When a Sinus Headache Means More Than Just an Infection
The story of Brian McNamara, a teacher and football coach from New Jersey, reminds us that sometimes the body sends complicated bits of information that can be misinterpreted. What began as what appeared to be a simple sinus headache soon spiraled into an overwhelming medical odyssey. Brian’s persistent, nagging symptoms were initially dismissed as nothing more than a sinus infection. However, as his discomfort grew day by day with additional signs such as ringing in the ears, a strange underwater fullness, bad breath, neck pain, and jaw tightness, it became clear that these were not the typical twists and turns of a harmless infection.
Despite the initial diagnosis at an urgent care center, Brian’s plight continued to worsen. His story is one that urges us to take a closer look at the hidden complexities in the human body, especially when minor signs hide something more menacing. His journey is a sobering reminder that even common illnesses can sometimes mask far more serious conditions and that both patients and healthcare providers need to steer through the tricky parts of diagnosis with extra caution.
Detecting the Subtle Signs: When Chronic Symptoms Demand More Attention
One of the many challenges in modern healthcare is distinguishing between the common and the complicated pieces of a patient’s presentation. Brian’s symptoms—initially mild and persistent—escalated to new heights that many would consider nerve-racking. His experience sheds light on how easily initial symptoms can be overlooked, especially when they fall within the realm of what many assume to be routine sinus infections.
It is common practice for healthcare professionals to treat suspected conditions with standard protocols that sometimes miss the outlier cases. In Brian’s case, it wasn’t until he experienced facial numbness and double vision that the pattern of his symptoms could no longer be dismissed as mere sinusitis. This scenario underlines the need to figure a path for improved diagnostic protocols that consider both the visible signs and the subtle details—the fine points—that might indicate a deeper condition.
The situation forces us to consider the importance of listening to one’s body and the necessity for open communication between patients and doctors. There are often tangled issues in clinical diagnoses, particularly when the symptoms evolve gradually. For patients, every minor twist and turn in their symptom profile should be seen as a super important indicator that something more serious might be at play—especially if previous treatment plans have not produced the expected relief.
Recognizing Rare Cancers: The Critical Role of Medical Imaging and Specialist Evaluation
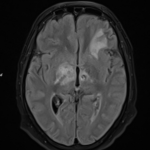
Brian’s journey took a dramatic turn when he returned to the emergency room after Thanksgiving. It was then that medical imaging—through MRI and CT scans—revealed a mass in his sinuses. Initially thought to be squamous cell carcinoma, the mass was later reclassified as small cell neuroendocrine carcinoma, a rare and highly aggressive form of cancer. This revelation highlights the tricky parts of differentiating between various types of cancers, particularly when they occur in less typical locations.
Modern medical imaging has dramatically improved our ability to get into the nitty-gritty of a patient’s physical condition. However, even these advanced techniques can sometimes present confusing bits. In Brian’s case, the initial assumption by some medical personnel and the subsequent detailed analysis underscored how a revisit to one’s diagnosis can be both intimidating and essential.
Here is a simplified table outlining the progression of symptoms and tests that Brian experienced:
| Time Period | Symptoms/Findings | Action Taken |
|---|---|---|
| Early 2024 | Persistent sinus headache, ear ringing | Visited urgent care for sinus infection treatment |
| Over subsequent months | Worsening pain, fullness in ears, neck pain, jaw tightness | Continued treatment with minimal improvement |
| Two weeks before Thanksgiving | Facial numbness, double vision | Return to ER; MRI and CT scans performed |
| Post-Thanksgiving | Mass detected in sinuses | Biopsy conducted; diagnosis refined |
This table illustrates how a series of subtle developments can signal a severe underlying problem. It is critical that both patients and healthcare providers are aware that the body’s messaging might come in layers—small distinctions which, when pieced together, can change the course of diagnosis entirely.
Working Through the Maze: The Value of Immediate Specialist Intervention
Once it became clear that Brian’s mass was not a mere sinus infection, the race against time began. The situation required immediate and expert intervention. With specialists at the forefront, Brian was transferred to a top-tier facility, Memorial Sloan Kettering Cancer Center. There, he met with both a medical oncologist and a radiation oncologist who stressed that every moment counted.
In critical scenarios like this, it is super important to get around the delays that can sometimes plague standard medical procedures. Instead of a routine follow-up, Brian’s case was handled with urgency. He was placed into a treatment plan that involved intensive chemotherapy—three consecutive days of treatment every three weeks for five rounds—and proton radiation administered twice daily for 15 days.
This rapid response, although overwhelming and off-putting in its intensity, exemplifies the key shift in modern cancer care. It demonstrates that when rare cancers strike, it is not just the treatments themselves that matter, but also the swiftness and determination of the medical team. When the unexpected appears, it is imperative for the healthcare system to have a clear and rapid response pathway in place.
Patient Advocacy and Community Support: Taking the Wheel in Healthcare Decisions
While Brian’s fight against an aggressive cancer was being waged inside hospital walls, another equally important aspect of his journey was unfolding outside: the power of patient advocacy and community support. His wife, Jodi, emerged as a central figure in ensuring that his voice was heard and his needs were met. Describing the ordeal to Newsweek, Jodi emphasized just how nerve-racking it was to see Brian go from one diagnostic phase to another, with treatment decisions changing rapidly.
In an age where many experience tangled issues in communication with insurance companies and healthcare providers, patient advocacy is more important than ever. Jodi took to platforms like TikTok to document Brian’s journey. What started as an effort to find answers quickly turned into a platform that rallied community support. Hundreds of messages, car parades, and public displays of solidarity created a network of care that stretched far beyond the hospital corridors.
Below is a list of key actions that underscore the power of patient advocacy in Brian’s case:
- Documenting daily struggles and improvements on social media.
- Engaging with experts and seeking second opinions from leading cancer centers.
- Sharing the financial and emotional challenges encountered with insurance providers.
- Mobilizing local communities to show support through events and public displays.
- Utilizing digital platforms to gather information and create a supportive network.
This list not only shows the practical steps taken by Jodi but also highlights the super important influence that a supportive community can have during nerve-racking times. It also serves as a reminder that in the modern healthcare environment, families sometimes need to take an active role in managing the course of treatment.
Exploring the Fine Points of Treatment Options for Rare Cancers
When facing an aggressive disease like small cell neuroendocrine carcinoma, the treatment options available are both critical and often riddled with tension. The approach taken in Brian’s case reflects a blend of traditional chemotherapy techniques and cutting-edge proton radiation therapy. While both are essential parts of the treatment plan, they involve a series of complicated pieces that require close monitoring and adjustments as needed.
Proton therapy stands out because it uses a focused beam of protons to target cancer cells with precision. It is often seen as a safer alternative to traditional radiation, given its ability to minimize damage to surrounding healthy tissue. However, its availability is limited to specialized centers, and the procedure itself demands a highly coordinated team of medical experts.
Here is a bullet-point summary of the treatment aspects that Brian underwent:
- Chemotherapy: Administered in cycles to target rapidly dividing cancer cells. Brian’s regimen involved three days of treatment every three weeks for a total of five cycles.
- Proton Radiation Therapy: Delivered twice daily for a set period of 15 days to ensure the highest precision in destroying tumor tissue while protecting nearby critical structures.
- Multi-Disciplinary Team Approach: Combining the expertise of oncologists, radiologists, and specialized nurses to adapt treatment strategies in real time.
The decision to initiate such a rigorous treatment plan was accompanied by a mix of hope and the nerve-racking uncertainty that always accompanies aggressive cancer care. For patients like Brian, it is a journey that requires them to get into the nitty-gritty of making constant decisions—sometimes without a clear roadmap on what the future may hold.
Finding Your Way Through a Complex Medical Landscape: Expert Consultation and Second Opinions
One clear lesson from Brian’s medical roadmap is the super important need for diverse expert input. After the initial cancer diagnosis, Brian and his family did not limit themselves to just one perspective. Instead, they traveled to various medical communities in Texas, Boston, and Maryland in an effort to gather as many insights as possible.
This proactive approach is essential in conditions that present with numerous confusing bits—conditions where a single opinion might not provide the full picture. Seeking multiple expert opinions not only provides a safety net against potential error but also allows for a broader discussion on advanced treatments such as immunotherapy. Though there is hope that Brian might be eligible for an additional year of this therapy, there remains the pressing fear that if the cancer returns within that period, there will be few options left.
The process of sorting out different opinions is like piecing together a puzzle: each perspective contributes a piece that, when combined, presents a fuller view of the treatment landscape. Here are some practical steps that individuals can take when faced with such a challenging situation:
- Request referrals to specialized centers with a strong track record in rare cancer treatment.
- Compile a comprehensive list of symptoms and previous treatment responses to share with each specialist.
- Research treatment options and clinical trials that might provide additional avenues for care.
- Engage with patient support groups who have experienced similar health journeys.
- Maintain an open line of communication with all healthcare providers involved in the care process.
These steps serve as a guide for those who must find a way out of the maze of medical decisions, ensuring that every fine shade in the treatment process is considered before arriving at a final plan. For many, this kind of proactive engagement is both liberating and essential in overcoming the intimidating barriers of modern healthcare.
Social Media and Digital Engagement: Building a Community of Care
The digital age offers both challenges and opportunities in managing personal health. For Brian’s family, social media became a vital lifeline—a tool to connect with others who had weathered similar storms in their health journeys. Jodi’s decision to document Brian’s condition on TikTok was driven by a mix of desperation and determination. Her posts quickly transformed into a dynamic community where people exchanged tips, shared personal stories, and offered much-needed emotional support.
This intersection of technology and healthcare exemplifies how digital platforms can help people get around the isolated nature of medical crises. Jodi’s online presence not only raised awareness about a rare form of cancer but also provided a space for practical advice—ranging from understanding treatment options to dealing with insurance hurdles—to be shared widely.
Below is a brief outline of the potential benefits that come from embracing digital engagement during healthcare battles:
- Emotional Support: Social media groups often offer empathy and understanding from individuals who truly get the situation.
- Shared Experiences: Hearing firsthand accounts from others who have faced similar diagnoses can help in anticipating challenges and planning next steps.
- Access to Information: Digital platforms provide real-time updates on the latest treatments, clinical trials, and healthcare research.
- Advocacy and Awareness: A strong online community can amplify one person’s story into a movement that brings about systemic changes in healthcare policies.
Yet, the blend of digital technology and personal health does come with nerve-racking issues related to data privacy. Amidst all the supportive interactions, there is an underlying reality concerning how personal information and medical details are collected and shared online. The need to balance outreach with caution remains full of problems, as individuals must continuously manage their privacy settings and decide whom to trust with sensitive health information.
Privacy in the Digital Age: Balancing Awareness with Data Protection
In a world where digital footprints are ever-present, the discussion around privacy choices becomes super important. Many websites, including those in healthcare, use cookies and other tracking technologies to offer personalized content and advertising. While these methods are designed to enhance user experience, they also raise concerns about who gets to see one’s personal data.
Brian’s family, while busy tackling the health crisis, also had to deal with the off-putting intricacies of privacy policies. When visiting websites for health information or community support, users often encounter lengthy privacy settings that allow them to accept, reject, or customize data usage. These settings can feel intimidating, especially when the policies are filled with confusing bits of legal jargon and technical details.
The duality of being both informed and protected in the digital space is a challenge that modern news outlets and healthcare websites must address. Users are often required to click on “Privacy Settings” to fine-tune what data is shared with partners, and even when this is done, some partners rely on what is known as legitimate interest to process personal data. Although there is an option to “object to legitimate interest,” the whole process underscores how intricate—and on edge—the management of personal data can be.
This matter isn’t just an abstract debate about data; it has very real implications for patients who share their health journeys online. When stories like Brian’s become public and inspire widespread discussion, the accompanying data collection practices become full of problems that need to be managed with caution. Healthcare websites, therefore, have the responsibility to maintain robust privacy policies while also allowing their users to access the compassionate support and accurate information they need.
Lessons Learned: The Off-Shore Realities and Future of Healthcare
Brian McNamara’s case is a potent reminder of how easily a health journey can take unexpected and dramatic turns. His experience is layered with lessons for both the public and medical professionals. Even though his initial symptoms seemed like routine complications, the hidden severity of his condition became clear only after persistent issues and multiple tests.
For healthcare providers, the story emphasizes the necessity of getting into every subtle part of symptom evaluation. There is a need to acknowledge that every little twist—a persistent headache, unexplained facial numbness, or a sudden change in vision—can be the early signal of a condition that requires immediate and specialized attention. In such situations, it is critical to act swiftly and to figure a path that minimizes delays, even if that path is laden with challenges.
For patients, there is an equally important lesson about the power of patient advocacy. Keeping track of one’s symptoms and insisting on further tests when something doesn’t add up can be the difference between early detection and a missed opportunity for timely treatment. While it is nerve-racking to challenge an initial diagnosis, doing so might just be the push needed to secure life-saving care.
Moreover, the role of expert consultation cannot be overstated. Brian’s journey shows that seeking second and even third opinions is not just a luxury but a necessity—especially when dealing with rare and aggressive diseases. By actively engaging with multiple experts and researching further, patients can manage their conditions more effectively and possibly avoid the pitfalls associated with a one-size-fits-all treatment approach.
Healthcare is a complex interplay between technology, human judgment, and the unpredictable nature of biology. In these challenging situations, professionals and patients alike must work together to map out the little details that could ultimately lead to better outcomes. Whether it is through innovative treatments like proton therapy or comprehensive community-based information sharing, every effort counts when time is of the essence.
Finding Strength in the Community: The Unseen Benefits of Collective Support
Beyond the hospital corridors and the high-stakes decisions, the community response to Brian’s illness has been both heartening and instructive. The outpouring of love—demonstrated through initiatives like local car parades and heartfelt social media messages—serves as a reminder that even in the face of intimidating challenges, a united community can offer strength and resilience.
The practical benefits of this collective support go beyond simple emotional comfort. Community involvement can also provide tangible assistance, such as logistical help with transportation, emotional counseling, or even financial aid to help with mounting medical bills. In today’s fast-paced digital world, connecting with like-minded individuals who have faced similar experiences can help patients and families get around the nerve-racking issues of isolation during long treatment cycles.
Here are some of the key practical benefits that come from a strong community support network:
- Emotional Resilience: Knowing that one is not alone can help reduce feelings of anxiety and stress during extreme medical challenges.
- Practical Assistance: Community-managed events and local initiatives can provide direct support, such as rides to treatment centers or help with household chores.
- Shared Information: Platforms where patients share experiences may highlight treatment options or coping strategies that would otherwise remain hidden.
- Advocacy Efforts: A vocal community can influence policy decisions, prompting healthcare systems to improve communication and streamline treatment processes.
Observing the public response to Brian’s situation reminds us that, while the battle against a rare cancer may be full of problems and unpredictable twists, it can also bring out the best in human solidarity. In this case, the community’s rallying cry not only boosted Brian’s morale but also highlighted the potential for grassroots movements to affect meaningful change in the way healthcare challenges are approached.
The Road Ahead: Embracing Change in Healthcare Diagnosis and Treatment
Brian’s journey, marked by a series of confusing bits and nerve-racking moments, calls for a broader conversation about the state of modern healthcare. It is an invitation for medical institutions, policymakers, and patients alike to get into a closer look at the process by which diagnoses are made, and treatments are decided upon. The experience invites us all to consider what can be done to smooth out some of the twisting turns in current diagnostic practices.
There are several key areas where improvements can be made to help prevent another case like Brian’s from unfolding:
- Enhanced Diagnostic Protocols: Medical professionals should be urged to consider a wider range of potential conditions when dealing with persistent symptoms. This includes reusing imaging and lab tests if treatments do not produce the expected outcomes.
- Interdisciplinary Collaboration: Bringing together experts from different fields encourages the sharing of ideas and ensures a more comprehensive review of a patient’s symptoms.
- Patient Empowerment: Educating patients to recognize when a standard diagnosis might not fully explain their symptoms can foster a more proactive approach to seeking second opinions.
- Technological Advances: Continued investment in advanced medical imaging and diagnostic algorithms can help sift through the tangled issues of symptom presentation more effectively.
- Community Outreach and Digital Engagement: Leveraging social media and online health platforms can create networks of support and information, driving a collective effort in improving patient care.
By addressing these areas, the healthcare field can begin to untangle the tricky parts inherent in diagnosing rare or aggressive diseases. It is through thoughtful, community-based reform and individual vigilance that the prospects for early detection and effective treatment improve, giving hope to patients who face the most challenging conditions.
Reflecting on the Journey: Personal Stories as Catalysts for Systematic Change
As we reflect on Brian McNamara’s ongoing struggle, it becomes clear that his personal experience is more than just a story of misdiagnosis—it is a call to action. His journey urges healthcare professionals to not merely rely on first impressions but to figure a path through every twist and turn until they reach a sound diagnosis. It also reminds patients of the super important need to trust their instincts and advocate for themselves when the stakes are so high.
There is an underlying human truth in these narratives: that the body’s messages, no matter how small, deserve attention. In an era of advanced medical technology and fast-paced digital communication, the intricate dance between patient symptoms and professional assessments must remain a collaborative effort.
Moreover, Brian’s case teaches us that while technological advancements have dramatically improved diagnostic accuracy, they must be paired with compassionate care and active patient involvement. Even the most sophisticated medical systems are sometimes loaded with issues that leave patients feeling on edge, especially when treatments are experimental or outcomes remain uncertain.
His story is a poignant reminder that every detail matters—from the first persistent headache to the final decision on which treatment to undertake. And for every patient and family facing similar challenges, the journey through a problematic diagnosis is one that can be made less isolating and more hopeful when shared broadly and discussed openly.
Conclusion: Embracing the Future of Patient-Centered Healthcare
In the end, Brian McNamara’s experience is a microcosm of larger trends in modern medicine—a reality where symptoms can be deceptive, and the path to healing is fraught with both predictable and unexpected challenges. It is a story that underscores the necessity for both cautious medical investigation and robust community support.
Healthcare providers must find new ways to get around the confusing bits of diagnosis by incorporating thorough patient history, advanced testing, and a willingness to reexamine initial findings. At the same time, patients must feel empowered to take the wheel in their own healthcare decisions, knowing that every subtle detail, no matter how small, could be the indicator of a larger issue.
As we move forward, the hope is that such stories will drive improvements in both the technical and interpersonal aspects of medicine. By embracing a strategy that combines expert consultation, advanced technology, and empathetic community outreach, the journey from diagnosis to treatment can become more transparent and less intimidating for everyone involved.
For those of us who follow these narratives closely, there remains a super important lesson: our health is our most valuable asset. Small changes in how symptoms are interpreted and how medical information is shared can make a world of difference in patient outcomes. Whether you are a patient, a caregiver, or a healthcare professional, taking the time to appreciate every subtle detail of a medical situation is not merely an academic exercise—it could very well be a matter of life and death.
Brian’s story, with all its twists and turns, is not just about a rare cancer; it is an important reminder of the value of perseverance, the necessity of questioning standard diagnoses, and the need for a healthcare system that works in tandem with the community. It is a call to re-examine how we approach health in an age of both technological marvels and profound human challenges, urging us all to be more vigilant, more informed, and more caring as we face the future.
In this rapidly changing landscape, balancing medical advancement with personalized care is a journey that requires continuous learning and adaptation. Stories like Brian’s are catalysts for change, showing us that when patients and healthcare providers come together, they can overcome even the most daunting challenges—turning a once-overwhelming crisis into a roadmap for progress in patient-centered care.
Ultimately, the fight against aggressive diseases is a community effort. It depends on acknowledging every subtle detail, every small distinction in how symptoms manifest, and every critical piece of information that can lead to better treatment outcomes. This collective vigilance and cooperation will help ensure that the next time someone experiences what seems like a minor health issue, both the patient and their doctors are ready to get into the problem-solving process with all the resources at their disposal.
As we witness stories of resilience and determination such as Brian’s, we are reminded of a timeless truth: in the realm of healthcare, the small victories—every step taken to overcome an initial misdiagnosis or to secure a second opinion—accumulate into a larger movement towards a system that truly listens and responds with both precision and compassion.
While the digital age poses its own challenges in terms of data privacy and the complexities of information sharing, it also offers us the tools to build stronger, more connected communities. In this brave new world, the balance of cutting-edge technology and heartfelt human empathy paves the way for a better tomorrow. Let us all take a closer look at our own health journeys and, together, shape a future where every patient’s story contributes to a more responsive and compassionate healthcare system.
Originally Post From https://www.newsweek.com/man-rare-cancer-sinus-infection-2099677
Read more about this topic at
Unexpected Diagnosis at 28: Aggressive Breast Cancer
Living with an unexpected lung cancer diagnosis: Bobbi …