Patients Embrace Personalized Ovarian Cancer Treatment: Insights From the VALTIVE Study
In recent years, advancing technology and research have empowered patients with ovarian cancer to take a more active role in their treatment plans. A UK-based study published in BMJ Open, embedded within the VALTIVE1 clinical trial, has sparked an invigorating discussion on patient preferences regarding biomarker testing to guide treatment decisions. This study, which looks closely at the use of the drug bevacizumab in conjunction with chemotherapy, reveals that many women are eager to take part in personalizing their treatment—especially if it means avoiding unnecessary side effects.
The research involved qualitative phone interviews with 11 women undergoing treatment for advanced ovarian cancer. The women shared their experiences with bevacizumab, discussed potential side effects, and offered opinions on continuing or ceasing the use of the drug based on their biomarker test results. Their voices underscore the importance of clear and empathetic communication between healthcare professionals and patients when it comes to making tricky parts of cancer treatment decisions.
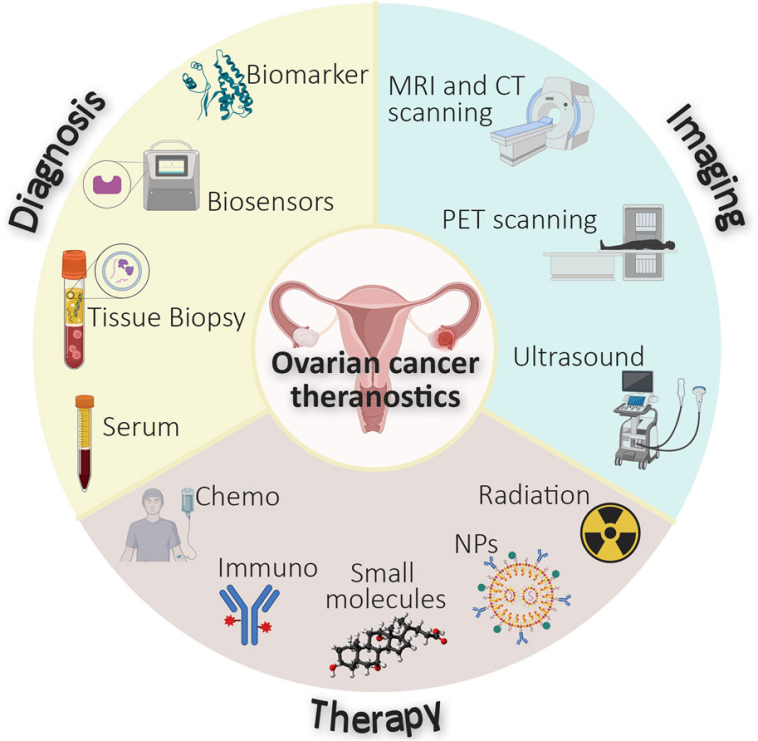
Personalizing Ovarian Cancer Treatments With Biomarker Testing
Biomarker testing is an emerging frontier in cancer care, aiming to tailor treatments to an individual’s unique biological makeup. The VALTIVE1 trial focuses on measuring Tie2—a protein associated with blood vessel growth in tumors—to determine how effectively bevacizumab works for each patient. This method of aligning treatment based on a patient’s biomarker test results represents a major shift away from one-size-fits-all therapy.
Several women in the study reported experiencing alarming side effects such as fatigue, joint stiffness, nosebleeds, and muscle aches when taking bevacizumab, especially during its combination with chemotherapy. Despite these uncomfortable experiences, most participants welcomed the idea of a future trial (VALTIVE2) where treatment could be modified based on precise biomarker results. Patient sentiment was clear: if a drug is unlikely to work, the potential for unnecessary side effects should be avoided.
Long-Term Benefits of Benefit-Driven Biomarker Testing in Ovarian Cancer
One of the long-tail keywords frequently driving discussion in health forums today is “benefit-driven biomarker testing in ovarian cancer treatment.” When patients and oncologists work together to align treatment strategies according to measurable biological signals, the hope is that overall outcomes will improve and the treatment experience will become less nerve-racking.
Here are some key benefits observed from such personalized approaches:
- Reduced Physical Burden: Patients can avoid the overwhelming side effects of drugs that may not be effective for them.
- Targeted Treatment Choices: Biomarker testing can help clinicians figure a path for treatments that are more likely to yield positive outcomes.
- Enhanced Communication: Regular updates about test results and treatment adjustments foster trust and engagement between patients and care teams.
- Increased Patient Empowerment: With access to relevant information and support, patients feel more in control of their journey.
By focusing on these benefits, researchers and clinicians are gradually transforming the landscape of ovarian cancer care into one that is more patient centered and geared toward managing the small distinctions and hidden complexities of individual cases.
Side Effects and Patient Experiences: Managing the Physical Toll
For many patients, the physical toll of treatment is one of the most taxing parts of the journey. In the study, participants reported a variety of side effects from bevacizumab, including tiring fatigue, persistent joint stiffness, spontaneous nosebleeds, and muscle aches. Such uncomfortable experiences highlight the importance of not only finding the right drug but also ensuring that treatments do not introduce new, trickier parts to an already challenging disease experience.
The decision to potentially discontinue a drug like bevacizumab if it proves ineffective, based on biomarker insights, presents a compelling argument for personalized treatment. For many women, the idea of stopping a medication that is causing additional discomfort—in favor of an alternative treatment strategy—resonates deeply. They appreciate having the option to mitigate the physical repercussions attributed to drugs that may not be offering them any benefit.
Balancing Side Effects with Treatment Efficacy in Ovarian Cancer
A detailed exploration of this balance is key to understanding patient expectations and physician responsibilities. When it comes to treatment decisions, the following steps are especially crucial:
- Open Dialogue: Ensuring patients are fully informed about potential side effects and what each drug can and cannot do.
- Regular Monitoring: Implementing frequent check-ins and tests to gauge the effectiveness of the treatment.
- Flexible Treatment Plans: Adjusting or discontinuing treatments based on biomarker test results to limit exposure to negative side effects.
- Patient Support Networks: Creating robust systems that provide emotional and practical support throughout the treatment journey.
These strategies not only help patients manage the physical and psychological toll of treatment but also empower them to participate actively in their healthcare decisions.
Transparent Communication: A Cornerstone in Patient-Centered Care
One repeated theme that emerged from the interviews was the immense value patients place on transparency and regular communication. Women in the VALTIVE1 trial underscored the need to be kept informed about the results of biomarker tests, the effectiveness of their treatments, and any emerging side effects as soon as they come to light.
In a disease as unpredictable as ovarian cancer, clear communication can transform an intimidating treatment experience into one that is manageable and, at times, even hopeful. When patients understand the little details behind their treatment decisions, they are better equipped to face its subsequent twists and turns.
Effective Communication Strategies for Better Cancer Care
Healthcare teams can incorporate several key communication strategies to foster a supportive and empathetic environment:
- Personalized Reporting: Instead of providing generic lab reports, clinicians can offer personalized explanations that break down the fine points of biomarker testing, treatment plans, and expected outcomes.
- Consistent Updates: Regular one-on-one meetings or phone sessions help patients stay up-to-date with their test results and any changes in treatment protocols.
- Accessible Language: Using everyday language rather than dense medical jargon ensures that patients fully understand their treatment journey.
- Emotional Support: Integrating mental health resources so that individuals feel supported both academically in their treatment choices and emotionally throughout the process.
Many experts argue that transparent communication is not merely a courtesy—it is a central component of a patient’s overall well-being. When patients are armed with knowledge and made an active part of the decision-making process, they are more likely to adhere to treatment recommendations and engage fully with every opportunity to improve their quality of life.
Navigating the Tricky Parts: The Role of Bevacizumab in Ovarian Cancer Treatment
Bevacizumab has long been a staple in the treatment of ovarian cancer, particularly when paired with traditional chemotherapy. However, the complexity of its side effects—as experienced by the women in the study—illustrates the challenges in managing this therapeutic approach. Balancing its potential to shrink tumors with its capacity to produce uncomfortable side effects is an ongoing challenge in clinical practice.
For many patients, the appeal of biomarker-based treatment choice lies in the possibility of avoiding the unnecessary toxicity of a drug that may be doing more harm than good. This approach, which hinges on measuring biomarkers like Tie2, is intended to guide decisions about whether to continue or stop the use of bevacizumab during treatment.
Innovative Approaches for Bevacizumab Management in Ovarian Cancer
The experience of patients in the VALTIVE1 trial suggests a broader trend in oncology: the move toward more individualized care plans. A few of the innovative strategies include:
- Real-Time Biomarker Monitoring: Using blood tests that quickly measure key proteins and signals can help determine if the drug is working as desired.
- Tailored Dosing Schedules: Adjusting the dosage of bevacizumab based on the patient’s response as indicated by biomarker data.
- Early Intervention Protocols: Setting up clear benchmarks for when a drug should be adjusted or discontinued ensures that patients experience the least possible negative effects.
- Collaborative Decision-Making: Involving patient input in every step of the treatment plan allows for a more flexible and responsive approach to care.
These approaches not only provide a model for handling the specific case of bevacizumab in ovarian cancer treatment but also set the stage for broader applications in personalized cancer care. Ideally, a future trial like VALTIVE2 will absorb these lessons and optimize treatment protocols that are both pragmatic and tuned to the needs of the patient.
Empowering Patients Through Shared Decision-Making
One of the most compelling outcomes of the study is the strong desire expressed by patients to be fully engaged in the decision-making process regarding their treatment. Rather than being passive recipients of medical interventions, many women voiced the need to actively participate in treatment planning. This aligns with a broader trend in modern medicine: the shift toward shared decision-making.
Shared decision-making means that clinicians and patients collaborate to weigh the risks, benefits, and likely outcomes of different treatment options. In the context of ovarian cancer care, this method is especially important, as it directly addresses the need to manage the side effects and identify the most effective treatment strategies.
Strategies for Enhancing Shared Decision-Making in Oncology
A number of strategies can support a more balanced partnership between patients and their care providers:
- Accessible Information: Educational materials should be provided in plain language, outlining the key aspects of biomarker testing, treatment benefits, and potential risks.
- Decision Aids: Visual aids, checklists, and simple decision trees can help patients evaluate their options without getting overwhelmed by the dense medical data.
- Patient Support Groups: Forums and support communities where patients share their experiences and advice can reinforce the benefits of personalized approaches.
- Feedback Loops: Regularly soliciting feedback from patients regarding their treatment experiences helps clinicians refine their communication and treatment strategies.
The insights shared by the patients in the VALTIVE1 trial underscore that when patients are equipped with the right tools and information, they can work through the tangled issues of ovarian cancer treatment with greater confidence. They are more likely to stick with a treatment plan if they clearly understand its rationale and see immediate relevance to their own health.
Overcoming the Overwhelming Challenges: A Closer Look at Ovarian Cancer
Ovarian cancer remains one of the most challenging and nerve-racking forms of cancer to treat. Often diagnosed in advanced stages, its management involves not only the direct battle against the tumor but also the management of myriad side effects that accompany treatment. The VALTIVE study brings to light both the heroic resilience of the patients and the pressing need for treatments that are finely tuned to their biological profiles.
The idea of eliminating unnecessary treatment—thereby easing the physical and emotional burden on patients—is both appealing and essential. It is crucial for healthcare providers to figure a path through the labyrinth of treatment decisions by integrating patient feedback, biomarker testing, and a flexible approach to drug regimens.
Key Considerations in Addressing the Challenges of Advanced Ovarian Cancer
When tackling ovarian cancer, several key factors must be kept in mind:
| Challenge | Considerations |
|---|---|
| Late Diagnosis | Emphasize early screening and patient education to catch the disease earlier when treatment may be more effective. |
| Side Effect Management | Utilize biomarker testing to adjust therapy and reduce toxic exposure from treatments like bevacizumab and chemotherapy. |
| Emotional Strain | Prioritize ongoing emotional and psychological support through counseling and patient support groups. |
| Lack of Personalized Treatment | Adopt new diagnostic tools such as Tie2 testing to tailor treatment strategies for individual patient profiles. |
Addressing these issues requires a coordinated effort from the entire healthcare team, ensuring that all aspects—from early intervention to emotional support and personalized treatment design—are seamlessly integrated into patient care.
Charting a New Course in Ovarian Cancer Treatment: What the Future Holds
The VALTIVE study represents a promising step in a larger journey toward truly individualized medicine in ovarian cancer care. Looking forward, there is significant enthusiasm around ongoing and future trials like VALTIVE2, which aim to build upon the lessons learned from their predecessors and refine treatment protocols in a way that more effectively manages treatment side effects while prioritizing efficacy.
The future of ovarian cancer treatment lies in several critical areas:
- Integration of New Biomarkers: Continuing research into additional biomarkers that can further refine treatment choices is a promising area of advancement.
- Adaptive Clinical Trials: Designing trials that can quickly incorporate new findings and adjust treatment plans in real time will make for a more dynamic approach to patient care.
- Patient-Centric Research Models: Emphasizing the role of patient feedback in shaping future studies ensures that clinical research addresses the actual needs and priorities of those affected by ovarian cancer.
- Holistic Support Systems: Combining state-of-the-art treatment with comprehensive care strategies—including nutrition, mental health support, and complementary therapies—can significantly enhance quality of life during and after treatment.
This evolving approach in oncology is a testament to how modern medicine can learn from patient experiences to craft more flexible, effective, and supportive care models.
Implementing a Patient-Centric Future in Oncology
For the future, it is crucial to develop an environment where patients and providers work together on equal footing. Some strategies include:
- Establishing Multidisciplinary Teams: Bringing together experts in oncology, genetics, nutrition, and mental health to create integrated treatment plans.
- Leveraging Technology: Utilizing advanced data analytics and digital health tools to monitor patient progress and quickly flag any signs of treatment inefficacy.
- Feedback-Driven Adjustments: Continuously gathering and incorporating patient feedback to refine treatment protocols in real time.
As research continues to dig into the potential of personalized medicine, the hope is that more women will be spared the unnecessary physical and emotional strain wrought by treatments that may do little to improve their outcomes. This is not just a medical challenge—it is a call for a more compassionate and practical approach to healthcare that puts patients at the very heart of every decision.
Patient Stories: The Human Face of Biomarker-Based Decisions
Beyond the quantitative data and clinical outcomes, the human stories behind these advances remind us why personalized care matters so much. For example, one participant in the VALTIVE study shared how her quality of life improved dramatically once she fully understood her treatment options. Once she learned that the biomarker test could indicate whether continuing bevacizumab would be beneficial, she felt empowered to discuss alternative strategies with her physician.
Her story—and those of many other women—underscores the critical reality that individual experiences, while sometimes varied and unpredictable, drive innovation in care. When patients are informed, supported, and actively engaged in decisions about their treatment, the overall journey becomes a shared mission aiming to reduce the nerve-racking and overwhelming uncertainties of battling ovarian cancer.
The Impact of Shared Experiences on Future Treatment Protocols
Patient narratives are not only important for creating empathy but also for influencing future research and clinical practice. Here are some of the ways patient experiences are making a difference:
- Clinical Trial Design: Incorporating patient feedback into trial protocols can help design studies that are both scientifically robust and sensitive to patient needs.
- Treatment Personalization: Understanding the subtle differences in patient responses can lead to more tailored treatment approaches.
- Support Resources: Patient stories often spark the development of support networks and educational programs that address the practical realities of living with cancer.
- Research Priorities: Patient advocacy can help shift research priorities toward studies that are most aligned with improving quality of life.
By continuing to collect and analyze these experiences, the medical community can stay grounded in the day-to-day realities of those living with ovarian cancer. In doing so, they ensure that scientific advances translate into tangible improvements in patient care.
Integrating Nutrition, Fitness, and Holistic Care in Cancer Treatment
While biomarker testing and personalized drug decisions represent the frontier of cancer treatment, a comprehensive approach to care does not neglect lifestyle factors such as nutrition and fitness. Many patients dealing with ovarian cancer also face challenges related to weight management, physical activity, and overall wellbeing. It’s increasingly recognized that a multidisciplinary approach—including holistic care—can play a supportive role in managing the load of treatment side effects.
Recent discussions among healthcare experts call for integrating nutritional guidance and physical activity recommendations into treatment protocols. When patients experience fewer side effects, they are not only more physically robust, but they also develop a proactive mindset toward their overall health.
The Role of Nutrition and Exercise in Reducing Treatment Side Effects
Here are several points outlining why nutrition and fitness are considered essential in a holistic ovarian cancer treatment plan:
- Supporting Immunity: A balanced diet rich in antioxidants and vital nutrients can help boost the immune system during treatment.
- Improving Energy Levels: Regular, moderate exercise can alleviate fatigue—a common side effect of cancer treatments.
- Mental Wellbeing: Physical activity is known to reduce instances of anxiety and depression, contributing to a more positive outlook during difficult times.
- Complementing Medical Treatment: Holistic approaches that include nutritional support can enhance the overall effectiveness of medical therapies.
A combination of advanced biomarkers in clinical trials, along with supportive lifestyle interventions, creates a comprehensive care model where every component—from the smallest twist in treatment strategy to the broad quick fixes in lifestyle—is geared towards improving patient outcomes.
Concluding Thoughts: Toward a More Compassionate Future in Ovarian Cancer Care
The VALTIVE study sheds light on an important narrative: patients with advanced ovarian cancer not only desire but also strongly support treatment plans that are uniquely tailored to their biological and personal needs. As precision medicine continues to evolve, there is hope that these advances herald a future where decisions about cancer treatment are guided both by science and by the lived experiences of patients.
In a field where every decision carries significant weight, it is super important to combine the measurable insights provided by biomarker testing with a caring, open dialogue between patients and their doctors. The ultimate goal is to create treatment paradigms that not only extend survival but also improve the quality of life by minimizing unnecessary side effects.
The path ahead may be filled with tangled issues, nerve-racking uncertainties, and complicated pieces to figure out, but there is a resolute commitment among clinicians and researchers to pilot a course that advocates for personalized, compassionate care. By thoroughly integrating biomarker insights, robust patient communication, and a holistic support system, the medical community is steering through the twists and turns toward a future where the management of ovarian cancer is as tailored as it is effective.
Patients, clinicians, and researchers alike are encouraged to continuously take a closer look at the evolving approaches in treatment, ensuring that decisions are always made with transparency, care, and a deep respect for the patient’s personal journey. As we figure a path through the hidden complexities of ovarian cancer care, the message is loud and clear: every patient deserves the chance to engage in a treatment plan that honors not just their disease status, but their quality of life and overall well-being.
In conclusion, the insights provided by the VALTIVE study are a clarion call for enhanced personalization in ovarian cancer treatment. The discussion points raised—from managing side effects to the intricacies of shared decision-making and holistic care—are not isolated clinical issues but part of a broader patient movement toward choices that are more informed, compassionate, and attuned to individual needs. As the medical community continues to work through the challenging bits of treatment optimization, there is hopeful anticipation that future trials and research will chart a more human-centered approach to combating ovarian cancer.
Ultimately, the integration of biomarker testing and personalized treatment strategies should serve as a model for all areas of oncology. This approach not only respects the myriad subtle details of each patient’s experience but also leverages modern research to create more effective, targeted, and emotionally supportive care regimens. While the journey may at times seem overwhelming and the road ahead riddled with tension, the shared commitment to improving patient outcomes promises a brighter, more empowered future in ovarian cancer care.
Originally Post From https://www.docwirenews.com/post/patients-support-biomarker-based-decisions-in-ovarian-cancer-treatment-trial-study-finds
Read more about this topic at
What Patients Want: Personalized Healthcare Experiences
Personalization in Healthcare: Patient Experience Use Cases