Universal Alcohol Screening: A Fresh Perspective on a Growing Health Concern
Unhealthy alcohol use has long been a subject of discussion among healthcare professionals and public health advocates. With the newest recommendations from the U.S. Preventive Services Task Force (USPSTF), the call to screen all adults—even those who are pregnant—for unhealthy alcohol use is gaining momentum. In this opinion editorial, we take a closer look at the evidence behind these guidelines, consider the practical implications for primary care clinicians, and explore the various counseling methods that can make a significant difference in patients’ lives.
The USPSTF’s proposal to screen all adults is not just another guideline; it is a call for an approach that addresses the many tangled issues associated with alcohol consumption. Given that excessive drinking is linked to several chronic diseases and even death, the recommendation is both timely and critical. As we dive in, we will poke around the subtle parts of these guidelines and explore the strengths and potential challenges of universal screening, all while keeping in mind the essential need for practical interventions.
Alcohol Use in America: The Reality Behind the Numbers
The modern landscape of alcohol consumption in the United States is full of problems. According to the Centers for Disease Control and Prevention (CDC), nearly 17% of American adults engage in binge drinking and about 6% practice heavy drinking. This isn’t just a matter of individual behavior—it’s a public health crisis, with approximately 178,000 deaths attributed to excessive alcohol use each year. Beyond the statistics, there are also documented links between alcohol use and serious health conditions, such as breast cancer and colorectal cancer.
These figures highlight the critical need for early identification and intervention. With such overwhelming data, the USPSTF has set out to reduce the scary consequences of unchecked drinking by intervening before issues escalate to alcohol use disorders (AUD). Although the nuances of this topic are loaded with issues, the goal remains simple: to detect and address unhealthy alcohol consumption before it spirals into more complicated health problems.
Understanding the USPSTF Recommendation: Key Points
The USPSTF’s draft recommendation is built on a thorough evaluation of over 100 studies analyzing the effectiveness of screening strategies and behavioral counseling interventions. The core message is straightforward: all adults should be asked about their alcohol use habits during routine health appointments. For those who are identified as engaging in risky or hazardous drinking, counseling should be offered as a preventive measure.
According to Dr. John Ruiz, a task force member and clinical psychology professor, brief interventions can be a powerful tool to increase patients’ awareness of their intake and motivate behavior changes. These interventions might include brief advice, cognitive behavioral therapy, or motivational interviewing techniques—each tailored to the specific needs of an individual patient. The hope is that by addressing the issue early and clearly, healthcare providers can help reduce overall consumption and steer patients away from dangerous drinking patterns.
Alcohol Counseling Effectiveness: What Do the Numbers Say?
The evidence supporting the USPSTF’s recommendation shows that counseling interventions can lead to measurable reductions in alcohol intake. In systematic reviews referenced by the task force, participants who received some form of intervention reportedly reduced their alcohol consumption by an average of 1.6 drinks per week compared to those who received standard care. Although this might appear to be just a small difference on the surface, even minor reductions can translate into significant long-term health benefits.
It is important to notice that the studies reviewed did not just focus on the quantity of alcohol consumed. They also noted reductions in risky behaviors such as heavy episodic drinking. For pregnant women involved in trials, these interventions have been shown to help maintain abstinence—a key factor in preventing maternal and fetal complications. The numerical evidence thus underscores that early behavioral counseling offers an opportunity to change the course of unhealthy habits before they cause irreversible harm.
Screening for Unhealthy Alcohol Use: Essential Yet Challenging
Screening as a routine part of adult health management is not without its tricky parts. One of the most intimidating issues for healthcare professionals is how to integrate the screening process into already busy clinical schedules. Many primary care providers express concerns about time constraints and the nerve-racking nature of discussing alcohol use with patients, fearing a negative reaction or the inability to address a deeply personal topic adequately.
Additionally, the current recommendation puts forward the idea of universal screening for unhealthy alcohol use. While this may seem like a comprehensive strategy for identifying at-risk individuals, it also brings with it concerns about the fine points of implementation: the correct screening tools, follow-up assessments, and appropriate counseling techniques. However, these complicated pieces of the process can be managed effectively if clinicians are given the proper resources and training.
Effective Counseling Approaches: Multiple Paths to Positive Change
The discussion around alcohol use interventions is rich with a variety of counseling techniques that can be tailored to the needs of different patients. The USPSTF guidelines leave room for various approaches, such as brief advice, motivational interviewing, and cognitive behavioral therapy. Each of these methods offers its own style of engagement, and when applied properly, they empower patients to figure a path toward reducing their alcohol consumption.
Here are some of the key counseling strategies:
- Brief Advice: A short conversation that highlights the risks of unhealthy drinking and suggests immediate steps for reducing intake.
- Motivational Interviewing: A collaborative, patient-centered approach that involves asking open-ended questions and reflective listening to help the patient articulate their own reasons for change.
- Cognitive Behavioral Therapy (CBT): A structured approach that helps patients identify and alter patterns of thought and behavior related to their drinking habits.
These techniques are designed to make the often overwhelming challenge of behavior change more approachable, providing clear, actionable steps that patients can integrate into their daily lives. The key is for healthcare providers to work through the process alongside their patients, discussing the little twists of behavior change and gradually increasing patient awareness and motivation.
Addressing Risky Drinking: A Closer Look at Counseling Approaches
When we get into the realm of counseling for unhealthy alcohol use, it becomes apparent that one size does not fit all. Health care professionals (HCPs) should collaborate with their patients to select the approach that best meets their personal needs. Here’s a more detailed look at how each strategy can be deployed:
| Approach | Description | Key Benefits |
|---|---|---|
| Brief Advice | A short, structured conversation focusing on the risks of alcohol use and immediate recommendations for moderation or abstinence. | Quick to implement; effective for increasing awareness. |
| Motivational Interviewing | A patient-centered counseling style aimed at enhancing intrinsic motivation to change by exploring and resolving ambivalence. | Builds trust; empowers patients to change from within. |
| Cognitive Behavioral Therapy (CBT) | An approach that identifies and challenges negative thought patterns and helps develop healthier coping strategies. | Addresses underlying cognitive triggers; provides long-term tools for change. |
This table illustrates that each counseling strategy offers distinct advantages. Depending on the context and the patient’s individual needs, the clinician might even consider combining methods to maximize effectiveness. The goal is simple—to reduce harmful drinking habits before they give rise to more complicated and potentially dangerous health issues.
Special Considerations: Pregnant Women and Adolescents
While the guidelines strongly advise universal screening for all adults, including pregnant women, extra care must be taken when it comes to younger populations. The USPSTF has issued an I-grade recommendation for screening adolescents due to insufficient evidence to fully endorse or denounce the practice. This careful stance reflects the nuanced differences in alcohol metabolism, developmental risk, and potential outcomes that complicate screening in this age group.
For pregnant women, on the other hand, the recommendation underscores the critical importance of early detection. Alcohol use during pregnancy has been associated with severe complications, including fetal alcohol spectrum disorders. By screening all adults without exception, clinicians can ensure that pregnant women receive the necessary counseling to maintain abstinence or reduce consumption, thereby protecting both maternal and fetal health.
These differences highlight the tangled issues in developing broad public health guidelines. While universal screening offers a promising pathway to early detection, clinicians will need to use their judgment—particularly when dealing with adolescents—so as to provide the best care tailored to each individual’s circumstances.
Integrating Screening into Everyday Clinical Practice
Implementing universal screening in primary care settings is both a critical need and a notable challenge. Many healthcare providers view the addition of routine screening as an extra layer of responsibility that must be squeezed into an already-overwhelmed schedule. The process of integrating screening protocols involves not just asking patients about their alcohol consumption, but also ensuring a smooth follow-up process for those who may need in-depth counseling.
Some of the steps to effectively incorporate screening in everyday practice include:
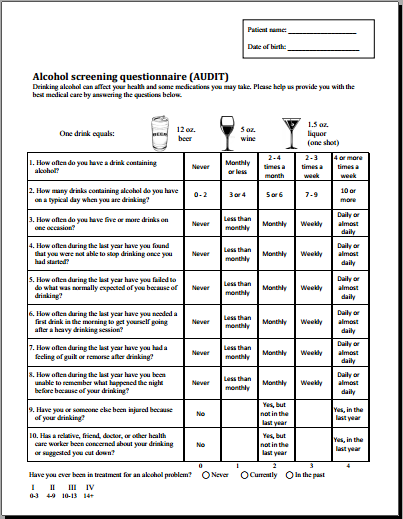
- Adopting Standardized Screening Tools: Tools such as the Alcohol Use Disorders Identification Test (AUDIT) are widely recommended to help clinicians quickly assess risk levels.
- Training Staff: By providing training on how to comfortably and effectively approach the subject, clinics can help reduce the nerve-racking nature of these discussions.
- Scheduling Follow-Up Appointments: For patients identified as at risk, timely follow-up ensures that counseling interventions are initiated without delay.
These measures can assist clinicians in sorting out and making their way through the implementation process. The integration of standardized screening tools provides an efficient foundation, while training and follow-up practices help to bridge the gap between identification and intervention.
Overcoming the Overwhelming Parts of Alcohol Counseling
Even with established guidelines and proven counseling techniques, the idea of addressing alcohol use with patients can still feel off-putting. Many clinicians may find the subject intimidating due to the potential for personal discomfort and the challenge of initiating a conversation about a behavior that can be deeply personal and surrounded by social stigma.
However, it is important to recognize that the benefits of early intervention far outweigh the initial awkwardness that may arise. By employing open-ended questions, providing nonjudgmental support, and offering clear options for behavioral change, providers can break through the barriers of stigma and foster an environment where patients feel empowered to share their true struggles.
Simple techniques, such as reflective listening and summarizing previous discussions, make the process less overwhelming. Patients begin to see that the intention is not to criticize, but to work together in finding the best path forward. These confidence-building measures are super important for patients, as they transition from risky drinking behaviors to healthier patterns over time.
Understanding the Fine Points of Screening and Counseling Together
One of the small distinctions that makes the USPSTF recommendation so promising is its focus on pairing screening with personalized counseling interventions. The minor act of asking patients about their drinking habits, when combined with a carefully selected counseling strategy, can serve as a turning point in a patient’s health journey.
This combined approach is designed to address both the behavioral and the cognitive aspects of unhealthy alcohol use. On one hand, screening provides the initial data point: it identifies those who are at risk. On the other hand, counseling interventions dig into the subtle, often hidden complexities of why an individual might engage in risky drinking habits. For example, a patient might not realize that stress or social pressures play a role in their drinking habits. With the right counseling approach, such as motivational interviewing, these issues can be uncovered and tackled head-on.
When a patient is invited to get into a genuine discussion about their alcohol consumption habits, even the confusing bits of behavioral change become more manageable. The healthcare provider works collaboratively with the patient to figure a path that incorporates both immediate interventions and long-term strategies for maintaining a healthier lifestyle.
Taking the Wheel: Empowering Patients Through Self-Management
Empowering patients to take control of their drinking habits is a key element of the USPSTF’s approach. Self-management strategies, when correctly adopted, offer a practical means to steer through the day-to-day challenges associated with reducing alcohol consumption. For many patients, the change begins with setting small, attainable goals:
- Deciding to reduce the number of drinks on heavy drinking days.
- Monitoring daily and weekly alcohol intake.
- Using tools like drinking diaries to track progress.
- Setting up reminders and accountability measures with the help of family, friends, or support groups.
These simple steps, though they might seem like minor adjustments at first, can significantly impact long-term outcomes. The person in control of their life is more likely to feel motivated and capable of evolving their behavior. This empowerment is at the heart of transforming risky drinking patterns into more sustainable, healthy habits.
Collaborative Efforts: The Role of Healthcare Providers and Policy Makers
While the USPSTF’s recommendation makes it clear that healthcare professionals play an essential role in this effort, it is also critical for policy makers to create an environment conducive to these practices. There are a few key areas where collaboration can help overcome the tricky parts involved in implementing universal screening:
- Funding for Training Programs: Investment in regular training sessions for clinicians can ensure that all providers are well-prepared to have these sensitive conversations with their patients.
- Enhanced Screening Tools: Ongoing research and development of streamlined screening tools can reduce the time and resources required to identify risky drinking behaviors.
- Community Awareness Campaigns: Public health campaigns that normalize the topic of alcohol use can lessen the social stigma associated with these discussions, making it easier for patients to open up.
- Improved Access to Counseling Services: Ensuring that patients have access to affordable counseling services can make the leap from screening to effective intervention smoother.
By finding your way through these challenges collaboratively, the healthcare community, along with policy makers, can deliver a more robust and effective system of care. This approach not only addresses the immediate signs of unhealthy alcohol use but also lays the groundwork for long-term improvements in public health outcomes.
Balancing Efficiency with Empathy in Primary Care
The drive to implement universal alcohol screening must be balanced with the need for empathetic and patient-centered care. The nature of discussing alcohol use can be nerve-racking for both providers and patients, particularly when the conversation touches on personal habits and lifestyle choices. However, balancing efficiency with empathy is key to ensuring that the intervention is meaningful and effective.
Here are some practical tips for healthcare providers to incorporate into their practice:
- Start with the Basics: A simple, respectful inquiry about alcohol use as part of the regular health assessment can ease the patient into a deeper conversation.
- Create a Judgment-Free Zone: Emphasize understanding and support rather than punishment, which helps patients feel more secure in discussing their habits.
- Follow-Up Consistently: Regular follow-ups can help maintain progress and adjust interventions as needed, ensuring that the patient does not feel left to navigate the tough bits alone.
- Use Personalized Goals: Working together with the patient to set clear, manageable goals makes the path to change feel more achievable.
These strategies not only improve the effectiveness of the screening process but also strengthen the patient-provider relationship, ensuring that patients are more likely to stick with recommendations over the long term.
Charting the Future of Alcohol Screening and Intervention
Looking forward, the USPSTF’s recommendation to screen all adults for unhealthy alcohol use signals an important shift in the approach to preventive healthcare. By embedding screening as part of routine patient assessments, the healthcare community can proactively reduce the rates of alcohol-related illnesses and build a more resilient public health framework.
Research must continue to explore the best methods to implement these guidelines efficiently, with an eye toward the little twists that make each patient’s journey unique. As more studies are conducted and more data are gathered, it is anticipated that screening tools and counseling methods will become even more sophisticated, allowing providers to find their way through the most complicated pieces of alcohol intervention.
Moreover, as debates continue regarding the screening of adolescents, it is essential to remain flexible and patient-centered. Leveraging the existing evidence while acknowledging the nerve-racking uncertainties of this area, healthcare professionals are encouraged to use their judgment and tailor their approach on an individual basis for younger patients.
Reflections on the Role of Universal Screening in Modern Healthcare
The push for universal screening is emblematic of a broader movement toward preventive care in modern medicine. By identifying unhealthy alcohol use early, primary care clinicians can intervene before the condition develops into a full-blown disorder that is loaded with problems. The approach is not about penalizing patients, but rather about offering support before a more serious crisis arises.
At its core, universal screening for alcohol use is a practical, evidence-based strategy that showcases the importance of early intervention. For many, the initial conversation about alcohol consumption might seem intimidating, yet it is a small price to pay for the potential to avoid more severe health complications down the road. The fine points, the subtle details, and even the challenging bits of behavior change must all be considered when designing interventions that are both effective and empathetic.
A Roadmap Toward Lasting Change
As we take a closer look at the proposed changes in alcohol screening, it becomes clear that a comprehensive approach is the best way forward. Here’s a brief roadmap to outline the steps needed for a successful transition toward universal screening and effective intervention:
- Education and Training: Ensure that all clinicians are well-trained in using standardized screening tools and understanding the range of counseling interventions available.
- Standardization: Adopt uniform protocols to assess alcohol use so that every patient receives a consistent and supportive evaluation.
- Follow-Up and Support: Establish a system for timely follow-up counseling and support, seamlessly integrated into regular patient care.
- Community Outreach: Launch campaigns to educate the public about the risks of unhealthy alcohol use and the benefits of early intervention.
- Ongoing Research: Continue gathering data on the effectiveness of different counseling strategies, ensuring that interventions remain responsive to emerging evidence.
This roadmap illustrates that while the path forward might have its twists and turns, the overall direction is clear: proactive, empathetic, and evidence-based care can make a significant difference in preventing alcohol-related health issues.
Conclusion: Embracing the Challenge for a Healthier Future
In conclusion, the USPSTF’s draft recommendation to screen all adults for unhealthy alcohol use marks a pivotal moment in preventive healthcare. It challenges providers to integrate routine screening and tailored counseling into everyday practice—a change that, despite its intimidating beginnings, promises substantial benefits for public health.
By using a combination of brief advice, motivational interviewing, and cognitive behavioral therapy, healthcare professionals have the tools to help patients navigate the tangled issues of risky drinking. As research continues and more evidence emerges, it is likely that these methods will evolve, further reducing the nerve-racking risks associated with unintended overconsumption.
While there are still many fine points to be ironed out—from effectively implementing these measures in busy clinical settings to addressing the specific needs of diverse populations—the underlying principle remains resolute: early intervention is the key to preventing more serious alcohol-related problems.
Ultimately, the call for universal screening is not merely about the numbers or the statistics. It is about recognizing the power of early conversation and collaboration between patients and providers. It is about taking that first small step, even if it feels overwhelming at first, and watching how that step can lead to a cascade of healthy changes—a journey that starts with a single question and the promise of better health outcomes for every individual.
For clinicians, policy makers, and patients alike, this is a moment to acknowledge that while the road to healthier living might be full of tricky parts and complicated pieces, the benefits of early, effective intervention are far too important to ignore. With the support and commitment of the entire healthcare community, we can not only manage today’s challenges but also steer toward a future where unhealthy alcohol use is recognized and handled before it escalates into a crisis.
As we move forward, let this moment be a reminder that every conversation matters, every screening can be a turning point, and every effort to reduce risky drinking is a step toward a healthier, more resilient society. The collective energy invested in these preventive measures today will pave the way for a future where the risks linked to alcohol consumption are minimized, and individuals can enjoy lives marked by better health, improved relationships, and a stronger sense of well-being.
The task is big, and the issues may feel overwhelming at times, but by working together, staying informed, and using the right counseling tools, we can dive in and address the hidden complexities of alcohol use—one patient, one screening, and one conversation at a time.
Originally Post From https://www.healio.com/news/primary-care/20250805/uspstf-screen-all-adults-for-unhealthy-alcohol-use
Read more about this topic at
Screen and Assess: Use Quick, Effective Methods
Alcohol Screening and Brief Intervention (SBI)