Partial Breast Radiotherapy as a New Standard in Early-Stage Breast Cancer Treatment
In recent years, the field of radiation oncology has witnessed an evolution in treatment options that simplify the tricky parts of traditional full-breast radiotherapy. In early-stage breast cancer patients with low risk of recurrence, partial-breast and reduced-dose radiotherapy have emerged as promising alternatives that appear to be as safe and effective as whole-breast irradiation. This opinion editorial examines the recent findings from the phase 3 UK IMPORT LOW trial, discussing the long-term results, patient selection criteria, and the potential of these techniques to reshape standard care practices internationally.
Clinical studies, including the 10-year analysis from the IMPORT LOW trial, provide critical insights into both the clinical outcomes and the subtle details of dose management, treatment planning, and adverse event profiles. By taking a closer look at these findings, health professionals and patients alike can better understand how modern treatment protocols may alleviate some of the nerve-racking aspects of cancer therapy while maintaining a high standard of care.
Understanding the IMPORT LOW Trial Findings
The IMPORT LOW trial was designed to compare traditional whole-breast radiation with two experimental approaches: reduced-dose radiation that combines whole-breast treatment with a boost to the partial breast, and partial-breast radiation alone. With 2,018 patients enrolled, the study meticulously followed patients over a median of 10 years to assess outcomes such as ipsilateral breast tumor recurrence (IBTR), locoregional recurrence, distant recurrence, and overall survival rates.
One of the major takeaways from this long-term study is that partial-breast radiotherapy—as delivered via intensity-modulated radiation techniques—demonstrated excellent long-term efficacy. The trial showed that the incidence of IBTR at 10 years was remarkably low in all groups, with the partial-breast radiation group reporting only a 3.0% incidence compared to 2.8% in the whole-breast group. Moreover, the reduced-dose approach exhibited a similar low recurrence rate of 1.9%, reinforcing that a smaller volume of irradiated tissue does not compromise treatment effectiveness.
Key Outcomes and Statistical Comparisons
For clinicians and patients alike, the reassuring findings of the IMPORT LOW trial provide confidence in adopting these less extensive radiation protocols. Here are some principal outcomes that emerged from the study:
- Ipsilateral Breast Tumor Recurrence (IBTR):
- Whole-Breast Radiation: 2.8%
- Reduced-Dose Radiation: 1.9%
- Partial-Breast Radiation: 3.0%
- Locoregional Recurrence:
- Whole-Breast Radiation: 3.2%
- Reduced-Dose Radiation: 1.9%
- Partial-Breast Radiation: 3.5%
- Distant Recurrence:
- Rates across groups hovered around 3.8%–4.1%
- All-Cause Mortality Rates:
- Whole-Breast Radiation: 12.3%
- Reduced-Dose Radiation: 13.1%
- Partial-Breast Radiation: 9.8%
These statistical findings, derived from a robust, multi-center, randomized trial, illustrate that the reduced irradiated volume does not translate into an increased risk of recurrence. Instead, it supports the rationale for a tailored approach in treating patients with low-risk early-stage breast cancer.
Detailed Comparison of Radiation Protocols
To understand the potential benefits of partial-breast radiotherapy, it is essential to compare the three different approaches:
| Parameter | Whole-Breast Radiation (40 Gy/15 fractions) | Reduced-Dose Radiation (36 Gy/15 fractions to the whole breast + 40 Gy/15 fractions to the partial breast) | Partial-Breast Radiation (40 Gy/15 fractions to the partial breast) |
|---|---|---|---|
| IBTR at 10 Years | 2.8% | 1.9% | 3.0% |
| Locoregional Recurrence | 3.2% | 1.9% | 3.5% |
| Distant Recurrence | 3.8% | 4.1% | 3.8% |
| All-Cause Mortality | 12.3% | 13.1% | 9.8% |
This table underscores the close similarity in outcomes among the different techniques. With every approach delivering results with minimal differences, it is clear that partial-breast radiotherapy holds promise as a standard treatment option, streamlining the approach for the appropriate patient population.
Exploring the Advantages of Partial Breast Radiation
One of the most appealing aspects of partial-breast radiotherapy is its potential to minimize some of the overwhelming side effects commonly associated with full-breast irradiation. By reducing the volume of breast tissue that is exposed to radiation, the technique helps limit damage to surrounding healthy tissue and reduces the chance of late adverse effects. These factors are of super important consideration for patients who already face a nerve-racking diagnosis.
Reduction in Adverse Effects: A Closer Look at Patient Benefits
The trial’s data revealed that clinician-reported outcomes, such as moderate to marked breast shrinkage, occurred in less than 10% of patients in each treatment arm. This finding is significant because it suggests that despite reducing the irradiated area, patients did not experience a greater risk of cosmetic or functional deficits over the decade-long follow-up.
Consider the following bullet list to recap some of the key benefits of the less extensive treatment:
- Maintaining favorable cosmetic outcomes with minimal breast shrinkage
- Potentially reduced exposure to secondary cancers—non-breast tumors occurred less frequently in the partial-breast group
- Lower incidence of long-term complications such as rib fractures, symptomatic lung fibrosis, and ischemic heart disease
- Preservation of patient quality of life over a prolonged period
These reduced long-term risks are not only comforting from a clinical standpoint but also address the emotional and physical well-being of patients who might find the array of treatment side effects to be overwhelming.
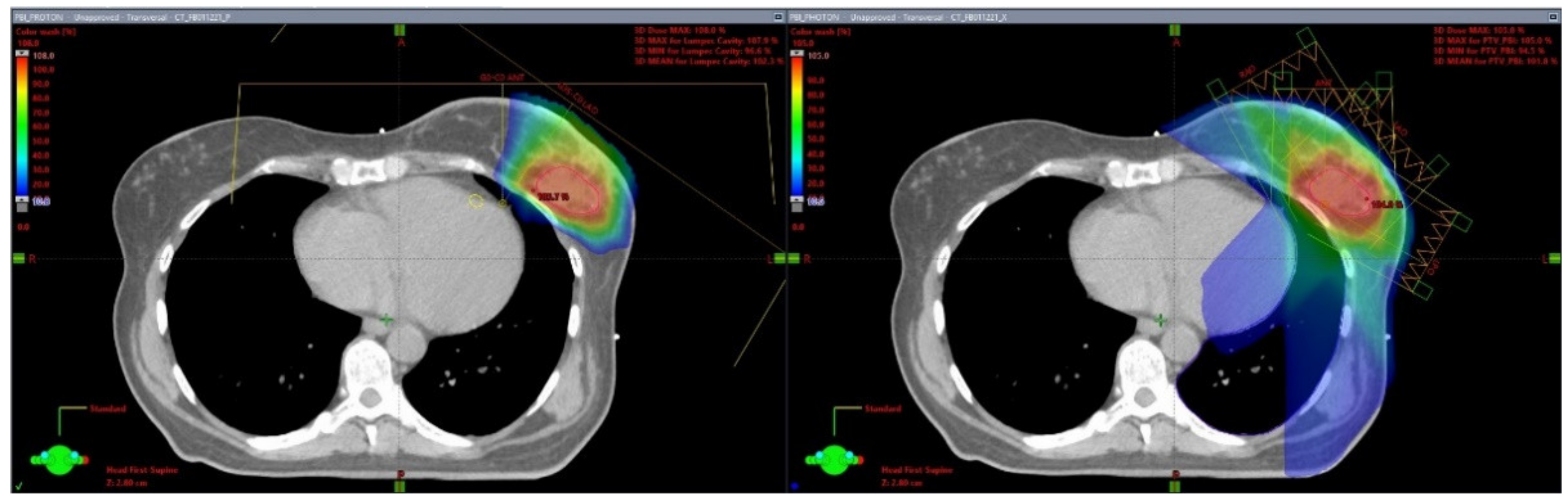
Intensity-Modulated Radiation Therapy: Modern Precision in Action
Intensity-modulated radiation therapy (IMRT) has made it possible to deliver precise radiation doses, even when targeting a reduced volume of breast tissue. This state-of-the-art approach allows clinicians to steer through the hidden complexities of treatment planning, ensuring that the selected portion of the breast is treated effectively while minimizing exposure to surrounding organs.
An important aspect of IMRT is its ergonomic design to get around the tricky parts of dose fractionation. By keeping the same fractionation schedule as whole-breast radiation (15 fractions in the IMPORT LOW trial), the technique avoids altering the overall dosing regimen—an approach that is both familiar and super important for patient assurance.
Practical Implications: Streamlining Treatment for Patients
For many patients, cancer therapy can feel like navigating a maze full of daunting twists and turns. The option of partial-breast radiotherapy offers a simpler path with several practical advantages:
- Shorter Treatment Duration: With fewer side effects, there is potential for fewer follow-up interventions and reduced time in treatment sessions.
- Minimized Exposure: Limiting the irradiated volume can preserve non-cancerous tissue, meaning patients might experience fewer long-term complications.
- Enhanced Quality of Life: A more tolerable side effect profile can help patients feel more comfortable during and after treatment, contributing to physical and mental well-being.
For patients whose treatment journey may already feel intimidating, these benefits can make a significant difference. With experienced oncologists and tailored care strategies, the shift towards partial-breast radiotherapy appears to be a positive development in modern oncology.
Patient Selection Criteria and Clinical Considerations
Not every patient is a candidate for partial-breast radiotherapy. The IMPORT LOW trial specifically targeted women over the age of 50 with low-risk, early-stage breast cancer. Eligible patients had tumors measuring 3 cm or less, unifocal disease, and minimal nodal involvement. This careful selection ensures that only those patients who are most likely to benefit from reduced radiation exposure are offered this treatment.
Understanding Eligibility: Who Benefits Most?
The criteria set forth by the trial help define a group of patients for whom partial-breast radiotherapy can be confidently recommended. These include:
- Age: Typically, patients aged 50 and older
- Tumor Size: Tumors of 3 cm or smaller are considered ideal
- Nodal Status: Patients with no more than 1 to 3 positive axillary nodes
- Histological Type: Invasive adenocarcinoma that displays a less aggressive behavior
Other exclusion criteria, such as previous malignancies (barring nonmelanoma skin cancer), prior endocrine or chemotherapy treatments, and concurrent chemoradiation, were integrated to ensure the trial’s outcomes would reflect a more homogenous patient population. Such careful selection helps steer through the messy terrain of patient variability, ensuring that treatment recommendations are based on solid, long-term evidence.
Clinical Decision-Making: Weighing the Options
For clinicians, the decision to opt for partial-breast rather than whole-breast radiotherapy involves balancing the benefits and potential risks while considering each patient’s unique clinical picture. The following factors are key when making this choice:
- Recurrence Risk: Both reduced-dose and partial-breast techniques have shown similar recurrence rates compared to whole-breast radiation, making them a viable option for low-risk patients.
- Adverse Effects: With a lower rate of long-term side effects, partial-breast irradiation is appealing for patients concerned about post-treatment quality of life.
- Patient Preference: For many, the possibility of a shorter, less toxic treatment plan is a compelling reason to choose partial-breast radiotherapy.
Ultimately, this tailored approach empowers patients and clinicians to figure a path that prioritizes long-term health outcomes with a reduced burden of treatment-related complications.
Balancing Safety and Efficacy in Radiotherapy Techniques
The safety profile of partial-breast radiotherapy has been a subject of considerable interest. Data from the IMPORT LOW trial demonstrate that despite the reduction in the irradiated volume, the incidence of treatment-related adverse effects such as breast shrinkage, rib fractures, lung fibrosis, and ischemic heart disease remained controlled and comparable across treatment arms.
Comparative Safety: Weighing the Risks
In examining the 10-year follow-up data, several points stand out:
- The incidence of moderate to marked breast shrinkage was below 10% in all treatment groups.
- Reports of adverse events, such as rib fractures and lung fibrosis, were minimal and numerically similar between whole-breast and partial-breast treatments.
- The overall mortality rates did not indicate any safety concerns related to the reduced irradiated volume.
These findings are particularly encouraging for patients and providers facing the confusing bits of treatment side effects. The data suggest that less can indeed be more, particularly in a subset of low-risk early-stage breast cancer patients.
The Role of Follow-Up and Long-Term Monitoring
While the results are promising, continuous follow-up remains key to ensuring that any late-occurring adverse events are identified and managed. The long-term surveillance strategies employed in clinical practice can help capture subtle changes over time, allowing medical professionals to refine treatment protocols if necessary.
In this context, it becomes super important for both patients and providers to engage in an ongoing dialogue about what to expect during and after treatment. Frequent check-ups, imaging studies, and discussions around quality of life can help address any nerve-racking uncertainties that may arise long after the initial therapy.
Impact on Clinical Practice and Future Research Directions
The encouraging outcomes from the IMPORT LOW trial are poised to have a ripple effect across clinical practice. By integrating partial-breast radiotherapy into the standard care repertoire, oncologists can offer a treatment option that caters to both the physical and emotional needs of patients with early-stage breast cancer.
Changing the Clinical Landscape
Here are some ways in which the trial’s findings are likely to influence current clinical practice:
- Simplified Treatment Pathways: Adoption of partial-breast radiotherapy can streamline the treatment process by reducing the irradiated tissue volume without compromising effectiveness.
- Patient-Centered Care: With fewer side effects and comparable outcomes, patients may be more receptive to treatment plans that offer not only clinical efficacy but also improvement in quality of life.
- Reduction in Healthcare Burden: Fewer treatment-related complications can potentially decrease the need for supplemental interventions, thereby alleviating part of the strained healthcare resources.
The evidence not only supports the safe use of partial-breast radiotherapy but also challenges the long-held belief that a more extensive volume of irradiation is inherently superior for all patients. This perspective shift encourages the oncology community to re-evaluate the standard protocols and look into more efficient, patient-friendly alternatives.
Future Studies and Emerging Questions
Even as the IMPORT LOW trial brings robust reassurance, several questions remain that future research should address:
- Could further dose reduction or alternative fractionation schedules yield additional benefits for certain patient subsets?
- What are the long-term psychosocial outcomes for patients receiving partial-breast radiotherapy compared to those undergoing whole-breast treatment?
- How might advances in imaging and radiation planning technologies further refine patient selection and treatment targeting?
- Will similar approaches prove effective in other types of cancer where radiation-induced side effects are a substantial concern?
These emerging questions underscore the need to continue probing into the fine points of radiation therapy and to conduct additional studies that build on the encouraging data from the IMPORT LOW trial. Future trials that integrate novel biomarkers, patient-reported outcomes, and advanced radiation planning could provide deeper insights into how best to tailor treatments for individual patients.
The Broader Implications for Oncology and Patient Care
Moving beyond the immediate context of breast cancer treatment, the success of partial-breast radiotherapy heralds a broader shift in oncology. As medical professionals take a closer look at how treatment can be both effective and less burdensome, there is an increased focus on personalized care that considers the overall well-being of patients.
Personalized Treatment Plans for Better Outcomes
In today’s oncology landscape, the ideal treatment achieves two key goals: eradicating cancer and preserving quality of life. Partial-breast radiotherapy aligns with this goal by offering a strategy that minimizes the risk of adverse effects while delivering robust tumor control. This is particularly important for a patient group that may already be dealing with various emotional and physical stressors amid their treatment journey.
Clinicians are now more than ever encouraged to work through the subtle distinctions between different radiotherapy techniques. This means carefully evaluating not only the clinical trial data but also understanding each patient’s individual situation.
Key components of this personalized approach include:
- Risk Stratification: Using detailed patient profiles—including age, tumor size, nodal involvement, and overall health—to determine the most suitable treatment option.
- Shared Decision-Making: Involving patients in the discussion about the benefits and potential challenges of each treatment option, thereby ensuring that their concerns are addressed.
- Ongoing Surveillance: Implementing long-term follow-up measures to monitor and address potential late effects while reinforcing the confidence in the chosen treatment plan.
Through these strategies, oncology care evolves into a more patient-centered model, one that prioritizes both efficacy and quality of life—a balance that is, in many ways, the cornerstone of modern cancer care.
The Role of Multidisciplinary Collaboration
The shift towards more tailored radiation therapy requires close collaboration among different specialties. Surgeons, radiation oncologists, medical oncologists, radiologists, and even allied health professionals must all work together to figure a path that optimizes patient outcomes.
Some of the benefits of such a multidisciplinary approach include:
- Enhanced Treatment Planning: Bringing various expert perspectives to the table can help address the tricky bits and tangled issues of dosage distribution and target delineation.
- Improved Patient Monitoring: Regular multidisciplinary meetings ensure that changes in patient status are identified early and managed appropriately.
- Comprehensive Support Systems: Integrating psychosocial support with clinical care can help patients navigate the intimidating aspects of their treatment journey.
Personal Reflections: Embracing Change in Cancer Therapy
As an observer in the rapidly evolving field of oncology, I find these developments deeply inspiring. The progress reflected in the IMPORT LOW trial not only highlights improvements in the technical delivery of radiation but also underscores a broader shift towards treatments that prioritize the patient experience. The idea that less can sometimes be more—when applied thoughtfully and based on robust evidence—resonates with both clinicians and patients.
The long-term data instill confidence that a reduced volume of irradiated tissue does not translate to inferior outcomes, but rather may deliver comparable efficacy with fewer of the nerve-racking long-term side effects that patients often dread. This is a classic example of how rethinking traditional approaches, and being open to innovation, can lead to tangible improvements in healthcare delivery.
Addressing Concerns and Misconceptions
Despite these promising advancements, some patients and practitioners may still have reservations about adopting a new approach that deviates from what has long been considered standard practice. Here are some common concerns and how they are being addressed:
- Fear of Incomplete Treatment: Many worry that targeting only a portion of the breast might leave behind microscopic disease. However, the IMPORT LOW trial data dispel this concern by demonstrating that local recurrence rates remain acceptably low with partial treatment.
- Uncertainty About Long-Term Outcomes: The 10-year follow-up in this trial provides reassuring evidence that the outcomes are stable over a significant period, alleviating fears about late recurrences or delayed adverse effects.
- Concerns Over Cosmetic Results: With less breast tissue irradiated, there is a decreased likelihood of significant cosmetic changes, which is an important quality-of-life factor for many patients.
By addressing these concerns head-on and emphasizing the robust data behind partial-breast radiotherapy, the oncology community can help patients and their families feel more comfortable with the idea of a treatment that is both effective and less burdened by long-term complications.
Looking Ahead: The Future of Radiotherapy in Breast Cancer
The promising outcomes of partial-breast radiotherapy signal the beginning of a new era in cancer treatment where the focus is not solely on survival statistics but also on the overall well-being of patients. As research continues and technology advances, we may well see further refinements in treatment protocols that drive even better patient outcomes.
Future studies may explore:
- Optimized Fractionation Schedules: Research into alternative dosing regimens could further minimize side effects while maintaining excellent control over the tumor.
- Integration of Molecular and Genetic Markers: Tailoring radiotherapy based on individual tumor biology could enhance the personalization of care, leading to even more targeted treatments.
- Technological Enhancements: Advancements in imaging and delivery systems have the potential to make dose distribution even more precise, reducing the impact on adjacent healthy tissues.
- Patient-Reported Outcome Measures: Incorporating feedback directly from patients will continue to inform best practices as we work to optimize both the physical and emotional aspects of cancer care.
Each of these areas represents not only an opportunity for clinical improvement but also a commitment to addressing the hidden complexities of cancer treatment by focusing on both the evident and subtle needs of patients.
Integrating New Research into Clinical Guidelines
It is crucial that the valuable insights gained from studies like the IMPORT LOW trial be disseminated widely and integrated into clinical guidelines. This ensures that the benefits of partial-breast radiotherapy are appreciated not only by academic institutions but also by community-based cancer centers where the majority of patients receive care.
By updating national and international protocols, the oncology community can provide clinicians with the confidence to adopt this approach, knowing that it is backed by rigorous long-term data. The dissemination process involves:
- Incorporating trial findings into continuing medical education (CME) modules
- Publishing detailed analyses in peer-reviewed journals
- Hosting workshops and expert panels to discuss practical applications and emerging data
Conclusion: A Step Forward in Patient-Centered Oncology
The evolution of radiotherapy in early-stage breast cancer represents an exciting chapter in modern oncology. The IMPORT LOW trial has opened the door to treatment options that not only maintain robust tumor control but also lessen the side effects that can make cancer therapy feel overwhelming and off-putting.
Partial-breast radiotherapy, along with reduced-dose approaches, is gradually reshaping the cancer treatment landscape by emphasizing precision, patient quality of life, and a more tailored approach to care. As we take a closer look at these developments, it becomes evident that the future of cancer therapy lies in strategies that carefully balance efficacy with the overall well-being of patients.
For patients, this means having access to treatments that respect their quality of life while providing the best possible outcomes. For clinicians, it emphasizes the importance of personalized, evidence-based planning that addresses both the obvious and the subtle challenges of cancer care.
In the coming years, ongoing research, technological progress, and the continued refinement of treatment protocols will likely further reduce the intimidating side effects associated with radiotherapy. The journey of figuring a path through modern therapy may still be full of twists and turns, but studies like IMPORT LOW guide us along a safer, more efficient road.
Ultimately, embracing partial-breast radiotherapy is not just an adjustment of technical parameters, but a thoughtful embrace of a model that champions patient-centered care. It is a model that prioritizes reduction in complications, timely management of side effects, and above all, a commitment to sustaining quality of life amidst the battle against cancer. As we continue to work through the tangled issues of treatment selection and long-term monitoring, the future holds promise for oncology practices that are both innovative and deeply compassionate.
Originally Post From https://www.cancernetwork.com/view/partial-breast-radiation-appears-effective-safe-in-early-breast-cancer
Read more about this topic at
Radiation therapy for breast cancer
Radiation for Breast Cancer