Cancer Diagnosis: Transforming the Weight of the C-Word
The phrase “you have cancer” carries immense power. When doctors utter these words, they do more than convey a medical fact—they set off a chain reaction of emotions, expectations, and decisions. In modern oncology, the impact of a cancer diagnosis is loaded with hidden complexities that influence treatment choices, often leading patients toward aggressive interventions even when a more measured response might be just as effective.
Historically, cancer was a secret, spoken in hush tones; today it is a rallying cry. We must ask ourselves: Has the battle against cancer become a fight against the label itself? And does this label unintentionally push patients into nerve-racking treatment decisions?
Cancer Diagnosis and the Power of Language
The Weight of Speech: Illocutionary Force in Medical Communication
Drawing on J.L. Austin’s theory of speech acts, it becomes clear that words are not neutral carriers of information. Instead, they perform actions. For instance, when a patient is told “you have cancer,” the statement not only identifies a disease but also assigns a role—transforming the patient into a warrior expected to fight. This effect, sometimes known as the “fighter effect,” imposes a new identity that can lead to aggressive treatment strategies even in cases where a watchful waiting approach might be preferable.
Consider two hypothetical scenarios: In one, a patient is informed of a yellowish benign lesion that poses minimal risk. In another instance, a lump in a more sensitive area is labeled as “cancer.” Even if both conditions share similar low-risk profiles, the label “cancer” can transform a manageable condition into an intimidating battle, with patients and doctors alike leaning toward immediate treatment. It is clear that the words we use can set a narrative that is both compelling and troubling.
How Labels Create Roles: The Fighter Effect Explained
The fighter effect is a prime driver of overtreatment. The term “cancer” doesn’t merely serve as a diagnosis. Instead, it sends an unspoken command: “fight,” “battle,” and “conquer.” These expectations can make patients feel that any form of non-intervention is equivalent to giving up. When faced with a low-risk prostate cancer or ductal carcinoma in situ (DCIS) in the breast, many patients opt for aggressive treatments like surgery or chemotherapy simply because they have been conditioned to respond with a heroic battle stance.
This response is driven by two main factors:
- Emotional Pressure: Patients are bombarded with messages that equate strength with the willingness to fight hard against an enemy that, by its very name, calls for action.
- Medical Culture: Doctors, influenced by ingrained medical traditions and patient expectations, may also feel compelled to act even when less invasive strategies are available.
The combination of these pressures has resulted in a situation where too many patients experience unintended, and sometimes damaging, aggressive interventions.
Shifting the Narrative Through Reframing
Reframing the Fight: Changing Social and Medical Conventions
One promising alternative to fighting the overtreatment problem is not to rename cancer but to reframe the story that the word “cancer” tells. Instead of insisting on a militant and aggressive response, health professionals and public health campaigns could work to alter the cultural narrative. Reframing means addressing the tricky parts of language use directly by emphasizing measured decision-making over fear-induced action.
Rather than hiding behind euphemisms, reframing works to change how patients and clinicians think about a cancer diagnosis. This approach involves:
- Educating Patients: Providing clear, balanced information about risks and benefits empowers patients to make decisions based on the small distinctions between treatment options rather than a forced fight mentality.
- Modifying Medical Communication: Doctors can lessen the inevitable alarm by using language that acknowledges a patient’s autonomy and the availability of less aggressive options where appropriate.
- Crafting Public Health Campaigns: Shifting away from slogans like “fight like hell” to messages that focus on understanding the disease, managing expectations, and emphasizing quality of life.
By rethinking these messages, we can help reduce the hidden pressure to “fight” and instead allow patients to make a well-considered choice about treatment intensity.
The Role of Cultural Expectations in Treatment Decisions
Our social and cultural milieu plays a key role in how cancer is perceived and treated. In a society increasingly obsessed with immediate results and heroic battles, cancer is seen not as a medical condition to be managed with careful thought but as a crisis that demands urgent, decisive action. This cultural backdrop can lead both patients and providers to choose treatments that are more aggressive than necessary.
For example, consider the management of early-stage prostate cancer in the United States: Over half of those diagnosed with a low-risk variant still undergo invasive procedures such as surgery or radiation. Yet multiple studies have shown that the outcomes of observation are comparable, with the added benefit of avoiding the risky side effects—like incontinence and erectile dysfunction—that come with aggressive treatments.
Similarly, in early breast lesions such as DCIS, nearly all patients are pushed toward surgery, and a significant number even opt for mastectomies. Despite clinical trials that support more conservative management, the societal expectation to “remove the enemy” at all costs remains deeply entrenched. These examples highlight how the language and cultural imagery associated with cancer shape treatment decisions in ways that may not always serve the patient’s best interests.
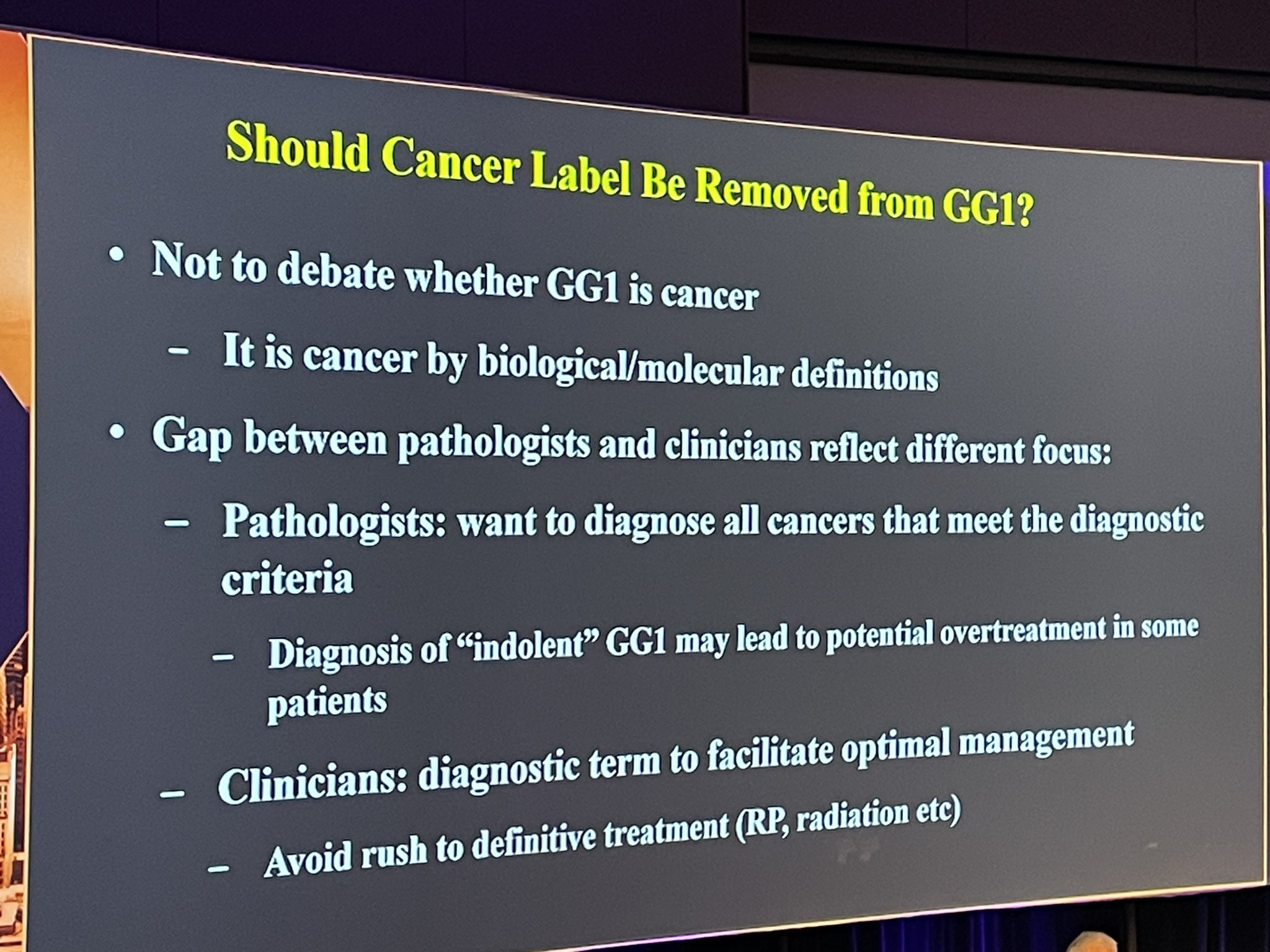
The Controversy of Renaming Cancer
Renaming Versus Reframing: A Comparative Exploration
A contentious debate in modern oncology involves whether early cancers should be renamed. Proponents of renaming argue that dropping the “dreaded C-word” could alleviate the overwhelming pressure to fight. They propose new terms such as “indolent lesion of epithelial origin” (IDLE) to describe certain low-risk conditions. The idea is that without the intimidating label of cancer, patients may be more open to less aggressive management.
However, critics of renaming raise several concerns:
| Issue | Renaming | Reframing |
|---|---|---|
| Patient Autonomy | May feel like deception, undermining trust once the truth surfaces. | Empowers patients with transparent information and balanced choices. |
| Effectiveness | Might reduce immediate fear but does not address the underlying cultural pressure to act aggressively. | Targets and reshapes the social narrative, creating long-lasting change. |
| Robustness | New labels can appear contrived and might prompt further questions about what constitutes “real” cancer. | By directly challenging the default fighter mindset, reframing creates a more resilient strategy. |
Ultimately, while renaming avoids the visual and psychological impact of the word “cancer,” it may simply shift the problem rather than eliminating the societal assumptions that drive overtreatment. In contrast, reframing offers a way to address these tangled issues at their source.
Respecting Patient Autonomy: The Case for Transparent Communication
Critics also argue that renaming can come off as patronizing. Imagine offering a dish to a friend who despises a particular ingredient and renaming it to something unfamiliar just to get them to eat it. That might work for a small child, but for an informed adult, it feels deceptive. Patients deserve to make informed decisions about their care based on honest discussions about the risks and benefits of each option.
Healthcare providers must work to make the sometimes intimidating language of diagnosis more digestible. By using everyday language that respects a patient’s ability to understand the fine points of their condition, physicians help patients figure a path that is tailored to their individual preferences and health status. An honest conversation that lays out the small distinctions between treatment approaches, along with their likely outcomes, can go a long way toward ensuring that patients do not feel forced down an unnecessarily aggressive path.
Changing the Medical Culture: A Roadmap for the Future
Altering Treatment Norms and Expectations
The current healthcare climate often seems to favor action for the sake of action. When a diagnosis is given, inertia is rarely an option—the default response is to push for immediate intervention. The challenge is to shift this mindset by introducing language and cultural practices that encourage careful consideration over knee-jerk reactions.
Key strategies for achieving this transformation include:
- Training and Education for Clinicians: Medical professionals should receive guidance on how to discuss diagnoses calmly without invoking the militaristic language that can trigger a fighter mindset.
- Patient-Centered Communication: Physicians should offer clear explanations of what each term means in real-life terms, helping patients understand the tricky parts of their treatment decision without resorting to pathos.
- Revised Public Health Messaging: Campaigns that promote early detection and treatment must also inform the public about subtle risks related to overtreatment. Instead of issuing rallying cries, these campaigns can highlight balanced decision-making.
Such changes in communication styles could help decouple the association between “cancer” and an automatic call to arms, reducing the likelihood that patients will face nerve-racking and unnecessarily aggressive treatments.
Empowering Patients to Make Informed Choices
At its core, the goal is to enable patients to decide on their own terms how best to manage their condition. When a patient learns that their so-called “lesion”—a condition that, in many cases, poses little threat—was labeled as cancer in the past, it can erode trust in the medical system. Instead of misleading patients with new labels, a more honest, supportive dialogue is needed.
Empowerment comes from transparency. Patients should be provided with:
- Accurate, complete information about their condition.
- An explanation of the subtle differences between various treatment options, including the hidden risks involved in each approach.
- Support in understanding that choosing a more conservative treatment or even palliative care does not equate to surrender.
By clarifying these tangled issues and reducing the overwhelming pressure to “fight” at all costs, the medical community can help patients steer through the confusing bits of cancer decision-making and feel confident in their choices.
Long-Term Impacts of Aggressive Cancer Treatment
The Hidden Costs: Quality of Life Versus Extended Treatment
There is a price to pay for overtreatment. Aggressive interventions—complicated pieces of medical practice that often focus on removing every trace of disease—can take a heavy toll on a patient’s quality of life. The side effects of chemotherapy, invasive surgeries, and prolonged hospital stays can lead to a host of challenges, including:
- Physical discomfort and persistent side effects like nausea and fatigue.
- Emotional stress and anxiety resulting from the relentless pressure to remain in a constant state of battle.
- Loss of time with loved ones as treatments and recovery interfere with daily life.
Recent estimates indicate that many patients with advanced cancer endure aggressive treatments in the final months of life. Studies show that one in three patients receive intensive interventions, while nearly one in five face chemotherapy in their final weeks. These aggressive measures rarely extend life in a meaningful way, and they frequently diminish its quality, leaving both patients and families coping with the enduring consequences.
The trade-off between the pursuit of life-extending treatments and preserving quality of life is one of the most challenging issues in modern cancer care. The pressure induced by the battle narrative forces both patients and clinicians to opt for immediate action rather than a thoughtful weighing of benefits versus costs.
The Social and Financial Dimensions of Overtreatment
Beyond the individual, overtreatment imposes a significant burden on health systems and society as a whole. The hidden financial costs include not only the expense of unnecessary procedures but also the long-term social cost of diminished quality of life and productivity. Studies indicate that overtreatment drains billions from healthcare systems every year.
Consider a few aspects:
- Economic Pressure: Unwarranted aggressive treatments put a strain on healthcare budgets and drive up insurance costs for everyone.
- Resource Allocation: When unnecessary treatments are administered, resources that could benefit patients with high-risk and aggressive cancers are diverted to low-risk cases.
- Emotional Toll: The societal expectations to fight simply because one is labeled a “cancer patient” can lead to widespread anxiety and stress, affecting not only individuals but also communities.
By rethinking the language used in cancer diagnoses and treatment decisions, we could potentially reduce these social and financial costs. A more carefully calibrated approach that emphasizes quality of life over a reflexive battle may ultimately prove more sustainable for both patients and the broader healthcare system.
Redefining the Cancer Journey: Toward a Balanced Approach
Empowering Narrative Change in Oncology
Changing the narrative around cancer is not about undermining its seriousness or the need for early detection. Rather, it is about enhancing patient autonomy and ensuring that decisions are driven by clear, balanced reasoning instead of compelling slogans and culturally ingrained expectations. The idea is to shift from a binary mindset—one where patients are either warriors or failures—to one where the real focus is on individual well-being and informed choice.
Taking a closer look at the journey, patients should be seen not just as fighters, but as individuals capable of understanding and managing the twists and turns of their own treatment pathways. Healthcare providers must work through these tangled issues by clearly explaining the fine points of each available option, thereby allowing the patient to decide which path suits them best, free from the heavy burden of a predefined “fighting” label.
Cancer Treatment Choices: Embracing a Spectrum of Options
A patient diagnosed with a low-risk cancer should not feel forced into choosing an aggressive remedy if a more conservative approach offers similar outcomes. In practice, this means encouraging a discussion that includes:
- A realistic appraisal of the risks and benefits of each treatment option.
- Consideration of the side effects and how they might impact daily life.
- A discussion of the patient’s personal values and goals, ensuring that decisions are made from a place of informed choice, free from societal pressure.
The goal should be to empower patients to figure a path that is flexible and tailored to their unique circumstances, rather than one that forces them into a binary win-or-lose scenario. When patients are given the space to choose, they can move forward at a pace that preserves both their health and their dignity.
The Future of Cancer Communication: Steps Toward a New Norm
Integrating Reframed Communication in Clinical Practice
Transitioning to a reframed approach in cancer care will not happen overnight. It requires coordinated efforts across multiple fronts—clinical training, patient education, and public health messaging need to evolve in tandem. Medical schools and continuing education programs must take up the challenge of teaching upcoming and current clinicians not only the science of oncology but also the subtle parts of language that shape patient experiences.
Key steps include:
- Communication Workshops: Practical sessions for clinicians to practice discussing diagnoses in a way that is transparent, compassionate, and balanced.
- Patient Forums: Open forums where patients can share their experiences and learn how different communication styles impact treatment choices.
- Updated Treatment Guidelines: Clinical guidelines that advocate for a balanced approach, encouraging the use of neutral language while still acknowledging the seriousness of the disease.
These elements can collectively help create an environment where the decision-making process is less about reacting to a fearsome label and more about understanding the small distinctions between various treatment strategies.
Reassessing Public Health Campaigns and Media Portrayal
Media and public health campaigns play a critical role in shaping perceptions about cancer. For decades, messages of urgency and combativeness have dominated the narrative, reinforcing the notion that every cancer diagnosis is an all-out war.
To create a calmer and more balanced approach, future campaigns could:
- Shift the focus from battle metaphors to messages that emphasize informed decision-making and personal empowerment.
- Highlight stories of patients who opted for conservative management and still maintained a high quality of life, thus offering alternative models of coping.
- Educate the public on the fine points between curing a disease and managing it as a chronic condition, stressing that more treatment is not always better treatment.
These revised messages could help reduce the overwhelming pressure that many cancer patients feel, allowing for a dialogue that respects both the seriousness of the disease and the need for thoughtful, individualized care.
Conclusion: Toward a Future of Informed, Balanced Cancer Care
Rethinking the Fighter Identity in Cancer Treatment
The discussion around cancer overtreatment exposes a crucial tension at the heart of modern medicine: the interplay between language and treatment decisions. The label “cancer” wields a powerful force that, while it has mobilized significant public support and increased research funding over the decades, also promotes an almost automatic recourse to aggressive interventions. Many patients find themselves caught between the tricky parts of a condition that demands immediate action and a desire for treatments that respect their overall quality of life.
To truly transform this landscape, both clinicians and patients need to work together to challenge the entrenched fighter identity. This means reassessing what it means to “fight” cancer. It means understanding that choosing a less aggressive treatment does not equate to surrender but can often represent a balanced, informed approach that prioritizes long-term well-being over short-term aggression.
Healthcare providers must take into account the small distinctions between aggressive intervention and measured management, while also ensuring that patients are well-equipped to make decisions that align with their values. In this way, medical communication can evolve into a tool for empowerment rather than a trigger for unnecessary action.
Embracing a New Communication Paradigm for Cancer Treatment
Ultimately, transforming how we talk about cancer—emphasizing a more nuanced, patient-centered approach rather than a simplistic battle narrative—can have far-reaching benefits. By addressing the root of overtreatment through reframed communication, the medical community can redefine what it means to face a cancer diagnosis. This shift not only respects patient autonomy but also eases the societal pressures that sometimes lead to interventions that are more harmful than helpful.
In the end, it is not enough to change the words we speak—we must change their force. By stepping away from aggressive, militarized language and embracing a model that values clarity, balanced decision-making, and patient empowerment, we open the door to a future of cancer care that is truly centered on the needs and preferences of each individual.
Toward a Collaborative Future in Cancer Care
The journey to reform cancer communication is akin to steering through a maze of twists and turns—filled with confusing bits and tangled issues. Yet, it is an essential task. As society gradually shifts away from clinging to outdated battle metaphors, each stakeholder in the field of oncology has the chance to contribute to a more thoughtful, compassionate approach to care.
This collaborative shift includes:
- Clinicians who explain treatment options with care and clarity.
- Researchers who study the fine shades in communication and their impacts on treatment choices.
- Public health officials who craft messages that empower rather than intimidate.
- Patients who share their experiences and advocate for a balanced narrative in cancer care.
When everyone—from the doctor’s office to the media boardroom—commits to changing the way we talk about and treat cancer, we set the stage for a healthcare environment where patient welfare and autonomy become the primary drivers of clinical decisions.
Final Thoughts: Moving Beyond the C-Word
In summary, the force of the word “cancer” has shaped not only patient identities but also treatment pathways, sometimes to the detriment of overall quality of life. The fighter effect has created an environment where opting for aggressive intervention becomes the default, even when evidence supports a more conservative approach. By choosing to reframe rather than simply rename, we address the core of these twisted issues—the social and linguistic cues that compel us to react in a particular way.
Reframing calls for a comprehensive rethinking of conventions in medical communication. It is about revealing and then reworking the subtle parts of language that subtly, yet powerfully, guide our expectations and decisions. This approach respects patient autonomy, reduces unnecessary interventions, and ultimately leads to cancer care that is as innovative in communication as it is in treatment.
The steps ahead are not simple. It will require persistent effort and a willingness to challenge deeply entrenched norms. But the payoff—a health care system that champions informed, balanced, and personalized care—will be well worth the effort.
In our collective fight against cancer, let us choose words that heal rather than harm, messages that empower rather than intimidate, and narratives that respect the complex, personal journey of every patient. By reworking the language of cancer, we pave the way for a future where every individual can truly decide how best to live with their diagnosis, free from the overwhelming pressure to simply “fight.”
It is time to move beyond the C-word, not by erasing it, but by transforming its meaning altogether—turning a symbol of inevitable battle into one of comprehensive, compassionate care.
Originally Post From https://aeon.co/essays/the-word-cancer-leads-to-overtreatment-and-fear-should-we-drop-it
Read more about this topic at
Reframing Cancer as Part of the Story
Reframing cancer: challenging the discourse on …