Repositioning FDA-Approved Drugs in Prostate Cancer Treatment: A New Frontier
The field of prostate cancer treatment is experiencing a defining moment as researchers work to find clever ways to work around the tangled issues posed by conventional therapies. Prostate cancer, which is a leading cause of death among American men, particularly when it has advanced into castration-resistant prostate cancer (CRPC), has historically been a tricky area for treatment development. Today, an innovative approach aims to take advantage of FDA-approved drugs and repurpose them to make prostate cancer cells more vulnerable to polymerase inhibitors, sparking a hopeful change in treatment strategies.
Filling the Unmet Treatment Gap in Resistant Prostate Cancer
For years, physicians and researchers have grappled with the problem of CRPC cell resistance to androgen-deprivation therapy. While recent advancements, such as the approval of Olaparib, provide promising avenues for patients who harbor defects in their DNA repair genes, the reality remains that over 70% of prostate cancer patients do not possess these mutations. This leaves a massive gap in effective treatment options, raising concerns about the available standard of care.
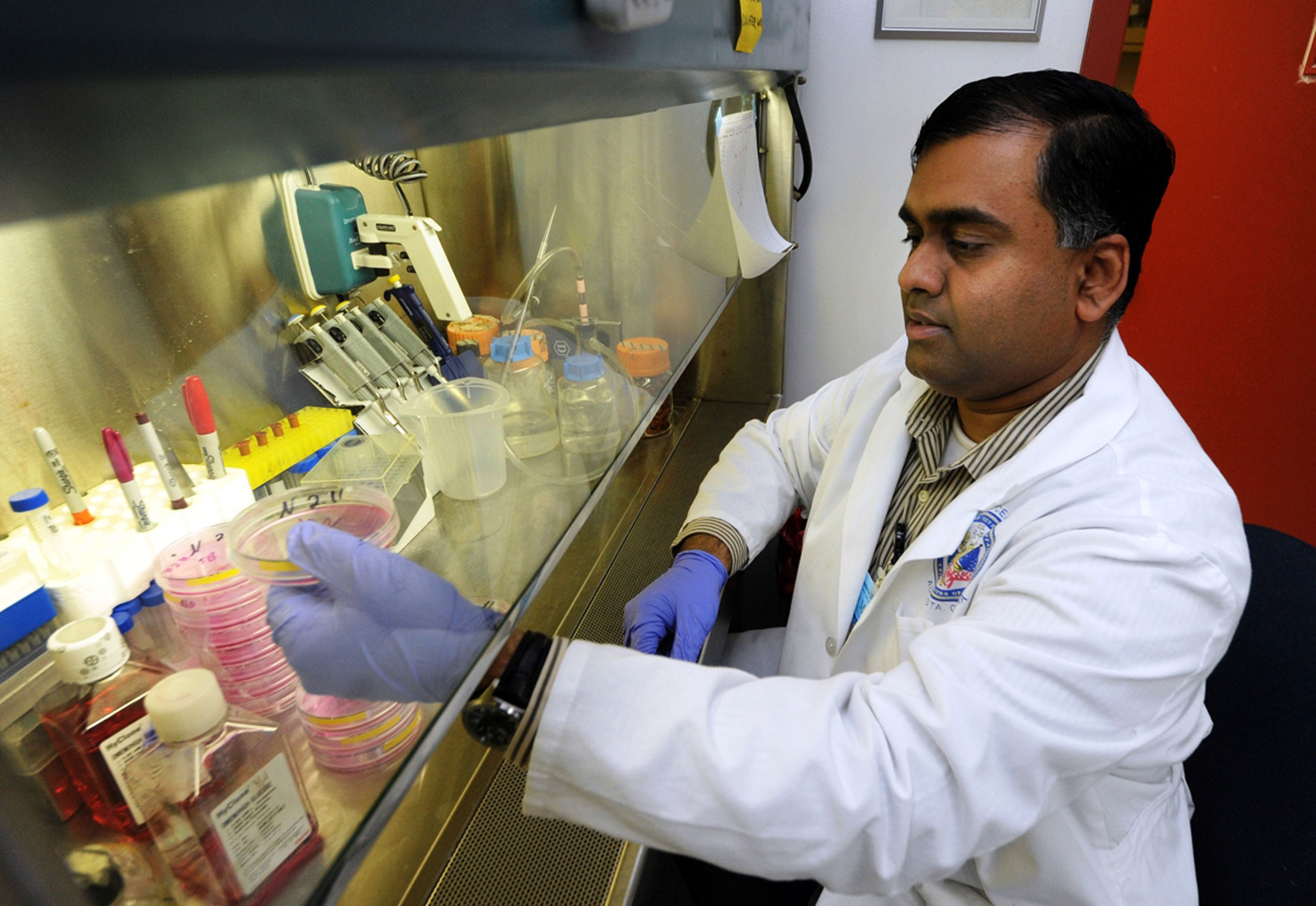
Chunhong Yan, PhD, a renowned professor of biochemistry and molecular biology at Augusta University, is at the forefront of an effort to tackle this challenge head-on. His groundbreaking research on mitochondrial uncoupling for prostate cancer therapy seeks to create opportunities by using already approved cancer treatments in a novel way. The idea is to sensitize prostate cancer cells—even those with intact homologous recombination repair (HRR) genes—to PARP inhibitors, a class of drugs traditionally used when HRR defects exist.
This approach is akin to repurposing traditional combat tactics for a new kind of war, allowing a fresh angle to probe the subtle parts of prostate cancer’s resistance mechanisms. By strategically using drugs that impact mitochondrial events, Yan’s research is poised to open doors for a broader spectrum of prostate cancer patients.
Understanding the Mitochondrial Uncoupling Strategy
The Role of Mitochondrial Events in Cancer Cell Vulnerability
Mitochondrial uncoupling is an emerging concept that involves disrupting the normal function of the mitochondria—the powerhouses of the cell—to induce a state of vulnerability in cancer cells. In Yan’s work, the focus is to precipitate a scenario where even cancer cells that do not exhibit traditional HRR gene mutations become susceptible to DNA repair disruption through PARP inhibitors.
This strategy works by targeting the “tangled issues” found in the mitochondrial energy production process. When mitochondrial function is compromised, prostate cancer cells may become less capable of managing the induced DNA damage, ultimately leading to their death. This approach essentially uses the cell’s own energy machinery as a fulcrum to tilt the balance toward cell death, offering a potential new therapeutic window.
- Disrupt normal energy production pathways
- Enhance sensitivity to PARP inhibitors
- Create conditions leading to accumulation of unrepaired DNA damage
- Expand the scope of therapy to patients with intact HRR genes
The idea is both clever and practical: rather than waiting for the natural occurrence of specific genetic mutations, why not create conditions where even cells with functional repair systems become overstressed and vulnerable? This innovative tactic brings us a step closer to a solution that could transform the treatment landscape for a majority of CRPC patients.
Beyond Conventional Treatments: Repositioning Old Drugs for New Purposes
Advantages of Drug Repositioning in Prostate Cancer Therapy
One of the key benefits of this new approach is the repositioning of drugs that have already received FDA approval. By repurposing established medications for a different therapeutic use, researchers can bypass many of the nerve-racking stages associated with the introduction of entirely new drugs. This strategy brings with it several important advantages:
- Speedy clinical deployment: Existing drugs come with known safety profiles and can be moved into new clinical contexts more rapidly than completely novel compounds.
- Cost-effectiveness: Utilizing drugs that have already been approved reduces the overall financial burden associated with drug development.
- Expanding treatment options: A broader array of patients—especially those not carrying HRR mutations—may benefit from therapies that were previously effectively off the table for them.
The process is reminiscent of taking a well-known key and using it in a newly discovered lock. Although the tool itself remains unchanged, its application is refined and redirected to solve a different problem. As Yan puts it, the objective is to “dig into” the fine points of mitochondrial biology to exploit the inherent vulnerabilities in prostate cancer cells.
Tackling the Limitations of HRR-Targeted Therapies
Understanding the Restrictions of Current Approaches
While PARP inhibitors such as Olaparib have shown promise, their use is largely restricted to patients who have mutations in their HRR genes. This has left a major portion of CRPC patients without a valuable treatment option. Here’s a closer look at the limitations of current therapies:
| Aspect | Current HRR-Targeted Therapy | Proposed Mitochondrial Uncoupling Approach |
|---|---|---|
| Patient Eligibility | Less than 30% of patients have the necessary genetic mutations | Broader coverage, including HRR-intact cells |
| Mechanistic Basis | Exploiting a pre-existing defect in DNA repair | Inducing vulnerability via mitochondrial disruption |
| Clinical Utility | Effective for patients with compromised DNA repair pathways | Potentially effective for a larger patient population |
| Development Timeline | Utilizes established drugs; similar pathway | Involves repurposing existing compounds in a novel way |
This clear comparison highlights how the mitochondrial uncoupling tactic could be a game-changer—turning an approach that was once reserved for a small group into one that could be available to many more men battling prostate cancer.
Overcoming the Intimidating Challenge of Drug Resistance
The challenge is significant: how do we overcome the nerve-racking hurdles imposed by cancer cell resilience? Current therapies, while promising in certain settings, fall short when it comes to addressing the off-putting reality that many cellular processes can compensate for the damage caused by treatment. Prostate cancer cells, with their ability to adapt and survive, present a particularly imposing set of obstacles.
By using a two-pronged strategy—first destabilizing the energy regulation system within the mitochondria, then applying the DNA-damaging action of PARP inhibitors—the new approach aims to throw a wrench into the cancer cells’ ability to repair damage. It’s like forcing a well-oiled machine to work with missing gears; even a slight disturbance in the rhythm can lead to systemic breakdown.
Implications for Other Cancer Treatments: A Broader Perspective
Exploring the Potential in Breast and Ovarian Cancers
While Yan’s current focus rests on prostate cancer, the insights gained from this research have wider implications. The underlying mechanism of mitochondrial uncoupling and PARP inhibition could, in theory, be applied to other cancers where similar challenges exist. For instance, certain types of breast and ovarian cancers also demonstrate difficulties in treatment due to intact DNA repair pathways.
When we look at the promising preclinical data for prostate cancer, it ignites the possibility of adapting the strategy for a range of cancers that have been hesitant to respond to traditional treatments. In such cases, the process of “poking around” in cellular energy clusters might reveal vulnerabilities that can be systematically exploited across various tumor types.
Here’s a brief look at how similar techniques might benefit other cancer treatments:
- Breast Cancer: Some subtypes, especially those with triple-negative profiles, can be notoriously difficult to manage. If mitochondrial uncoupling can make these cells more susceptible to DNA damage, a similar therapeutic window may open.
- Ovarian Cancer: Like prostate cancer, certain ovarian cancers have intact DNA repair systems that currently limit the utility of PARP inhibitors. Adjusting mitochondrial function could broaden treatment options for these patients.
This cross-applicability not only enhances our understanding of cancer biology but also fosters a more unified approach to cancer care. Rather than being confined by the conventional categories defined by genetics alone, researchers can build comprehensive strategies that incorporate metabolic vulnerabilities across the board.
Financial Backing and Community Support: The Role of Innovative Fundraising
How Paceline and Community Initiatives Propel Cancer Research
Research of this caliber does not happen in isolation and comes with its own set of challenging bits—financial limitations and the need for robust community backing. Since 2019, Paceline has been a crucial supporter for innovative cancer research at the Georgia Cancer Center, raising nearly $1.7 million. Their involvement is a reminder that effective cancer treatments require both scientific brilliance and community commitment.
Paceline’s signature fundraising event, PaceDay, now includes a diverse format with options such as walking, running, and biking. This inclusive approach not only helps raise funds but also fosters a sense of solidarity among supporters and patients alike. The following are some of the key benefits this support network delivers:
- Research Enablement: Financial contributions allow researchers to explore new and untested ideas without the constraint of lacking monetary resources.
- Community Engagement: PaceDay, and similar events, create bridges between researchers and the community, emphasizing that combating cancer is a collective effort.
- Future Funding: Continued support can open the doors to long-term clinical trials and further research innovations, possibly expanding successful protocols to other cancer types.
Community-driven support is a must-have component in this battle against cancer, ensuring that the scientific community’s discoveries do not remain confined to the lab but are translated into real-world treatments that can benefit millions.
Assessing Safety and Efficacy in Preclinical Trials
Using Genetic Mouse Models for Safety Evaluation
An essential part of this pioneering research involves confirming that the new treatment strategies are not only effective but also safe. Yan and his team are currently using genetic mouse models to assess the safety profile of the proposed therapy. This stage of research is critical, as it provides preliminary data on how healthy cells and tissues react when subjected to the dual assault of induced mitochondrial uncoupling and PARP inhibition.
Key areas of investigation during the preclinical phase include:
- Toxicity Assessments: Determining whether the newly combined treatment causes significant adverse reactions in vital organs.
- Dose Optimization: Finding the correct balance between efficacy and safety for the re-purposed drug combinations.
- Side-Effect Profiling: Charting out any unanticipated side effects that may be encountered with this new therapeutic approach.
- Long-Term Impact: Evaluating whether the treatment leads to any lasting damage or benefits the overall survival rate in preclinical models.
The results garnered from these studies will be crucial in laying the groundwork for human clinical trials. Researchers expect that within the next three to four years, the accumulated data could lead to the design of clinical studies, potentially ushering in a new era for patient care. This part of the process might seem nerve-racking at times, but it is indispensable in ensuring that any new treatment does more good than harm.
Charting the Clinical Trial Roadmap for Future Therapies
The Journey from Bench to Bedside
Bringing a new treatment idea from the research lab to the clinic is a journey filled with twists and turns that require careful planning and execution. The current preclinical findings will serve as the cornerstone for the design of future clinical trials. If successful, these trials could lead to wider use of the dual-therapy approach in an attempt to rescue a spectrum of prostate cancer patients who have not benefited from conventional treatments.
Some of the critical steps involved in this journey include:
- Data Collection and Analysis: The research team will continue to gather detailed safety and efficacy data using genetic models.
- Protocol Development: Based on initial results, investigators will craft clinical trial protocols that outline dosage, treatment duration, and patient selection criteria.
- Regulatory Review: The safety data acquired during preclinical testing must clear regulatory hurdles before any human trials can commence.
- Phase I Trials: The first phase of human trials will focus on evaluating the safety and pharmacokinetics of the re-purposed treatment in a small group of patients.
- Phase II/III Trials: Subsequent trials will assess treatment efficacy across a broader patient population, fine-tuning various therapeutic parameters along the way.
The overall objective is to create a streamlined but rigorous process that not only paves the way for better treatment options but also ensures that these innovations are both safe and effective. Researchers remain cautiously optimistic as they chart a path through the fine details of treatment design, always keeping the patient’s quality of life at the center of their mission.
Expert Perspectives on Overcoming Research Hurdles
Voices from the Scientific Community
It is important to acknowledge that revolutionary approaches like mitochondrial uncoupling for enhanced PARP inhibitor sensitivity come with their own sets of challenges. Many experts in the field have weighed in on the promise and pitfalls of using drug repositioning to overcome the tangled issues of prostate cancer treatment.
Renowned researchers appreciate that while the idea of repurposing drugs is not new, the combination of targeting mitochondrial function infused with DNA repair inhibition represents a bold step forward. Key points raised include:
- Scientific Innovation: Using well-understood drugs in unconventional ways can sometimes reveal unexpected benefits, offering a fresh perspective on managing recurrent cancers.
- Clinical Translation: Many believe that this dual approach could pave the way for treatments that might eventually extend survival and improve the quality of life in patients facing an intimidating diagnosis.
- Challenges in Data Interpretation: Given the complexity of cancer biology, understanding the fine shades of response to combined therapies will require careful interpretation of both preclinical and clinical data.
- Collaborative Efforts: The success of these initiatives will heavily depend on collaboration among research institutions, funding agencies, and community support groups.
By taking a closer look at these subtle parts of the research process, industry experts are learning to steer through the complications of cancer treatment more methodically. They emphasize that every promising idea, no matter how exciting, must undergo rigorous testing and validation before turning into a standard-of-care option.
Connecting Research to Patient Impact
The Human Element in Scientific Discovery
Behind every new scientific advancement, there is a deeply personal story of patients and their families grappling with the overwhelming challenges of cancer. The push to repurpose FDA-approved drugs to widen the therapeutic window for prostate cancer is not just a scientific pursuit—it is a mission driven by the real-world need to save lives and enhance the quality of care available.
Patients who do not carry the necessary HRR gene mutations for standard PARP inhibitor treatment have, until now, faced a limited horizon when it comes to effective treatment options. The research led by Dr. Yan and his colleagues offers hope by potentially expanding the available choices for a much larger group of men. It is an endeavor that underscores the true meaning of medical innovation: bringing tangible benefits to those who need them the most.
This focus on the human element serves as a powerful reminder that breakthroughs in medicine must eventually translate into better clinical outcomes. As the research progresses, every incremental step brings us closer to a future where patients—regardless of their genetic profile—can benefit from cutting-edge therapies available today.
Integrating Diet, Lifestyle, and Alternative Approaches
Complementing Therapy with Nutrition and Fitness
While the advancements in drug repositioning and mitochondrial uncoupling are critical, they also highlight the need for a holistic approach to cancer care. Nutrition, alternative medicine, and physical fitness continue to play a supportive role in managing the overall health of cancer patients. The integration of these elements is super important for several reasons:
- Improved Treatment Tolerance: A balanced diet and regular exercise can help patients better tolerate the side effects of aggressive therapies.
- Mental and Emotional Well-being: Activities such as yoga, meditation, and other complementary approaches contribute to reducing stress and improving quality of life.
- Enhanced Immune Response: Good nutrition and fitness can boost overall immunity, helping the body fight off infections and potentially aiding in recovery.
By integrating these lifestyle factors, patients can play an active role in their treatment journey. While novel therapies continue to evolve in the laboratory, supportive care measures are already making a difference in the lives of many struggling with cancer. The approach is truly comprehensive—combining groundbreaking scientific research with everyday practices that collectively contribute to better health outcomes.
Looking Ahead: Future Directions and Collaborative Efforts
Building a Roadmap for Continued Innovation
As we stand at the cusp of potentially transformative changes in prostate cancer treatment, it is clear that the journey ahead will require sustained collaborative efforts across multiple disciplines. Researchers, clinicians, funding agencies, and community organizations must continue to work together to bring innovative ideas from the lab bench to the patient’s bedside.
Looking to the future, several key directions stand out:
- Expanded Clinical Trials: With robust preclinical data, it is anticipated that clinical trials will soon test the effectiveness of the mitochondrial uncoupling strategy across a wider patient base.
- Cross-Cancer Applications: Success in prostate cancer could serve as the model for similar approaches in treating other cancers where DNA repair mechanisms are intact, such as certain breast and ovarian cancers.
- Personalized Medicine: Future treatments may increasingly incorporate personalized assessments of metabolic and genetic profiles, allowing for finely tuned therapeutic interventions that cater to each patient’s unique tumor biology.
- Ongoing Technological Advancements: Emerging technologies, including advanced imaging and genomic sequencing, will continue to reveal the fine details involved in cancer metabolism and treatment responses.
Each of these future directions represents a step toward a more comprehensive, refined, and ultimately successful battle against cancer. While challenges remain, the combination of scientific ingenuity, community support, and relentless passion for improving patient care provides a strong foundation for hope and progress.
Reflections on the Current Landscape and the Path Forward
Balancing Optimism with Careful Evaluation
Today’s developments in prostate cancer research and treatment are both inspiring and indicative of the long road ahead. While it is easy to get swept up in the promise of using FDA-approved drugs in innovative ways, it is equally important to remain realistic and cautious. All medical breakthroughs must withstand rigorous testing and validation, especially when dealing with such complicated pieces as cancer cells and their resilient behavior.
The work being undertaken by Dr. Chunhong Yan and his team exemplifies a balanced approach—one that is imbued with cutting-edge ideas yet grounded in meticulous preclinical evaluation. Their careful exploration of the mitochondrial uncoupling mechanism to induce vulnerability in prostate cancer cells is a testament to the combined power of traditional scientific methods and new-age innovation.
This balanced perspective is necessary for the following reasons:
- Patient Safety: No new treatment should ever compromise patient safety, and extensive preclinical studies ensure that any emerging therapy is thoroughly vetted before large-scale human trials begin.
- Scientific Rigor: The research community must continue to probe into the subtle details that could make or break a new therapy, leaving no stone unturned in the process of validation.
- Ethical Considerations: The potential expansion of treatment options carries with it important ethical implications, underscoring the need for fairness and accessible care for all patients.
By remaining optimistic yet meticulously careful, the scientific community can ensure that breakthroughs are implemented in a manner that truly benefits patients while upholding the highest standards of safety and efficacy.
Conclusion: A Step Toward a More Inclusive Treatment Paradigm
Charting the Future of Prostate Cancer Care
The innovative repositioning of FDA-approved drugs to make prostate cancer cells more vulnerable to PARP inhibitors represents an exciting evolution in the treatment of CRPC. While the traditional pathway of leveraging HRR mutations has left the majority of patients without new treatment options, this fresh strategy holds promise for expanding the benefit of targeted therapies to those previously excluded from such advances.
By strategically targeting mitochondrial function, researchers are opening up avenues to create a more inclusive treatment paradigm—one that acknowledges and exploits the subtle parts of cancer cell metabolism. This research is not only a beacon of hope for prostate cancer patients but may also have broader implications for other challenging cancer types. With continued support from innovative fundraising initiatives like Paceline’s PaceDay and unwavering dedication from the research community, the path forward looks promising.
Ultimately, this work synthesizes the cutting-edge with the practical: it repurposes proven drugs in new ways and complements these advances with robust preclinical testing and community engagement. As this multifaceted approach evolves, it holds the potential to redefine how we manage one of the most intimidating forms of cancer, offering hope to hundreds of thousands of patients who have long awaited improved therapies.
As we continue to figure a path through the maze of cancer research, it is clear that the journey is as important as the destination. Every new insight brings us closer to transforming confusion into clarity, mistrust into hope, and limitations into opportunities. The work of Dr. Yan and his team shines as a model of how modern medicine can thrive by adapting existing tools to confront nerve-racking challenges, ultimately paving the way for a future where cancer care is more effective, inclusive, and compassionate.
In reflecting on the strides made and the challenges that lie ahead, it is essential to recognize that this is a collective effort—a harmonious blend of scientific endeavor, community spirit, and unwavering resolve to improve the lives of those touched by cancer. With this collaborative spirit, we can look forward to a future where every patient finds a treatment that is as unique and dynamic as they are.
Looking ahead, it is the responsibility of the entire healthcare community to continue pushing boundaries, questioning the status quo, and embracing innovative approaches that convert today’s research into tomorrow’s standard of care. In so doing, we honor the lives impacted by cancer and reaffirm our commitment to making meaningful, transformative progress in the battle against this pervasive disease.
Originally Post From https://jagwire.augusta.edu/georgia-cancer-researcher-filling-gap-in-prostate-cancer-treatment/
Read more about this topic at
Bridging Treatment Implementation Gaps in Patients With …
Bridging Treatment Implementation Gaps in Patients With …


