The Intersection of Online Privacy and Healthcare: Your Rights, Your Choices
In today’s digital age, the line between healthcare and online privacy has become increasingly blurred. Many of us use web-based tools to access health information, schedule appointments, and even submit our sensitive medical details. Yet, as we navigate these virtual corridors, we encounter a series of tricky parts about data collection that can leave us feeling overwhelmed and unsure of where we stand. At the heart of this discussion is our personal privacy, a super important right that deserves a closer look.
When you click “Accept” on a website’s cookie notification, you might not realize that you are agreeing to let not only the website store essential cookies on your device—but also optional ones used by partners for advertising, content personalization, and usage analysis. This decision can significantly impact your personal data, from your browsing habits to unique identifiers generated by your device. This opinion editorial aims to take a closer look at how these online data practices intertwine with modern healthcare, using a case that highlights the unexpected dangers of self-medication and the tangled issues caused by underinsured care.
Understanding the Tricky Parts of Online Data Collection
It is no secret that many websites, including those hosting reliable healthcare journals, use cookies to ensure smooth functionality. Yet, the situation becomes trickier when these websites allow partners—93 in the case of one prominent platform—to use technology that tracks more than just your general web habits. While essential cookies help in making the site function properly, optional cookies stored for personalized advertising and audience research can collect a remarkable amount of personal data.
This may seem like a minor issue compared to complex medical concerns, but when combined with healthcare data, it opens up a whole new set of challenging, nerve-racking questions about personal privacy and safety. Consider this: every time you access clinical research or a case study online, you leave behind digital footprints. These footprints may later be used to profile your interests, analyze your behavior, and even target you with highly specific advertisements. The reasons behind such practices are full of problems—riddled with tension—and it remains a pressing concern for every internet user.
How Online Advertising Platforms Shape Our Digital Identity
Digital advertising and content personalization are key components of today’s online experience. On one hand, personalized content can be very helpful, allowing you to see information relevant to your needs. On the other hand, the equipment used to track and analyze your activity might be seen as intrusive. In many cases, these tracking technologies are intertwined with the very websites that host healthcare articles, transforming your experience into one that is simultaneously beneficial and invasive.
A few noteworthy subtopics in this area include:
- Storing device information such as screen size, language setting, and supported technologies
- Deploying login-based or randomly assigned identifiers to track visitor behavior
- Utilizing detailed reports to understand usage patterns and improve service delivery
Although these practices provide super important data that can improve web functionality and content relevance, the subtle parts regarding data security and protection standards remain a concern—especially when third parties outside the European Economic Area are involved. The differences in data protection standards globally add another layer of complication to an already loaded issue.
The Reality of Modern Healthcare: When Data and Medical Decisions Collide
The convergence of data collection practices and healthcare is becoming more and more prevalent. Healthcare providers are increasingly relying on digital platforms for everything from patient records and research publications to telemedicine and remote consultations. While these advancements in technology can significantly improve the quality and accessibility of care, they also come with their own set of twists and turns.
For example, while offering personalized treatment plans is a super important factor to improve patient care, the process of tailoring these plans collected from online data needs to be carefully managed. Health information that is gathered online can sometimes be at risk of exposure if robust cybersecurity measures are not in place. In many cases, patients remain unaware of the extent to which their data is being used, transforming what might seem like a straightforward visit to a healthcare website into an off-putting prospect when you consider the potential misuse of your information.
The Influence of Cost and Access on Patient Behavior
A more tangible real-world example of how high costs and inadequate access to prescribed medications can drive individuals to seek dangerous alternatives comes from a compelling medical case that many healthcare professionals continue to discuss. In this case, a 50-year-old man with a history of hypertension and asthma encountered a series of unexpected complications that serve as a cautionary tale for us all.
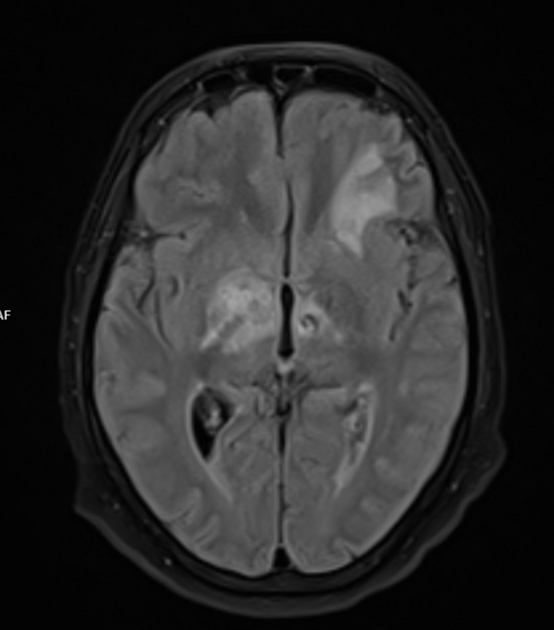
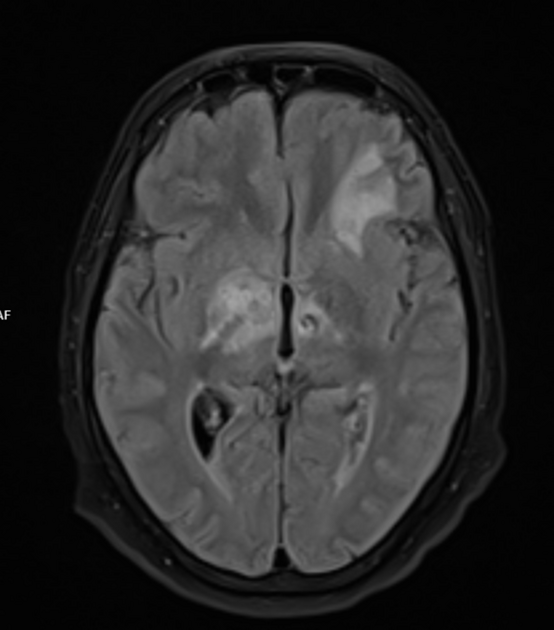
Case Study: Steroids, Seizures, and a Surprising Pathogen
The patient in question presented to the emergency department following a series of new-onset seizures and alterations in mental status. Although his symptoms first appeared to be linked to diabetic ketoacidosis and various metabolic derangements, his condition rapidly deteriorated to the point where he entered status epilepticus—an incredibly overwhelming situation requiring immediate, advanced intervention.
Not only did the patient exhibit signs of hypertriglyceridemia, elevated lactate levels, and metabolic acidosis, but his case also raised critical questions about the source of his underlying condition. After extensive workup including a lumbar puncture and the use of a meningoencephalitis PCR panel, the patient was diagnosed with Listeria monocytogenes infection—a pathogen that typically represents a twisted detail hidden within the broader narrative of central nervous system infections.
Tangled Issues in Self-Medication and Underinsured Healthcare
One key revelation during the patient’s history gathering efforts was the discovery that he had been self-medicating with prednisolone tablets purchased online from overseas. Faced with the high costs of his prescribed asthma inhalers, he had taken matters into his own hands, relying on unregulated sources for his medication. This self-medication not only contributed to his immunosuppressed state but also set the stage for the unexpected encounter with Listeria.
The case brings several points to the forefront:
- Cost Barriers: The staggering cost of correctly prescribed medications, such as asthma controller inhalers, drives patients to take shortcuts that can lead to severe, often nerve-racking complications.
- Self-Medication Risks: Relying on unverified online pharmaceutical sources can introduce medications that have not been appropriately screened, leading to adverse effects like infection and metabolic disruptions.
- Collateral Information: A comprehensive patient history—including inquiries into all medications used—is essential. The patient’s failure to disclose his online-purchased prednisolone use initially obscured the cause of his immunosuppression.
Below is a summary table of the patient’s key laboratory values on admission, which illustrate the confusing bits and fine points clinicians needed to sort out:
| Parameter | Patient Value | Reference Range |
|---|---|---|
| White Blood Cell Count | 12.0 x 10³/μL | 4.1–9.9 x 10³/μL |
| Sodium (Na) | 125 mmol/L | 135–146 mmol/L |
| Creatinine (Cr) | 2.30 mg/dL | 0.6–1.3 mg/dL |
| CO₂ | 9 mmol/L | 20–30 mmol/L |
| Triglycerides (TG) | 1570 mg/dL | <150 mg/dL |
| Glucose (Glc) | 330 mg/dL | 65–99 mg/dL |
| Ketoacidosis Marker | Positive Ketones | Negative |
This table underscores the profound metabolic disturbances in the patient’s system—a direct consequence of untreated diabetes compounded by the off-prescription use of oral steroids. Such a clinical picture requires providers to make their way through a myriad of overlapping issues, from managing metabolic derangements to treating an unusual central nervous system infection.
The Shocking Journey from Asthma Management to Listeria Infection
The patient’s journey highlights a series of problematic twists and turns that reflect broader issues within the healthcare system. His failure to afford proper asthma maintenance therapy led him to choose a cheaper but potentially hazardous alternative—oral prednisolone. This decision, unbeknownst to his healthcare providers, left him immunosuppressed and more vulnerable to infections that a healthy immune system could normally stave off.
Moreover, the gradual buildup of metabolic issues over time—evidenced by obesity, diabetes, and hypertriglyceridemia—serves as a stark reminder that self-medication is not without consequences. The fine details of his case reveal that while his outward symptoms were initially attributed to common complications such as diabetic ketoacidosis, the underlying cause was far more nuanced: unregulated medication usage. This case reminds both practitioners and patients to take a closer look at every piece of the health puzzle, because sometimes the most unexpected twist can be the most critical.
The Hidden Complexities of Self-Medication and Economic Barriers in Healthcare
Self-medication practices and the high cost of healthcare create a landscape loaded with problems. Many patients find themselves caught between a rock and a hard place: they either adhere to expensive, state-of-the-art treatment regimens or risk defensive, off-prescription alternatives that are full of problems. The case discussed above is one extreme example of what can happen when economic pressures lead to dangerous health choices.
There are several confusing bits that need to be addressed when assessing the risks associated with self-medication:
- Unregulated Pharmaceuticals: Medications obtained online, especially from overseas sources, often do not adhere to the same quality and safety standards found in regulated markets. Patients may unknowingly expose themselves to harmful contaminants or inappropriate dosing.
- Immunosuppression Risks: Oral steroids, even when taken intermittently, can suppress the immune system in a dose-dependent manner. This immunosuppression increases the risk of unusual infections, which might otherwise be rare in patients not using these medications.
- Systemic Side Effects: Chronic systemic steroid use is associated with a host of adverse effects—including, but not limited to, exacerbated blood sugar levels, hypertension, and changes in lipid profiles. These factors were clearly visible in our case study.
A table summarizing common adverse effects of long-term oral steroid use may help visualize these subtleties:
| Adverse Effect | Potential Impact |
|---|---|
| Increased Infection Risk | Greater vulnerability to bacterial and viral infections |
| Metabolic Derangements | Elevated blood sugar, hypertriglyceridemia, and weight gain |
| Hypertension | Increased blood pressure leading to cardiovascular strain |
| Osteoporosis | Bone density loss over time, increasing fracture risk |
These small distinctions matter a great deal in determining the overall health outcomes of patients. The case in question is a striking example of how the fine points of a patient’s history—in this instance, the undisclosed use of oral steroids—can dramatically alter both diagnosis and treatment outcomes.
Lessons Learned: The Importance of Collateral History and Informed Decision-Making
One takeaway from the case study is the critical need for thorough and honest communication between patients and healthcare providers. Obtaining collateral history—information from family, friends, or secondary records—can often uncover hidden details that may change the course of treatment entirely. In this scenario, once the healthcare team learned that the patient was taking prednisolone tablets purchased online, they were better equipped to understand his immunosuppressed state and modify treatment accordingly.
Here are several key lessons that can be drawn from this unfortunate episode:
- Comprehensive History-Taking: Clinicians must always take a complete and nuanced patient history. Even seemingly minor or unrelated details, like the use of unregulated medications, can have major implications for health outcomes.
- Communication is Key: Open, non-judgmental dialogue between patients and providers helps to ensure that all relevant information is disclosed, thereby preventing misdiagnoses and mismanagement.
- Economic Pressures Matter: The high cost of standard therapies can drive patients to risky alternatives. Addressing this issue requires broader policy changes and improved access to affordable healthcare options.
In many ways, this case teaches us that health is a mosaic made up of many small parts—a combination of physiological conditions, medication histories, and even socioeconomic factors. Each of these components, no matter how trivial they may appear at first glance, plays a role in shaping a patient’s overall well-being. Understanding these subtle parts is super important for ensuring that each patient receives care tailored to their unique circumstances.
Steps to Find Your Way Through the Maze of Modern Healthcare
For both patients and providers, taking the wheel in today’s complex healthcare landscape takes more than just medical knowledge—it requires a proactive approach to navigating tricky issues and potentially overwhelming challenges. Below are some steps that can help individuals figure a path through these issues:
- Be Proactive About Your Health Data: Regularly update your privacy settings on healthcare websites and be informed about how your data is used. It’s critical to read privacy policies carefully and, if necessary, adjust your cookie preferences.
- Maintain a Detailed Medication Record: Keep an updated list of all prescribed and over-the-counter medications you take. Ensure that this record includes any supplements or unregulated drugs you might be using.
- Seek Professional Guidance Before Self-Medicating: If you’re considering any alternative source for medications due to cost constraints, talk to your healthcare provider. They might have suggestions for financial assistance, generic alternatives, or other safe options.
- Engage in Open Dialogue: During doctor visits, share your challenges regarding medication costs and any non-standard practices you might be experiencing. This helps your provider tailor a treatment plan that’s both effective and sustainable.
- Stay Informed About Digital Privacy: Learn about the types of cookies and tracking technologies used on healthcare websites. Understanding these can help you feel more secure while browsing sensitive information online.
Implementing these steps can help both patients and providers work through the murky bits and subtle details of modern healthcare delivery. Transparency and collaboration are key to overcoming the nerve-racking challenges that arise in today’s digital and medical landscapes.
The Role of Healthcare Policy in Bridging Economic Gaps
One cannot ignore the broader economic forces at play in situations like the case described above. The soaring cost of medications—which in the United States can be overwhelming—often leaves patients with no choice but to resort to risky, self-managed alternatives. In fact, studies suggest that medication adherence in chronic conditions like asthma is disturbingly low, with cost-related nonadherence affecting a considerable segment of patients.
These economic pressures are full of problems and necessitate policy changes that aim to bridge the gap between available high-quality care and the ability of patients to access it affordably. By implementing strategies that enhance insurance coverage, reduce drug prices, and increase transparency in pharmaceutical pricing, lawmakers can make a positive difference. For instance:
- Increase Subsidies for Essential Medications: Expanding access to affordable therapies can drastically reduce the temptation for patients to pursue unregulated alternatives.
- Support Generic Drug Markets: Encouraging the availability of quality generic medications can ease the overall cost burden and reduce the risk associated with self-medication.
- Enhance Patient Education Programs: Clear and accessible information about medication risks, proper usage, and digital privacy can empower patients to make better decisions.
These measures, if implemented effectively, can help reduce the heated, overwhelming price tags associated with modern care while also decreasing the incidence of adverse medical outcomes due to self-medication.
Integrating Digital Literacy and Medical Expertise
As healthcare continues its digital evolution, there is a unique opportunity to integrate digital literacy with medical expertise. Both healthcare professionals and patients need to be equipped to cope with the subtle details and slight differences that digital data collection brings along. This integration is key not only to ensuring the confidentiality of patient information but also to improving outcomes by guiding users through the maze of health information without undue disturbance.
Medical professionals must adopt a proactive stance in educating patients about how their data is collected, used, and stored online. Providers can use easily digestible formats—such as infographics, bullet lists, and straightforward policy explanations—to demystify these processes. By doing so, they will help patients get into the nitty-gritty of digital privacy without feeling too overwhelmed by the technical jargon.
Likewise, digital platforms can invest in clearer notifications and user-friendly tools that allow individuals to customize their privacy preferences. For example, many healthcare websites now include a “Manage Preferences” option and a dedicated “Your privacy choices” section in the footer of every page. These tools are designed to give users more control over what data is stored or read on their device.
Bringing It All Together: A Call for Informed, Collaborative Decision-Making
The themes we’ve discussed—from online privacy issues and clever data tracking methods to the nerve-racking risks of self-medication due to mounting healthcare costs—underscore the complex, full-of-problems landscape that both patients and providers must navigate. While digital advances in healthcare offer incredible opportunities for better patient care, they also bring tangled issues that, if left unchecked, can have serious consequences.
In the case of the 50-year-old patient who suffered from Listeria meningoencephalitis after self-medicating with overseas prednisolone, the chain of events was set off by a series of seemingly small decisions, each influenced by a broader system of economic pressures and inadequate transparency. His story is not just a medical case report—it is a microcosm of how modern challenges in both digital data management and healthcare access can combine in unexpected, sometimes dangerous ways.
As both patients and healthcare advocates, it is essential to push for measures that support informed decision-making at every level. Providers should continue to take a closer look at each patient’s medication history, especially in cases where there might be underlying factors not immediately evident from a standard interview. Patients, for their part, must feel empowered to ask questions about both their treatment options and how their personal data is being managed online.
To conclude, let us remember these key points as we move forward in this era of changing healthcare and digital transformation:
- Transparency in Data Collection: Patients should be aware of what data is being collected and how it is being used. Empowered with this knowledge, they can make more informed choices about their online interactions.
- Informed Medication Choices: Cost should never force patients into taking dangerous shortcuts with their health. Comprehensive history-taking and dialogue with providers can help mitigate risks associated with self-medication.
- Collaborative Policy Changes: Addressing the problem of unaffordable healthcare requires collective effort—from healthcare providers, policy makers, and patient advocacy groups alike—to create a more equitable system.
- Digital and Medical Literacy: As both the digital and medical fields continue to evolve, continuous education is a must. Both patients and professionals must work together to figure a path through these intertwined issues.
The story and lessons recounted above should serve as a wake-up call. While the conveniences of digital tools offer many benefits, they also demand responsibility from all parties involved. Let us take a proactive approach to ensure that our personal data remains secure and that our healthcare choices are always informed by the best possible information. In a world where every click—and every medication decision—can have lasting impacts, we must remain vigilant, transparent, and collaborative in our approach to both online privacy and medical care.
Looking Ahead: A Future That Balances Privacy, Access, and Health
As we look toward the future, the challenges of online privacy and healthcare cannot be understated. It is a future full of both promise and potential pitfalls. The increasing interconnectedness of our digital lives with our personal health data means that every policy decision, every regulatory measure, and every healthcare provider’s choice impacts millions.
For instance, the evolving landscape of telemedicine and digital health records can lead to superior, more efficient care, but only if data protection measures keep pace with technological advancements. Similarly, affordable access to life-saving medications and therapies remains a super important concern for many patients who find themselves caught between the promise of modern medicine and the reality of soaring costs.
To ensure that the benefits of digital integration are fully realized without any compromising side effects, we must work through these tangled issues collaboratively. Future advancements should include:
- Robust Data Security Protocols: Investing in state-of-the-art cybersecurity that protects sensitive health information should be a top priority for healthcare organizations and digital platforms alike.
- Clearer Consent Processes: Websites and healthcare portals should move beyond generic cookie notices to provide patients with clear, understandable options regarding what data is collected and used.
- Effective Patient Support Programs: Government and healthcare institutions should collaborate to create programs that subsidize essential medications and reduce out-of-pocket expenses, ensuring that patients do not need to resort to unregulated alternatives.
- Enhanced Digital Literacy Initiatives: Both patients and providers must be encouraged to learn more about the digital spaces they frequent. Knowledge is the first step toward making informed decisions that safeguard health and privacy.
These future steps, combined with the lessons learned from real-world examples, have the potential to transform how we engage with both healthcare and digital information. The ultimate goal is to build a system that not only provides cutting-edge medical care but also respects and upholds the privacy rights of each individual—ensuring that every patient feels safe, informed, and empowered in their interactions with modern medicine.
Final Thoughts: Embracing a Collaborative Future
The intertwining of online privacy and healthcare brings to light many of the subtle but critical twists and turns that define our modern era. The story of a patient who found himself caught between medical necessity and economic hardship serves as a potent reminder: The simplest choices—like clicking “Accept” on a cookie notice or opting for an affordable medication alternative—can have profound, far-reaching consequences.
In our journey forward, it is essential for healthcare providers, policy makers, and patients alike to stay abreast of these challenging issues. Together, we can work through the confusing bits of digital data collection, make informed medication decisions, and advocate for policies that reduce the financial burdens on those in need. By doing so, we create a healthcare environment that is not only effective but also fair and ethically responsible.
Let this editorial serve as a call for awareness and collaboration. Whether it’s taking a closer look at your privacy settings online or ensuring that all aspects of your medication history are discussed openly with your healthcare provider, every step contributes to a safer, healthier future for us all.
Ultimately, managing your way through both digital and medical landscapes is a shared responsibility. By staying informed, embracing transparency, and pushing for accessible and affordable care, we can all work together to shape a future where privacy, health, and well-being go hand in hand.
Originally Post From https://www.cureus.com/articles/382815-steroids-seizures-and-a-surprising-pathogen-a-case-of-listeria-meningoencephalitis
Read more about this topic at
Anabolic steroid misuse
Anabolic Steroids and Other Appearance and Performance …