Perspective on Digital Health Data and Patient Consent
In today’s fast-paced digital age, managing both patient health and online data involves navigating a maze of tricky parts and technical details. When patients and healthcare providers interact with digital platforms, whether for scheduling appointments, accessing medical reports, or reading the latest oncology insights, the technology behind the scenes plays a critical role. One such technical element is the use of cookies—a tool that stores and accesses device information for improving user experiences.
Cookies are not merely bits of code; they are gateways that allow websites to understand user preferences and behaviors. With data such as browsing habits or unique IDs being processed, these digital tokens create a bridge between patient privacy and meaningful health data delivery. However, the fine points of cookie consent have sparked a lively debate around transparency and user control in modern healthcare environments.
The question we now face is: How do we balance the super important need for patient privacy with the undeniable benefits of a tailored and responsive digital user experience? This discussion is particularly significant for healthcare websites, where any misstep could lead to a cascade of confusing bits and tangled issues.
Understanding Digital Consent: A Closer Look at Its Functional Pieces
When discussing digital consent, it’s useful to break down the types of cookies and what they do. In essence, not all cookies are created equal. Some are essential, while others aim to enhance your browsing experience by storing your preferences or tracking data for analytical purposes. Here’s a closer look at four main types:
- Functional Cookies: These are always active as they are needed to provide basic services explicitly requested by the user. Without these, even simple tasks, such as logging in or transmitting secure communications, could become nerve-racking.
- Preference Cookies: These store user-specific settings based on prior interactions, making pages more adaptable to individual needs. This approach helps make learning about healthcare information more personalized.
- Statistics Cookies: Employed solely for collecting anonymous statistical data, these cookies allow providers to get into the numbers behind site activity. They help gauge user engagement without compromising individual identity.
- Marketing Cookies: Perhaps the most controversial, these cookies are used to compile user profiles to serve tailored ads or track users for marketing purposes. This method has sparked debate due to its potential for intrusive tracking across different websites.
The table below summarizes the primary functions and importance of each category:
| Type of Cookie | Purpose | Necessity Level |
|---|---|---|
| Functional | Enables specific user-requested services | Always active |
| Preferences | Stores user settings and customization | Important, but optional |
| Statistics | Collects anonymized data for analysis | Useful for improvements |
| Marketing | Tracks user behavior for tailored advertising | Optional and controversial |
This dissection of cookie types illustrates the many layers of processing carried out behind the scenes. For healthcare websites, these details are more than just technical jargon—they are a matter of trust between patients and their trusted medical information sources.
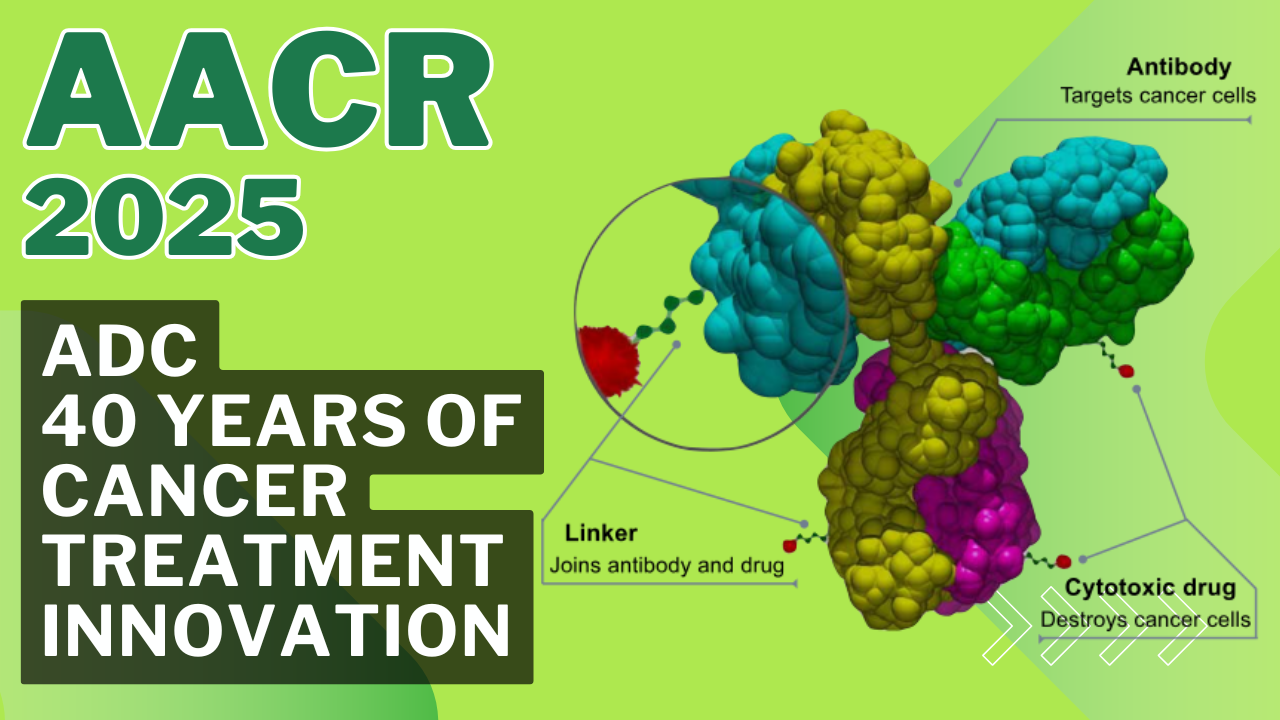
Challenging the Escalation Paradigm in Cancer Treatment
In the realm of contemporary cancer treatment, a familiar debate is rekindled time and time again: Is treating more always the key to better outcomes, or should our focus shift toward better treatment strategies? Recent discussions spearheaded by leading professionals have highlighted that in many cases, adding more drugs or therapies isn’t the answer. Instead, what is needed is a more refined, patient-centered approach that carefully measures treatment’s benefits against its side effects.
A prime example comes from the insights shared by Christina Szalinski in a well-regarded article on Medscape, where the argument was made that over-treatment can lead to life-threatening toxicities and enduring side effects. Renowned oncology experts, including Aleix Prat, have consistently pointed out that while guidelines often prioritize benefit, they sometimes overlook the subtle parts of the patient’s lived experience. This nuanced discussion forces us to re-evaluate how cancer therapy is prescribed and monitored.
Reassessing Treatment Protocols: Why More Isn’t Always Better
Cancer treatment guidelines are based on controlled clinical trial data. While these studies are crucial in the establishment of best practices, they sometimes miss the fine shades of real-world outcomes. In actual clinical settings, patients can face overwhelming side effects that are not fully accounted for by trial protocols. For instance, while a combination regimen that includes immunotherapies might be designated as a top level of evidence, many patients may achieve remission without incurring its risks.
This discrepancy brings forward a key question: How can oncologists make better-informed decisions without solely relying on trial data? One answer lies in developing tools that help estimate the individual patient’s risk of relapse more accurately. When we get into the nitty-gritty of each patient’s case, we understand that a one-size-fits-all approach may lead to overtreatment in situations where it might not be necessary.
Critical to this discussion is the need for transparency. In a fast-evolving medical landscape, effective treatment regimens require not only scientific precision but also clear communication with patients and their families regarding realistic expectations and potential side effects.
Key Considerations for Immunotherapy Approaches
Immunotherapy has emerged as a beacon of hope in oncology, offering patients the promise of harnessing their own immune systems to fight cancer. However, these therapies also come with challenges that need to be carefully managed. The following factors highlight the subtle parts of immunotherapy that practitioners must consider:
- Risk of Autoimmune Reactions: Immunotherapies may inadvertently prompt the immune system to attack not only tumor cells but also healthy tissue, leading to side effects in the thyroid, colon, lungs, and other organs.
- Balancing Efficacy and Safety: While these drugs offer impressive results in many cases, the tricky parts lie in weighing the benefits against the potential for overwhelming or long-lasting toxicities.
- Individual Patient Profiles: The effectiveness and tolerance of immunotherapy vary significantly from one individual to another. Personalized assessments are crucial for determining the best course of action.
- Cost and Accessibility: Beyond the physiological aspects, financial toxicity remains a significant concern. High treatment costs can strain both patients and healthcare systems.
Notably, comments from peers within the oncology community, like those from Miguel Bronchud, have reinforced the view that while controlled trial data provides a solid starting point, the unpredictable twists and turns experienced in everyday practice often tell a different story. It is this real-world complexity that obliges us to share clear and candid information with patients, ensuring that treatment decisions are truly collaborative and patient-focused.
Evaluating the Real-World Implications of Treatment Guidelines
Modern oncology faces the challenge of bridging the gap between controlled clinical environments and the unpredictable nature of everyday patient care. On the one hand, clinical trial data can create a comforting sense of reliability. On the other, they might leave out critical, patient-specific details that play a crucial role in treatment outcomes.
Guidelines often lean heavily on aggregated data, aiming to present the big picture. But as any seasoned clinician can confirm, the little details—the unexpected side effects, the patient’s unique medical history, and even socio-economic variations—can add layers of complexity to every treatment plan. It is these fine shades of information that can transform a well-intentioned treatment protocol into a risky venture if not carefully managed.
Real-life Experiences: The Need for Better Communication and Tailored Treatment
The call for better outcomes in cancer care isn’t just about finding more effective drugs; it’s about interpreting the small distinctions in each patient’s response to treatment. Patients often step into the world of cancer care with a mixture of hope and fear, and it’s the responsibility of healthcare providers to ensure that this journey is navigated with transparency and empathy.
For instance, the discussion around pembrolizumab’s use in early-stage triple-negative breast cancer has ignited debates within the oncology community. While trial data champions its efficacy, real-world cases reveal critical side effects that can have life-altering implications. As oncologists, figuring a path through these tense issues requires not only scientific acumen but also a compassionate understanding of the patient’s overall well-being.
Sharing experiences and expert opinions can help bridge the gap between theoretical benefits and practical, everyday outcomes. The conversation among professionals, echoed through platforms like Medscape and LinkedIn, underpins the need for constant reassessment and reassignment of treatment protocols that meet the evolving needs of patients.
Tools for Estimating Patient Risk: Enhancing Decision-Making
One promising avenue for addressing these challenges is the development and use of advanced tools tailored to predicting patient-specific risks. These digital solutions aim to provide oncologists with nuanced data on relapse probabilities, helping them fine-tune treatment regimens. Some of the key benefits of these tools include:
- Personalized Risk Assessment: By integrating patient history, genetic information, and current health status, these tools offer super important insights that can shape treatment decisions.
- Improved Outcome Predictions: Enhanced algorithms can provide a better estimation of the benefits versus the potential risks, which is key for avoiding unnecessary aggressive treatments.
- Real-Time Data Integration: Modern healthcare platforms can now update risk assessments in real time, ensuring that treatment decisions reflect the most current understanding of the patient’s condition.
- Enhanced Communication: These tools also facilitate clearer conversations between healthcare providers and patients by providing concrete numbers and detailed reports that support clinical decisions.
Integrating these advanced risk assessment tools into everyday clinical practice represents a significant opportunity to mitigate the overwhelming uncertainties that come with high-stakes cancer treatments. Ultimately, these solutions aim to ensure that treatment strategies are tailored meticulously, reducing unreasonable side effects while achieving optimal outcomes.
Managing Digital Health Platforms: A Double-Edged Sword
The digital revolution in healthcare is not limited to treatment innovations alone; it extends to how information is delivered and managed online. For websites and patient portals, the functionality of cookies and similar tracking technologies plays a super important role in ensuring that users receive personalized and timely content. However, this intersection of healthcare and technology also carries its own set of confusing bits and potential pitfalls.
On the one hand, the integration of advanced digital platforms allows patients to schedule appointments, access test results, and obtain the latest research findings with ease. These systems depend heavily on digital consent—not just for compliance with data protection laws, but to build trust with users who are increasingly concerned about how their personal information is used. On the other hand, inadequate transparency around data usage can adversely affect user experience and diminish trust.
Ensuring Transparency in Digital Consent
Healthcare websites must carefully explain the purpose and scope of the data they collect. Transparent communication is not only a legal obligation but also a key component in building lasting relationships with users. The challenge, however, lies in communicating these technical details in a way that is understandable, relatable, and free from overwhelming legalese.
One effective strategy is to compartmentalize the information into clear categories, as demonstrated by the breakdown of cookie types. When users can see what each category of cookie does, they are better equipped to make informed decisions. This process can be further enhanced by using tables, bullet lists, and plain language explanations that steer through the nervous or intimidating aspects of technology use.
For instance, a healthcare provider’s online platform might include a dedicated section that outlines exactly why cookies are used and what each type entails. Such an approach helps reduce uncertainty and allows patients to comfortably manage their digital consent settings while accessing critical healthcare information.
Implementing Patient-Friendly Data Policies
When crafting digital data policies, healthcare providers should keep the following guidelines in mind:
- Clarity: Use plain language and easily digestible sections to explain what data is collected and why it matters.
- User Empowerment: Offer clear instructions on how users can manage or withdraw consent without compromising essential services.
- Transparency: Regularly update policies to reflect current practices and emerging trends in data use.
- Feedback Mechanisms: Incorporate options for users to ask questions or provide feedback about their privacy concerns.
By adhering to these guidelines, digital platforms in healthcare can cultivate an environment where patients feel both secure and well-informed, ensuring that trust remains at the core of patient-provider interactions.
The Intersection of Innovation and Patient Care: Lessons Learned
Both in the realm of cancer treatment and digital data management, a key takeaway is that doing more is not enough. Whether it’s in prescribing new therapies or implementing advanced digital tracking systems, the emphasis must be on refining approaches for better outcomes. This philosophy is echoed in the broader healthcare landscape, where the pursuit of excellence requires balancing technological advancements with genuine human touch.
Modern medicine faces many tricky parts—from understanding the subtle details of treatment side effects to effectively communicating the intended purpose of digital tracking tools. The challenge lies in working through these issues in a way that optimally benefits patients. The cumulative experience over the years tells us that technology and medicine, when combined thoughtfully, hold enormous potential to improve quality of care while also respecting individual privacy and personal health journeys.
Bridging the Gap Between Data and Decision-Making
While clinical trials offer a foundation for treatment decisions, real-world patient care requires an appreciation for the unpredictable twists and turns that occur outside the laboratory. One striking example is the broad debate around treatment protocols that prioritize more drugs over better-targeted therapies. As professionals in the healthcare sphere continue discovering new tools for assessing patient risk and personalizing care, it becomes clear that the true progress lies not just in accumulating more data but in interpreting it with empathy and scientific rigor.
In practical terms, this means integrating digital risk-assessment tools, refining treatment protocols based on real-world evidence, and ensuring that patients have access to accurate, transparent information at every step of their journey. Each of these components, while technical in nature, also carries a significant emotional weight for patients and their families.
Improving cancer care, then, is a call for balance—where technological innovation meets the art of effective communication. It is about making sure that patients are well informed, that side effects are closely monitored, and that treatments are personalized to suit individual needs.
Key Takeaways for Healthcare Providers
- Emphasize Personalized Care: Leverage digital tools to evaluate individual patient risk, enabling more tailored treatment decisions that consider both efficacy and safety.
- Communicate Clearly: Use simple language and structured data presentations (tables, bullet lists) to ensure patients understand both the benefits and the potential risks of treatments and digital data collection practices.
- Promote Transparency: Whether discussing cookie consent or treatment plans, always be forthright about what data is collected, why it is important, and how it will be used.
- Balance Innovation and Empathy: Recognize that technological advancement should go hand-in-hand with empathetic patient care. Share the real-world implications of clinical data so that patients are fully aware of what to expect.
These takeaways underscore the idea that modern healthcare is a blend of art and science—a space where digital innovation can significantly enhance patient outcomes when applied thoughtfully.
Final Thoughts: A Call for Better Treatment and Transparent Digital Practices
The landscape of modern healthcare is evolving rapidly, and with that evolution comes the responsibility to balance scientific progress with genuine patient care. On one hand, digital technologies such as cookies and advanced tracking systems offer exciting opportunities to enhance patient experiences and provide personalized services. On the other, the same technologies require a careful, transparent approach to ensure that patient trust is not compromised.
Similarly, in the clinical realm, the conversation around cancer treatment is undergoing a subtle but important shift. The focus is moving away from merely treating more—with an emphasis on a heavier arsenal of drugs—and toward treating better. This means re-assessing guidelines, incorporating individual patient risks, and ensuring that every treatment decision considers the lived experience of the patient.
As healthcare professionals continue to figure a path through these tangled issues, a common theme emerges: the need for balance. Whether it’s reconciling the benefits of digital tracking with privacy concerns or ensuring that cancer treatments are as safe as they are effective, the goal is to provide care that is both informed and compassionate.
In conclusion, our journey toward improved healthcare is one marked by constant learning and adaptation. Every subtle twist in treatment outcomes, every small detail in digital data management, and every open conversation with a patient contributes to a broader effort to create systems that are truly patient-centric. Only by being clear about the challenges and proactively addressing them can we hope to provide both better treatment and better digital experiences for everyone involved.
Ultimately, this call for enhanced treatment approaches and digital transparency is not about forsaking progress in one area to benefit the other. Rather, it is about integrating the strengths of both domains so that they reinforce each other, leading to a healthcare ecosystem that is both innovative and deeply empathetic.
The road ahead may be filled with confusing bits and overwhelming uncertainties, but as long as we are committed to sharing the right information at the right time, transforming both clinical practice and digital health management will continue to pave the way for improved patient outcomes. In the spirit of collaboration and transparency, healthcare providers, researchers, and digital innovators alike must take the wheel and steer through these challenges together.
By championing both better treatment for cancer patients and ensuring that digital experiences remain trustworthy and user-friendly, we can create a future where technology and medicine, hand in hand, empower us all. The art of healthcare is not solely found in the breakthroughs of the lab or the rapid evolution of digital tools but in the harmonious interplay of knowledge, technology, and the heartfelt commitment to every patient’s journey.
We stand at the crossroads of opportunity: one where embracing the fine details, engaging in clear dialogue, and carefully weighing treatment decisions can lead to breakthrough moments in oncology and beyond. Let us continue to challenge outdated paradigms, refine our digital consent protocols, and, most importantly, deliver care that is as compassionate as it is cutting-edge.
In embracing these principles, we not only honor the trust patients have placed in us but also commit to an ongoing journey of learning, adapting, and ultimately, healing. Our shared goal—ensuring that every patient experiences not just more treatment, but better treatment—is a challenge worth pursuing with all the care and attention it deserves.
Originally Post From https://oncodaily.com/voices/aleix-prat-350386
Read more about this topic at
Rethinking how we deliver care across Canada
Oncology – AstraZeneca – Redefining Cancer Care