Understanding Colorectal Cancer Disparities in the USA
Colorectal cancer continues to be a major public health challenge in the United States, and the numbers tell a troubling story. Even as overall incidence rates decline, Black communities face higher rates of colorectal cancer incidence and mortality compared with their White counterparts. In this opinion piece, we take a closer look at the tangled issues surrounding screening, treatment, and survival outcomes while also considering the underlying social factors that create these persistent disparities. Through this discussion, we aim to shed light on both the near-term fixes and long-term strategies needed to find your way through these uneven healthcare trajectories.
The conversation is not merely about the existence of unequal outcomes; it is equally about understanding why these differences occur. When we talk about colorectal cancer care, there are a number of tricky parts that influence the overall picture. These range from structural challenges embedded in healthcare access to the less obvious, subtle details found in patient communication and trust. In highlighting these areas, we hope to offer an informed perspective on how improvements can be made for every community affected by this disease.
Social Determinants and Their Impact on CRC Outcomes
One of the most critical aspects that drive disparities in colorectal cancer outcomes is the range of social determinants of health. These include economic conditions, neighborhood environments, education, employment opportunities, and overall access to services. When these factors are skewed unfavorably, they create complicated pieces within the healthcare puzzle that make it difficult for many Black individuals to receive timely and high-quality care.
Socioeconomic Challenges and Screening Participation in Black Communities
For many in Black communities, the journey to diagnosis and treatment is loaded with obstacles. A lack of reliable transportation, unsupportive work policies, and a scarcity of nearby healthcare facilities all contribute to lower participation in screening programs. When people are busy juggling multiple responsibilities or dealing with financial strain, a routine screening can seem both overwhelming and off-putting.
A few key socioeconomic challenges include:
- Limited access to quality healthcare facilities
- Poor insurance coverage or high out-of-pocket costs
- Lack of flexible work schedules to allow for screenings
- Lower educational attainment leading to reduced health literacy
These factors work together to create a setting where missed screenings are common. It is not just about personal choices; these are the tangled issues that are deeply rooted in system-level inequities. Addressing such factors requires societal and policy-level changes that make screening services more accessible and affordable.
Medical Mistrust and Communication Gaps
The history of healthcare in the United States is riddled with episodes that have fostered deep-seated mistrust, especially among Black populations. Over generations, experiences with inequitable treatment have contributed to a widespread wariness about preventive care services. When the healthcare system is perceived as a daunting or even intimidating place, it makes it even tougher for individuals to schedule screenings or follow through with treatment recommendations.
This mistrust is often compounded by communication gaps between healthcare providers and patients. The fine points of patient–provider interaction, such as clear explanations, sensitivity to cultural backgrounds, and acknowledgment of individual concerns, are key to improving trust. When providers take the time to figure out a path that considers these subtle details, patients are more likely to engage fully in their care. However, until these gaps are bridged, the process of managing one’s own health remains nerve-racking at best.
Overcoming Tricky Parts in Colorectal Cancer Prevention
Despite the many off-putting obstacles, there have been encouraging success stories and strategies that have resulted in higher rates of screening and better outcomes. Planning and implementing programs that take into account the specific needs of Black communities have started to pay dividends. Here, we dig into some of these promising approaches and discuss how they can be replicated on a larger scale.
Improving Screening Participation: Lessons from Community Outreach Programs
Over the years, tailored community outreach initiatives have demonstrated that colorectal cancer screening disparities are not insurmountable. Programs that are culturally sensitive and specifically designed for Black communities have shown measurable improvements in screening rates. These initiatives often include:
- Local education campaigns that clearly explain the importance of early detection
- Collaborations with trusted community leaders and churches to spread awareness
- Mobile screening clinics that bring services directly to under-served neighborhoods
- Patient navigation services to help individuals set up appointments and complete follow-up care
For instance, some cities have organized screening drives that not only provide free or reduced-cost colonoscopies but also offer supportive counseling to overcome fears and concerns. By aligning these efforts with the community’s values and expectations, the intimidating notion of a medical screening begins to change into an accessible, community-supported step toward prevention.
Success Stories That Inspire Wider Change
Several case studies in metropolitan regions demonstrate that when initiatives are tailored to the community’s needs, the improvement in screening rates is both measurable and sustainable. One notable example is the comprehensive health programs initiated in certain urban centers where screening rates have improved by nearly 20–30% within a few years. These outcomes underscore a critical point: when you have the right support and proper communication, even the most nerve-racking procedures can become a routine, manageable part of healthcare.
The strategies that worked well include:
| Strategy | Description | Impact |
|---|---|---|
| Community Health Fairs | Events focused on education, screening, and direct support. | Increased awareness and higher screening participation. |
| Patient Navigator Programs | Assigning trained individuals to assist patients through the healthcare process. | Reduced no-show rates and timely follow-ups. |
| Mobile Clinics | Bringing screening services to community centers and neighborhoods. | Greater accessibility, especially in remote areas. |
These initiatives show that with carefully planned outreach efforts, the seemingly overwhelming gaps in service can be bridged over time.
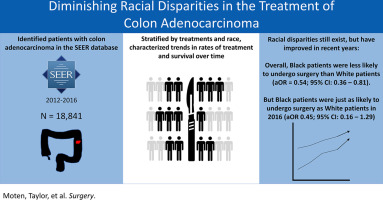
Examining Treatment Pathways and Survival Outcomes
Screening is only one piece of the puzzle in addressing colorectal cancer disparities. Even when screenings take place, the journey through treatment can be fraught with challenges that lead to differences in survival outcomes. The next piece of the discussion focuses on the twists and turns of treatment disparities and the need for timely, guideline-based care.
Barriers to Timely Treatment in Disadvantaged Communities
Following an abnormal screening result, the road to treatment is often complicated by a number of real-world obstacles. Studies have shown that Black patients frequently experience delays in diagnostic testing, surgery, and subsequent therapies compared with White patients. These delays can be attributed to several factors:
- Limited availability of specialists in under-resourced areas
- Complicated referral systems that add extra layers of waiting time
- Financial constraints that limit access to high-quality treatments
- Subtle biases in the way treatment options are presented or recommended
When everything is bundled up with these confusing bits, the result is a series of nerve-racking delays that can lead to poorer survival outcomes. Addressing these issues means not only improving the coordination of care but also ensuring that all patients, regardless of background, get prompt access to the best available treatments.
Guideline-Concordant Treatment: The Need for Standardization
Despite progress in therapy and surgical techniques, a persistent gap remains in the receipt of guideline-concordant treatment for colorectal cancer among Black patients. This term refers to medical care that strictly adheres to the latest standards and protocols, which have been proven to improve survival rates.
Some of the key elements of such treatment include:
- Standardized diagnostic workups
- Timely surgical interventions
- Consistent use of adjuvant chemotherapy when indicated
- Close monitoring and follow-up care after the primary treatment
The tough part is ensuring that every healthcare provider—regardless of region or resources—has the training and infrastructure needed to offer such consistent care. When guideline-driven care is implemented widely, the small distinctions in outcomes between Black and White patients begin to shrink significantly.
Digging Deeper: Social Factors Versus Biological Risk
There has been considerable debate about whether the differences in outcomes are largely due to underlying biological factors or if they are the result of social determinants that generate tangled issues over time. The majority of evidence now points to the conclusion that social and economic factors play a far more significant role than intrinsic biological differences.
Many studies have highlighted that the subtle parts of risk—such as lifestyle, nutritional habits, and exposure to environmental toxins—are heavily influenced by socioeconomic status. In fact, when both groups have equal access to screening and treatment, the differences in outcomes narrow up considerably. This suggests that what might have once been considered inherent risk differences are likely driven by modifiable, external factors.
The following points illustrate this viewpoint:
- Variability in diet and nutrition across different socioeconomic groups
- Differences in stress levels and exposure to adverse life events
- Access to preventive services and follow-up care
- Environmental exposures and occupational hazards
When you poke around the data, the evidence clearly suggests that social determinants largely account for these racial disparities. Supporting policies, such as those aimed at reducing financial barriers and improving overall community health, have the potential to mend these fine points of disparity.
Addressing the Tricky Parts: Dual Approaches to Systemic Change
The challenges in colorectal cancer care for Black individuals cannot be solved with a single strategy. Instead, a dual approach is essential: one that tackles the near-term issues like screening participation and timely treatment, and another that addresses the long-term structural barriers embedded within society.
Short-Term Interventions: Boosting Access and Adherence
In the immediate sense, strategies that improve access to high-quality screening and treatment are super important. These include better patient navigation services, enhanced community outreach, and programs that financially buffer patients from the intimidating costs associated with care.
The following short-term measures are worth noting:
- Enhanced Patient Navigation: Programs to help patients figure a path through complicated referral processes can reduce delays.
- Outreach and Education: Culturally tailored education programs that explain the importance of early screening and adherence to treatment protocols.
- Financial Assistance Programs: Reduced direct expenses through subsidies or charity care initiatives to lower the nerve-racking burden of treatment costs.
- Community Health Partnerships: Alliances between hospitals and community organizations to ensure care is accessible and trusted.
These interventions are not only designed to encourage early detection but also to ensure that once a problem is found, patients receive standardized, guideline-driven treatment quickly.
Long-Term Solutions: Tackling Systemic Inequities
While immediate measures are necessary to reduce the current gap, long-term change requires addressing the underlying social determinants that fuel disparities. Policies aimed at improving the socioeconomic conditions in disadvantaged areas can have a ripple effect on healthcare outcomes. Such policies may include:
- Investment in Education: Higher levels of education can lead to better health literacy, empowering patients to take control of their health.
- Economic Empowerment Initiatives: Job training and employment programs that lift communities out of poverty, thereby reducing the economic barriers to accessing care.
- Healthcare Infrastructure Improvements: Building more community-based clinics and expanding public health services in under-resourced regions.
- Policy Reforms in Healthcare Coverage: Medicare, Medicaid, and other insurance policies should be refined in order to make high-quality care accessible to all socio-economic groups.
These long-term solutions are designed not only to address the immediate screening and treatment gaps, but also to improve the overall social structure that contributes to such inequities. It is a dual approach where the fight against colorectal cancer begins on two fronts: the clinic and the community.
Spotlight on the Fine Points: How Community Health Drives Change
A closer look at several initiatives across different states provides an illuminating perspective on how well-planned community health programs are making a difference. These programs, which are usually tailored to meet the needs of specific neighborhoods, have managed to slowly but surely reduce the racial disparities in both screening and treatment outcomes.
Local Health Initiatives and Their Impact
In many urban centers, community-based organizations are working closely with healthcare providers to disseminate critical information about colorectal cancer. Local health fairs, free screening events, and patient education workshops are now common sights in many cities. These initiatives offer a practical solution by:
- Reducing the nerve-racking fear associated with medical screenings
- Helping individuals figure out a path for accessing care without getting lost in bureaucratic red tape
- Providing culturally sensitive information that resonates with the target community
When people see familiar faces and trusted community leaders involved in these efforts, the overwhelming sense of mistrust can begin to fade. It is a positive step toward balancing the scales of cancer care equity.
Comparative Data and Success Metrics
Data from several pilot programs reveals an encouraging trend: when Black individuals have been provided with targeted support, the rate of timely screening and subsequent treatment has improved significantly. Below is a simplified table summarizing some of the outcomes observed in these community-driven projects:
| Intervention Type | Outcome Measured | Observed Improvement |
|---|---|---|
| Patient Navigation | Screening Follow-Up Rates | +25% increase |
| Community Outreach | Screening Participation | +20% increase |
| Mobile Screening Clinics | Accessibility in Rural/Urban Areas | Expanded service reach by 30% |
This data is a hopeful reminder that, with the right strategies in place, even the most complicated obstacles can be overcome through community engagement and systemic reforms.
Hidden Complexities in Data Interpretation
While statistics and studies are critical in understanding colorectal cancer disparities, it is important to recognize that the data itself presents a mix of hidden complexities. The methods used to collect, analyze, and compare data across different populations can sometimes lead to confusing bits that need careful interpretation.
For example, many of the studies rely on historical data, which might not fully capture recent improvements in screening and treatment rates. Additionally, differences in reporting methods, geographic variations, and even the shifting demographics of communities all contribute to a picture that is as much about data challenges as it is about the real-world impact of disparities.
Researchers and policymakers must therefore dig into the numbers with a critical eye, acknowledging both the strengths and limitations of current studies. The goal is to use this information to highlight the small distinctions that can point the way toward more equitable healthcare solutions in the future.
Taking the Wheel: Policy Implications and Future Directions
The discussion on colorectal cancer disparities is not restricted to the medical community alone. Policymakers have a super important role to play in shaping the future of cancer care. By implementing reforms that directly address the root causes of inequity—be it through healthcare policy, education initiatives, or economic support programs—governments can make strides in reducing the gaps in care.
Policy Changes for Better Access and Equity
Some key areas for policy reform include:
- Improving Insurance Coverage: Expanding public health insurance programs to reduce out-of-pocket costs, which are a common barrier for low-income patients.
- Investing in Local Healthcare Infrastructure: ‘Taking the wheel’ in community clinics and mobile health units can help ensure that quality care is within reach for everyone.
- Strengthening Patient Protection Laws: Ensuring that all patients receive guideline-concordant care irrespective of race or economic status.
- Funding for Community-Based Research: Supporting projects that specifically aim to uncover the tangled issues behind healthcare disparities and test innovative solutions in real-world settings.
The dual approach—one that combines immediate, clinic-based interventions with long-term structural reforms—could ultimately eliminate many of the barriers that currently hinder equitable colorectal cancer care in Black communities.
Future Research Directions and Community Engagement
Looking ahead, research will play a key role in charting the path forward. Future studies need to continue to explore both the subtle details of treatment differences and the overall impact of improving socioeconomic conditions on cancer outcomes. Equally, it is important that research findings are translated into community action. When healthcare providers, researchers, and community leaders work together on projects that are directed by real-world needs, the resulting progress is often both impressive and sustainable.
Some promising directions for future research include:
- Exploring innovative screening technologies and methods that are simple to administer and less intimidating.
- Evaluating the long-term impact of community-based interventions on both screening rates and survival outcomes.
- Examining data on post-treatment quality of life to better understand whether improvements in survival are matched by improvements in day-to-day living.
- Investigating the effects of policy changes in real-time as communities adjust to new standards of care and improved economic conditions.
As researchers continue to take a closer look at these areas, the insights gained will not only help refine the interventions but also provide policymakers with the evidence needed to justify investments in addressing these tough, systemic issues.
Conclusion: A Call to Chart a Clear Path Forward
The disparities in colorectal cancer outcomes between Black and White communities in the United States represent one of the most pressing public health challenges of our time. As we have explored, the issue is layered with many nerve-racking twists and turns—from socioeconomic conditions and access to care to communication gaps and policy shortcomings. Yet, there is a clear message emerging from the research and community experiences: when targeted and culturally sensitive interventions are applied, progress is possible.
There is no silver bullet to fix every complicated piece of this problem, but there is substantial evidence that a combination of short-term strategies and long-term policy reforms can pave the way for more equitable outcomes. By boosting screening participation through community engagement and patient navigator programs, ensuring that treatment is timely and adherent to best practices, and by addressing the underlying social determinants of health, we can begin to flatten the uneven curve of colorectal cancer outcomes.
In the end, the call for change is super important—not only for those directly affected by colorectal cancer but for the overall health of our communities as well. Every patient deserves access to quality, guideline-based care, regardless of their background. With sustained investment, ongoing research, and a steadfast commitment from both health professionals and policymakers, it is entirely possible to overcome the intimidating barriers and make real progress toward health equity.
This opinion editorial is meant to stir a conversation—a call to action for all stakeholders involved—to figure a path toward dismantling the tricky parts of systemic inequity. By working together, we can make colorectal cancer screening and treatment not just a hopeful possibility but a realized promise for every individual, regardless of race or socioeconomic status.
Ultimately, the future of colorectal cancer care depends on our collective ability to take responsibility for the overlooked details, address the overwhelming challenges with persistent effort, and, most importantly, offer every patient a fair chance at a healthier life. The road ahead may still have its confusing bits and nerve-racking moments, but with the right approach, we can steer through the obstacles and ensure that quality healthcare is a reality for all.
Originally Post From https://www.nature.com/articles/s41575-025-01087-3
Read more about this topic at
Eliminating Racial Disparities in Maternal and Infant Mortality
Reducing disparities in health care