a proactive approach to osteoporosis treatment, we are not just treating a disease—we are preserving independence, enhancing quality of life, and affirmatively shaping the future of elderly care. With rigorous research, comprehensive patient education, and a willingness to work through the tangled issues of healthcare management, we have the opportunity to effect real, lasting change in the lives of those we serve.
As healthcare professionals, let’s commit to taking the wheel and ensuring that every elderly patient receives the timely, effective care they deserve. The path may be filled with confusing bits and intimidating challenges, but the rewards—improved health, reduced hospitalizations, and a longer, more vibrant life—make every effort worthwhile. It is a journey worth embarking on, one thoughtful decision at a time.
Originally Post From https://www.endocrinologyadvisor.com/reports/osteoporosis-treatment-after-fragility-fracture-lowers-mortality-risk/
Read more about this topic at
Summary – Medications for Opioid Use Disorder Save Lives
Treatment Using Medication for Opioid Use Disorder Can …