Medication and Breastfeeding: An Opinion on Balancing Health and Practicality
The connection between taking medicines and the decision to continue breastfeeding is a topic filled with twists and turns that affects countless new mothers. When a woman is faced with the need to take medication, the challenge of figuring a path between her own well-being and the benefits of breastfeeding becomes complicated. In this editorial, we take a closer look at how medication use influences breastfeeding continuation and why clearer, evidence-based guidance is essential for both mothers and healthcare professionals.
Over the years, research has shown that many medicines that are life-saving or supportive of health are, in fact, safe for breastfeeding mothers. Yet, a significant number of women opt to stop breastfeeding when faced with the need to take certain medications—a decision that might be more related to conflicting or off-putting advice than to any real risk. This editorial aims to poke around the key issues, pointing out both helpful and nerve-racking aspects of the problem.
Understanding the Decision-Making Process
The decision for a breastfeeding mother to discontinue breastfeeding while on medication is rarely a black-and-white issue. Rather, it’s a process replete with little details that are often tangled with medical advice, personal concerns, and cultural expectations.
Tricky Parts of Medication Safety and Breastfeeding
Many healthcare professionals have the responsibility to give guidance on medicine use during breastfeeding. However, the advice can sometimes be confusing or even too cautious. The following points outline critical, yet sometimes overlooked elements:
- Limited safety data: Despite many drugs having enough post-marketing evidence to demonstrate safety, the exclusion of breastfeeding women from early clinical trials has led to a scarcity of robust information.
- Inconsistent Guidance: Guidance provided by healthcare professionals can be mixed. Some practitioners lean toward safety by suggesting breastfeeding cessation, while others encourage continuing the process with proper monitoring.
- Societal and personal concerns: A mother’s own worries about the potential risk to her child and external pressures from family or society add layers of complexity to her decision-making process.
These confusing bits result in decisions that might seem off-base when compared to the fine points of evidence-based research. Mothers might be led to discontinue breastfeeding even for medications that are classified as safe, reflecting the nerve-racking situation that often arises from over-cautious medical advice.
Healthcare Professionals’ Role in the Process
Healthcare professionals, including doctors, pharmacists, midwives, and lactation consultants, play an essential part in guiding mothers through this maze. Their advice can either soothe the worries or pile on additional stress. Some key points include:
- Influence of Clinical Experience: Many practitioners rely on their past experiences and ingrained caution when recommending a course of action. This can sometimes lead to unnecessarily advising a mother to stop breastfeeding.
- Access to Resources: There are several trusted resources—such as LactMed® and national breastfeeding support services—that provide updated safety information. However, these are not always well-known within general practice.
- Facing Legal and Ethical Concerns: Clinicians might sometimes play it safe due to fears of professional liability, which can result in overly conservative recommendations.
It’s important to note that when advice is given under pressure or without a full understanding of subtle details, the impacts on the mother’s well-being can be far-reaching. Mothers, after all, are making a decision that balances a lot of challenging factors. When a physician or midwife tells a mother to stop breastfeeding based on medication use, that advice can carry enough weight to overturn what might be a safe and beneficial practice.
Factors Influencing the Breastfeeding Decision
Mothers are influenced by a range of factors when faced with medication during breastfeeding. Some are rooted in consistent evidence, while others stem from socioeconomic and cultural backgrounds.
Personal Concerns and Socioeconomic Influences
Many women express personal worries about the impact of medications on their infants. These concerns are often magnified by external pressures. Some of the key personal and socioeconomic influencing factors include:
- Educational Background: Evidence indicates that mothers with lower educational levels may be more inclined to discontinue breastfeeding, partly because of less access to, or understanding of, the established safety profiles of many medications.
- Delivery Method and Early Experience: Factors such as birth via Caesarean section and fewer days of breastfeeding experience have also been linked to earlier cessation when medications are introduced.
- Employment Issues: Return to work and similar responsibilities have been identified as additional pressures influencing the decision-making process.
- Preexisting Health Behaviors: For example, mothers who smoked before pregnancy might be more predisposed to alter their breastfeeding routines when required to take medication.
All these elements contribute to making the decision both personal and complex. There is often a tension between trusting evidence-based guidance and responding to personal fears, which can be seen as both overwhelming and confusing for mothers who must manage their own health along with that of their infants.
Impact of Healthcare Advice on Breastfeeding Choices
Another layer to this issue is the actual advice provided by healthcare professionals. It is not uncommon for a mother’s choices to hinge on how her healthcare team communicates risk. Here are some of the subtle parts that play a role:
| Advisory Factor | Impact on Decision |
|---|---|
| Overly Cautious Advice | May lead mothers to stop breastfeeding unnecessarily, depriving them of essential health benefits. |
| Structured Support | Clear, evidence-based support from trained professionals can encourage continued breastfeeding, even when medication is needed. |
| Mixed Messages | Inconsistent guidance between different healthcare providers creates uncertainty, which can steer mothers away from breastfeeding. |
The table above lays out how different types of advice can influence the options that new mothers feel they have. In many cases, the overwhelming advice received is the product of a system that is still working through some of the tricky parts of modern medicine and its applications in postpartum care.
Reassessing the Evidence: Safety Profiles of Medications
A significant factor in this discussion is the safety profile of many medications. The evidence suggests that most medications, even those used for chronic conditions, are safe when breastfeeding, as long as they are used with appropriate guidance.
Examining Drug Safety and Post-Marketing Data
Despite the nerve-racking decisions that some mothers face, it is important to highlight that most medications have well-documented safety profiles derived from post-marketing evidence. Here is a quick look at what the research shows:
- Rheumatological Treatments: Drugs used in conditions like rheumatoid arthritis, including certain steroids and non-steroidal anti-inflammatory drugs (NSAIDs), are largely considered safe for breastfeeding mothers.
- Immunotherapies and Statins: Studies looking at medications for multiple sclerosis and familial hypercholesterolaemia indicate that these medicines are compatible with breastfeeding when managed carefully.
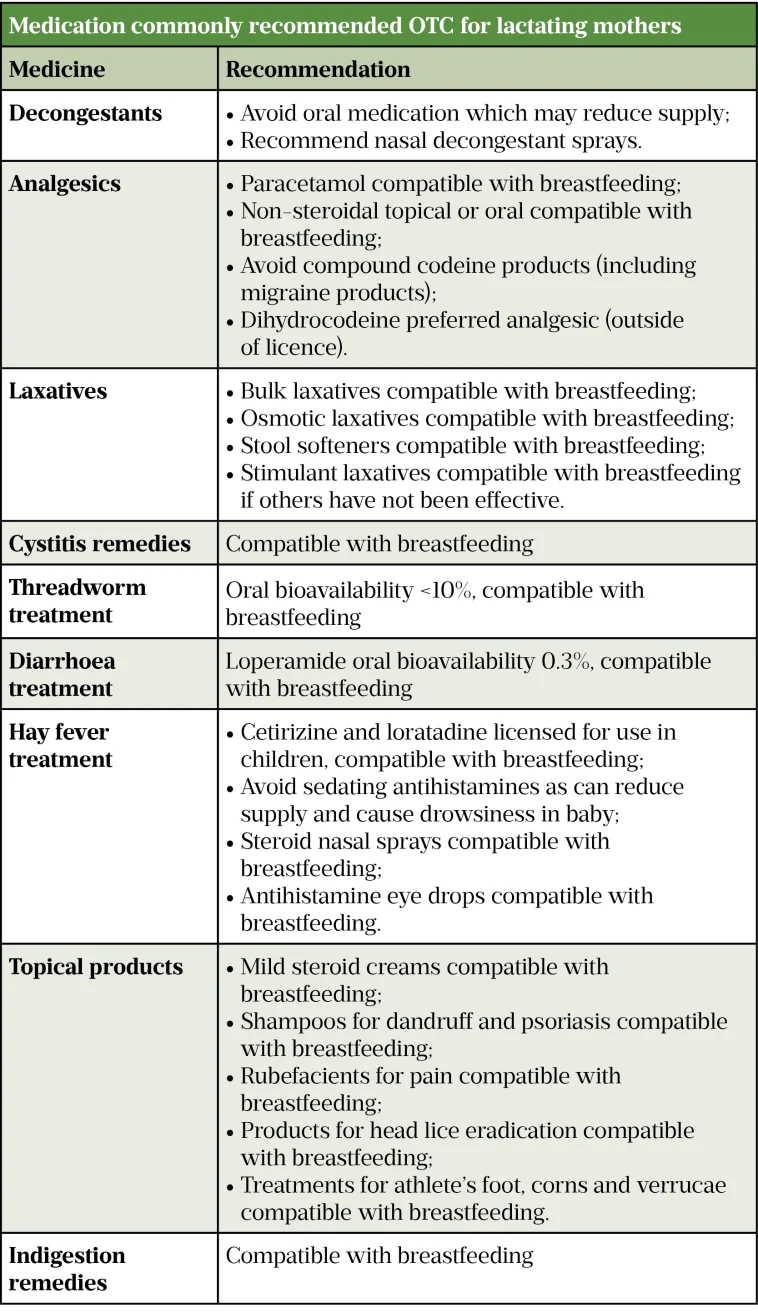
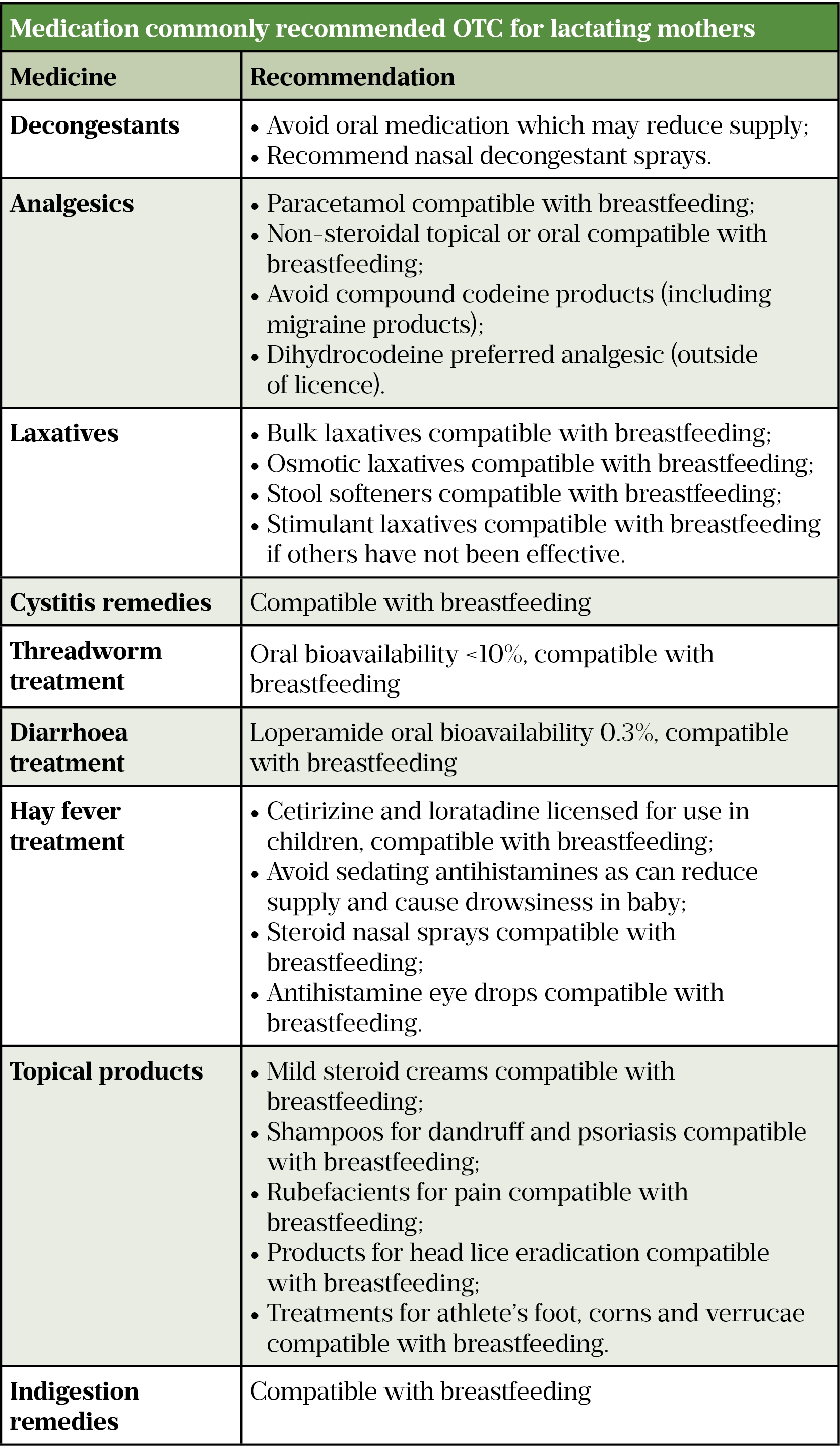
- Small Molecule Drugs: Many over-the-counter medications, including paracetamol and some antibiotics and vitamins, also fall into the category of safe for breastfeeding.
It is clear that the fine points of drug safety are well understood by pharmacologists. However, the challenge remains in translating that knowledge into everyday clinical practice in a way that is understandable, nuanced, and free of unnecessary alarm.
Overcoming the Over-Cautious Medical Culture
One of the more overwhelming issues in today’s healthcare environment is the tendency towards overly cautious medical advice. While it is essential to be safe, this caution sometimes ends up being counterproductive. Several factors contribute to this overly conservative approach:
- Lack of Specialized Training: Many healthcare providers may not have high-priority training in breastfeeding pharmacology, leading them to rely on outdated or generalized guidelines.
- Legal Liability Concerns: In a climate where legal action is increasingly common, some professionals might favor stopping breastfeeding over the potential risk—even if that risk is minimal.
- Information Gaps: The absence of regular updates to clinical guidelines means that many healthcare providers are left to make decisions based on incomplete or dated evidence.
By taking a closer look at these issues, it becomes evident that both the healthcare system and the individuals within it need to move towards more balanced and current advice. It is essential not only for patient safety but also for public health that mothers receive guidance that lets them make informed decisions.
Practical Strategies for Supporting Breastfeeding Mothers on Medication
Given the abundant evidence that many medications are compatible with breastfeeding, there is a pressing need to improve support systems and communication channels between mothers and healthcare providers. The following strategies are suggested for making better day-to-day decisions:
Improving Multidisciplinary Education
Enhanced education for healthcare professionals is a super important step in alleviating the nerve-racking choices mothers face. Key strategies include:
- Regular Training Sessions: Organize regular workshops and continuing education programs that focus specifically on medication safety in breastfeeding.
- Updated Resource Materials: Make available updated clinical guidelines and resources such as LactMed® and national formularies to all practitioners involved in maternal care.
- Interdisciplinary Communication: Promote better communication between obstetricians, paediatricians, pharmacists, and midwives to ensure consistency in advice.
Such multidisciplinary education not only benefits healthcare professionals but also directly translates into clearer, more consistent advice to mothers. With the right resources, these professionals can help new mothers steer through the confusing bits and find an informed path forward.
Enhanced Patient Information and Support Networks
For mothers, clear information is key to making the best health choices. Initiatives to support mothers should focus on:
- Accessible Information: Develop easily digestible informational materials that detail which medications are safe during breastfeeding and which may require caution.
- Peer Support Groups: Foster community-based support groups—both local and online—that allow mothers to share experiences and advice, reducing the sense of isolation when confronted with tricky medication choices.
- Direct Access to Specialists: Create systems allowing mothers to directly consult with lactation consultants and pharmacology experts who have current, evidence-based insights into medication safety.
A well-informed mother is more likely to trust her own judgment and the guidance provided by knowledgeable healthcare providers. When mothers feel confident about the small distinctions and subtle details regarding medication use and breastfeeding, they are better equipped to continue breastfeeding safely while taking necessary medications.
Tackling the Hidden Complexities of Research Gaps
While significant progress has been made in understanding the relationship between medication use and breastfeeding, many questions remain. It is crucial to point out the following distracting pieces of the research puzzle:
Gaps in Representing Diverse Populations
One of the major challenges in current research is the over-representation of certain demographic groups. The studies conducted to date largely involve well-educated, Caucasian women from high-income countries. This means that:
- Limited Generalizability: The findings might not hold true for women from minority ethnic backgrounds or lower socioeconomic classes, who could also be facing additional challenges related to breastfeeding.
- Cultural Differences in Decision-Making: Cultural beliefs and traditions about breastfeeding may strongly influence whether a mother feels comfortable continuing breastfeeding while on medication.
- Sparse Data on Personal Concerns: More qualitative research is needed to capture the small distinctions and personal conflicts that occur when a mother needs to decide on stopping breastfeeding due to medication.
Addressing these gaps is a key step in ensuring that future guidelines are representative and inclusive. When research reflects a wider range of experiences, the resulting advice becomes better tailored to support all mothers.
Need for Longitudinal Studies and Standardized Definitions
It is also important that future research clarifies what exactly is meant by “medication-related breastfeeding discontinuation.” Many studies have different definitions and study time points, making it difficult to compare data. Considerations for moving forward include:
- Standardized Definitions: Develop a clear, universally accepted definition of what constitutes medication-related breastfeeding discontinuation, differentiating between temporary and permanent cessation.
- Long-Term Follow-Up: Implement longitudinal studies that track breastfeeding outcomes well beyond the early postpartum months, ensuring that decisions made in the first few weeks do not lead to misinterpretation of long-term trends.
- Mixed-Methods Research: Combine quantitative data, such as incidence rates, with qualitative insights to get into the nitty-gritty of how and why decisions are made.
These approaches will help untangle the hidden complexities of current research and provide a more consistent basis for both clinical and policy decisions.
The Broader Implications for Public Health and Policy
Improving medication-related guidance for breastfeeding mothers isn’t just about individual health decisions—it also carries significant implications for public health. Clearer, consistent guidance can yield benefits such as:
- Enhanced Maternal and Child Health Outcomes: When mothers can continue breastfeeding safely, both they and their children enjoy long-term health benefits, from reduced infection rates in infants to a lower risk of chronic diseases in mothers.
- Reduced Healthcare Costs: Improved breastfeeding rates can lead to decreased reliance on formula feeding, with consequent reductions in healthcare and social costs.
- Empowered Communities: Better support and clearer information help reduce the stress and overwhelming feelings that come with the decisions around breastfeeding and medication, thereby empowering communities to make healthier choices.
At the policy level, these insights emphasize the need for a coordinated effort among healthcare institutions, governments, and non-profit organizations to ensure that pregnant and postpartum women receive super important advice that is up-to-date and inclusive of all lifestyles and backgrounds.
Policy Interventions That Could Make a Difference
Policymakers and healthcare administrators might consider several targeted strategies:
- Mandating Updated Training: Require regular, evidence-based training on breastfeeding pharmacology for all healthcare professionals involved in maternal care.
- Funding Inclusive Research: Direct research funding towards studies that include diverse populations and take a mixed-methods approach to capture the full range of experiences related to medication use and breastfeeding.
- Improving Information Dissemination: Launch public health campaigns that provide clear, easily digestible information about which medications are safe during breastfeeding and how mothers can access expert guidance.
- Interdisciplinary Collaboration: Support initiatives that bring together professionals from various fields—such as medicine, pharmacy, and community health—to create holistic care models for breastfeeding mothers.
Such interventions can help create a healthcare framework that truly reflects the fine points of evidence-based practice, ensuring that mothers are equipped to make informed choices without undue pressure or confusion.
Final Thoughts: Moving Toward Clarity and Confidence
In conclusion, the decision to discontinue breastfeeding due to the use of medication is a matter loaded with tricky parts, confusing bits, and many small distinctions. A large body of evidence suggests that for many medications, the benefits of continuing to breastfeed far outweigh the risks to the infant. However, the pathway to making a confident decision is often obscured by a mix of over-cautious advice, gaps in current research, and a lack of clear, inclusive guidance.
It is essential for both mothers and healthcare professionals to work together to solve the tangled issues surrounding this topic. For new mothers, having access to a well-informed support network—composed of healthcare experts, updated guidelines, and peer support—can make all the difference. With better education, more inclusive research, and policy interventions aimed at clarifying the fine points of medication safety, we can help reduce unnecessary shocks and overwhelming choices that lead to early cessation of breastfeeding.
This editorial calls for a balanced, evidence-based approach in supporting breastfeeding women who need to take medication. By tackling the hidden complexities and ensuring that all voices are heard, we can help mothers figure a path that not only protects their health but also secures the many documented benefits of breastfeeding for both child and mother.
Ultimately, the goal is to provide a system wherein mothers feel confident, supported, and empowered to continue breastfeeding under safe conditions—even when faced with the need to take medication. This is not just a personal issue for each mother, but a public health priority that stands to benefit families and communities as a whole.
As we continue to work through these twisted issues and fine-tune our approach, it remains super important for ongoing dialogue between researchers, clinicians, policymakers, and mothers. Only then can we hope to transform overwhelming challenges into manageable steps toward a healthier future for all.
Originally Post From https://internationalbreastfeedingjournal.biomedcentral.com/articles/10.1186/s13006-025-00756-y
Read more about this topic at
Breastfeeding and medications: What’s safe?
Drugs and Lactation Database (LactMed®)