Integrative Medicine in Focus: Rethinking Pain Management in Primary Dysmenorrhea
The growing interest in integrative approaches to healthcare has opened doors to innovative treatments for conditions that have long challenged conventional methods. Primary dysmenorrhea, characterized by menstrual pain without pelvic organic lesions, has been a subject of rigorous clinical research. Complementary interventions, including traditional acupuncture and the relatively newer method of myofascial trigger point dry needling (MTrP-DN), are garnering attention as potential alternatives to standard pharmacologic management.
In this editorial, we dive into a recent three-arm randomized clinical trial that compares the efficacy of MTrP-DN, traditional acupuncture, and sham needling in managing primary dysmenorrhea. Let us take a closer look at the study design, the methods employed, and the implications of its findings, all while unraveling some of the tricky parts of clinical trial design and treatment assessment.
Understanding the Basics: Primary Dysmenorrhea and Current Treatment Limitations
Primary dysmenorrhea affects between 50% and 90% of women, with over half experiencing moderate to severe pain during menstruation. Its symptoms not only include lower abdominal cramps but also extend to nausea, vomiting, fatigue, and even cold extremities. The societal impact is significant, with many patients missing school or work during their menstrual cycle. While non-steroidal anti-inflammatory drugs (NSAIDs) and oral contraceptives provide relief for many, they do not work for everyone and may introduce long-term risks such as cardiovascular side effects.
This situation has led some patients to explore complementary and alternative therapies. Treatments such as acupuncture have shown promising results in systematic reviews and meta-analyses, yet questions about their broader applicability and the long-term attenuation of pain remain. Emerging evidence now suggests that MTrP-DN may also offer a viable route toward alleviating menstrual pain by targeting specific myofascial trigger points related to pain perception.
Innovative Three-Arm Clinical Trial: A Closer Look at the Study Design
The recent trial under discussion adopted a well-designed three-arm, subject-blind, sham-controlled approach. It recruited 150 participants with a clear diagnosis of primary dysmenorrhea who then received treatment based on allocation into one of three groups: MTrP-DN, traditional acupuncture, or sham needling. With a treatment period of three weeks followed by a 12-month follow-up, the study aimed to evaluate both short-term and long-term effects on pain intensity, quality of life, and related physiological markers.
Key Features of the Trial Methodology
Some of the super important aspects of this trial design include:
- Randomization: Subjects were allocated into groups using a central randomization system to minimize selection bias.
- Blinding: Although practitioners could not be blinded due to the nature of the interventions, patients, examiners, data collectors, and statisticians were kept unaware of treatment assignments to prevent subjective influences on the outcomes.
- Sham Control: The inclusion of a sham needling group provided a baseline to assess the true physiological impact of needling therapies, reducing the risk that perceived improvements were solely due to placebo effects.
- Outcome Measures: The primary outcome was the change in pain intensity measured by a Visual Analog Scale. Secondary outcomes included quality of life, NSAID usage, serum inflammatory markers, and uterine blood flow assessments via Doppler ultrasound.
This multifaceted design allowed the researchers to ask a series of important questions: How do the subtle parts of the two needling techniques differ in therapeutic impact? Could the simpler, less training-intensive MTrP-DN offer comparable—or even superior—benefits compared to traditional acupuncture?
Myofascial Trigger Point Dry Needling: A New Frontier in Menstrual Pain Therapy
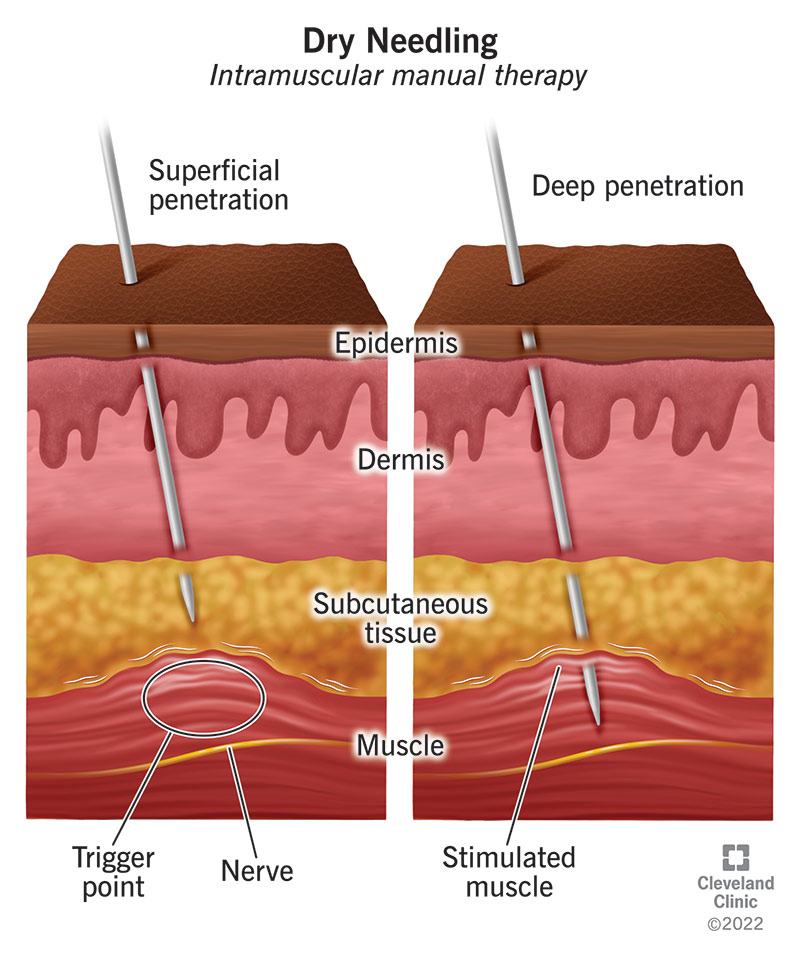
MTrP-DN is drawing increased notice in pain clinics for its targeted approach. Its primary focus is the stimulation of myofascial trigger points, which are often palpable as tense bands or nodules in the muscular tissue. These trigger points are thought to produce local and referred pain that can affect areas away from the point of stimulation, including the uterus. By inserting a needle directly into these points and inducing muscle twitches, practitioners of MTrP-DN aim to interrupt the pain cycle, reduce muscle tension, and improve blood flow.
A Closer Look at the Technique
In the clinical trial, MTrP-DN was administered by pain specialists who followed a standardized protocol. The steps included:
- Identifying trigger points along the lateral edges of the rectus abdominis muscle through palpation, noting the presence of taut bands, local tenderness, and referred pain symptoms that mimicked menstrual cramps.
- Disinfecting the area and using traditional acupuncture needles to provoke local twitch responses, a critical aspect believed to correlate with successful outcomes.
- Executing a needle manipulation technique—moving the needle horizontally in small in-and-out motions—to enhance the deactivation of muscle tension.
This straightforward method does not require extensive training in Traditional Chinese Medicine (TCM), making it an appealing option for more clinicians seeking to offer non-pharmacological solutions.
Traditional Acupuncture Versus Dry Needling: Comparing Clinical Approaches
Traditional acupuncture, based on the principles of TCM, involves the insertion of needles at specific acupuncture points along the body’s energy channels or meridians. This technique relies on restoring balance to the flow of Qi (energy) and is often associated with eliciting the “de qi” sensation—a combination of soreness, numbness, or heaviness that signals adequate stimulation of the point.
Despite the clear overlap between some acupuncture points and myofascial trigger points (with research indicating more than 90% correspondence in some cases), the two techniques differ in their theoretical underpinnings and practical execution. The trial compared the effects of traditional acupuncture on key TCM points against MTrP-DN to see which method might be more effective in managing menstrual pain and improving quality of life.
Contrast in Mechanisms and Training Requirements
While traditional acupuncture demands years of training to master precise point location and needle manipulation techniques based on TCM diagnosis, MTrP-DN is more methodically straightforward. The latter focuses on addressing the painful muscle “nodes” where trigger points reside, making it more accessible for clinicians who may not be certified in TCM.
Both approaches, however, share the concept of modulating the body’s neurophysiological responses to pain. By stimulating certain points, there is a possibility of initiating systemic effects such as reducing the release of inflammatory mediators, improving local blood flow, and ultimately diminishing perceived pain intensity.
Evaluating Long-Term Outcomes: Improving Quality of Life in Dysmenorrhea
A significant highlight of the trial was its comprehensive follow-up period of 12 months. This extended observation period sought to assess not only the immediate reduction in pain intensity but also any enduring changes in quality of life and functionality. The inclusion of standardized questionnaires such as the Short Form Health Survey (SF-36) provided an avenue to measure overall physical and mental well-being.
Key Aspects of Quality of Life Assessment
The study measured several indicators to capture the broad impact of the interventions:
- Physical Component Scores (PCS): These reflected changes in how pain affected daily activities and physical performance.
- Mental Component Scores (MCS): These measured the psychological repercussions of chronic menstrual pain, including anxiety and stress levels.
- Global Rate of Change (GROC) Scale: This scale allowed subjects to subjectively rate their overall improvement, acknowledging the importance of perceived well-being in evaluating treatment success.
By tracking these outcomes, the trial aimed to provide evidence for the super important influence that reduced pain and improved physiological parameters have on life quality. Ultimately, a treatment that can lower NSAID consumption and improve day-to-day function could be considered a major breakthrough in a field often riddled with tension and loaded with treatment challenges.
Addressing the Tricky Parts: Study Limitations and Blinding Challenges
Despite its comprehensive design, the clinical trial is not without its tricky parts. One notable challenge was the inability to fully blind the acupuncturists and pain practitioners conducting the interventions. Practitioners had to be aware of which technique they were administering. However, strong measures were taken to ensure that subjects and data assessors remained unaware of the treatment allocation to minimize any biased influence on outcome assessments.
Handling Blinding and Placebo Effects
Another potential pitfall in studies with subjective outcomes like pain intensity is the placebo effect. To counteract this, the study employed a sham needling group which used specially designed placebo needles that mimic the appearance and to some extent the pressure sensation of real needles without actual skin penetration. This approach was critical in ensuring that any differences in outcomes among the groups represented true therapeutic benefits rather than psychological expectations alone.
The researchers also administered the Treatment Credibility Scale at multiple time points. This allowed them to get into the fine details of how logical the subjects found each treatment and their confidence in its effectiveness. Such measures help figure a path forward in interpreting the results, especially when considering that subtle differences in expectation could influence study outcomes.
Comparative Tables: Summarizing the Study’s Core Elements
The following table summarizes the primary elements of the intervention groups in the study:
| Treatment Group | Technique | Key Features |
|---|---|---|
| MTrP-DN | Needling of myofascial trigger points with the aim to induce local twitch responses |
|
| Traditional Acupuncture | Insertion of needles at TCM acupuncture points based on individual diagnosis |
|
| Sham Needling | Placebo technique using non-penetrating needles at non-acupuncture points |
|
This structured approach not only aids in comparing the different interventions but also highlights the careful planning necessary to address the tangled issues associated with clinical trial blinding and bias management.
Exploring the Underlying Mechanisms: How Needling Techniques May Modulate Pain
Both MTrP-DN and traditional acupuncture may alleviate menstrual pain by modulating neurophysiological pathways. One key theory underlying the benefits of MTrP-DN is somatovisceral convergence, where somatic inputs from muscles and visceral inputs from organs share common neural pathways. For instance, the rectus abdominis muscle and the uterus are innervated by similar lower thoracic spinal nerves, creating a potential for cross-talk between musculoskeletal and visceral pain signals.
By stimulating trigger points in the abdominal muscles, MTrP-DN may reduce local nociceptive input—effectively lowering the overall pain signals transmitted to the spinal cord. This can lead to a higher pain threshold and a decrease in perceived menstrual pain. Traditional acupuncture may operate through a similar mechanism, though it conceptualizes the process in terms of energy flow and balance. Both modalities offer intriguing possibilities for interrupting the pain cycle, albeit from slightly different angles.
Inflammatory Mediators and Uterine Blood Flow
The trial also measured several markers to understand the physiological changes induced by these treatments. Inflammatory markers such as prostaglandin F2α, C-reactive protein (CRP), interleukin-6 (IL-6), and interleukin-8 (IL-8) were assessed. These substances play a significant role in pain modulation and uterine contractions. In conjunction with ultrasound measurements of uterine blood flow indices (such as the systolic/diastolic ratio, pulsatility index, and resistance index), the study sought to provide a detailed picture of how the interventions affect both local tissue conditions and systemic inflammatory responses.
By addressing both the biochemical and blood flow aspects of dysmenorrhea, the research team aimed to get into the nitty-gritty of how needling therapies could help balance physiological parameters critical to managing menstrual pain.
Long-Term Impact: Evaluating Changes in NSAID Use and Overall Well-Being
One of the most compelling reasons to explore alternative therapies for primary dysmenorrhea is the prospect of reducing reliance on NSAIDs. Although these drugs provide short-term relief, their long-term use raises concerns over side effects, particularly cardiovascular issues. The trial carefully tracked the frequency and dosage of NSAID use throughout the treatment period and follow-up intervals.
Reducing medication dependency not only lessens the risk of side effects but can also improve the overall quality of life. Subjects in the trial reported enhanced physical well-being, as measured by the SF-36 survey, and noted improvements in daily activities. For many women, a treatment that effectively decreases pain intensity while simultaneously allowing them to cut back on medication can be transformative.
Benefits of a Multidimensional Outcome Assessment
The study’s multidimensional approach to assessing outcomes offers several benefits:
- Objective Measures: Quantitative assessments such as the Visual Analog Scale (VAS) and Doppler ultrasound provide hard data on pain and uterine blood flow.
- Subjective Assessments: Tools like the Global Rate of Change (GROC) scale capture patients’ perceptions of improvement—a critical factor in understanding treatment impact.
- Quality of Life Metrics: By using instruments like the SF-36, researchers can quantify changes in both physical and mental components of health, which are key determinants of long-term outcomes.
This blend of objective and subjective endpoints is super important when evaluating therapies for conditions that are both physically and emotionally overwhelming.
Taking the Wheel: Implementing Integrative Approaches in Clinical Practice
As more evidence emerges from well-designed clinical trials like this one, practitioners are better positioned to offer integrative treatment options for primary dysmenorrhea. Yet, as with any innovative approach, there are several practical aspects to consider before translating research findings into widespread clinical practice.
Training and Standardization Issues
One of the appealing features of MTrP-DN is its relative ease of adoption compared to traditional acupuncture, which requires long-term specialized training. However, the implementation of either technique in “real-world” settings requires rigorous standardization to ensure that treatments are delivered consistently. This entails:
- Establishing detailed treatment protocols that cover everything from patient selection to needle manipulation techniques.
- Providing centralized training sessions to ensure that all practitioners are familiar with the protocol’s small distinctions and subtle parts.
- Maintaining high standards of data reporting and monitoring to track both effectiveness and safety outcomes.
Creating such standardized protocols can help steer through the tangled issues related to varied treatment execution and ensure the reproducibility of positive results across different settings.
Patient Education and Expectation Management
For integrative therapies to gain acceptance, it is essential to manage patient expectations. Educating patients on what constitutes a successful intervention—including understanding that some discomfort might accompany the treatment process—can help set realistic goals. Clinicians should be clear that while both MTrP-DN and acupuncture are promising, they may not completely eliminate pain for every individual. Instead, they may be instrumental in reducing NSAID usage, improving quality of life, and providing a more natural path to wellness.
Effective communication is also crucial when explaining the concepts of placebo effects, the role of blinding in clinical trials, and the significance of the observed improvements. By transparently discussing these topics, clinicians can foster a trusting relationship that encourages patients to actively participate in their treatment plans.
Walking Away from the Old Guard: The Promise and Limitations of Complementary Therapies
Every treatment method comes with its set of challenges, and no clinical trial is without limitations. In this case, a few key issues stand out:
- Blinding Challenges: As noted, only the subjects and outcome assessors were blinded, while practitioners inevitably knew which technique they were applying. This could potentially introduce bias in treatment delivery.
- Single Session Design: The trial’s design of a single session consisting of three weekly treatments may not capture the full range of therapeutic benefits or risks over time. Future research could explore multi-session interventions to address this.
- Placebo Considerations: While the sham needling control was designed to mimic a treatment experience, it is not entirely inert. This means that some groups might experience a pressure sensation that could itself have a therapeutic effect.
Appreciating these tricky parts and complicated pieces of trial design is essential. It reminds us that, while promising, the field of complementary therapies is still evolving, and researchers must remain vigilant in refining study protocols and broadening inclusion criteria to capture the full spectrum of patient experiences.
Future Implications: Integrative Treatments and the Path Forward
The results from this well-constructed clinical trial hold significant promise for the future of primary dysmenorrhea management. If MTrP-DN proves to be as effective—or possibly more effective—than traditional acupuncture for reducing menstrual pain and related symptoms, it could become a key tool in the integrative medicine arsenal.
Practitioners may soon find themselves managing their way through a landscape where alternative therapies are not only supplementary but could also serve as primary interventions for conditions that are otherwise loaded with problems. The potential benefits extend beyond just pain relief; improved quality of life and reduced medicinal side effects stand to make a considerable impact on the overall well-being of those affected by dysmenorrhea.
Key Takeaways for Clinicians
For those in the healthcare field considering the integration of these techniques into practice, here are a few must-have points to keep in mind:
- Adopt a Holistic Approach: Combine objective assessments, such as ultrasound measurements and inflammation markers, with patient-reported outcomes to build a comprehensive picture of treatment impacts.
- Standardize Protocols: Rigorous training and adherence to well-defined treatment protocols are essential to overcome the nerve-racking twists and turns of clinical practice.
- Evaluate Both Short- and Long-Term Outcomes: Consider not just immediate pain relief but also improvements in daily functionality and reductions in NSAID dependency over time.
- Educate Patients: Take a closer look at simple yet clear communication methods that help patients understand the rationale, potential benefits, and limitations of each treatment option.
By keeping these key points in mind, clinicians can better figure a path through the tangled issues of treatment efficacy and patient satisfaction. In doing so, they will help advance the field of integrative medicine and offer relief to those who have long suffered from primary dysmenorrhea.
Conclusion: Embracing a Future of Integrative Pain Management
Primary dysmenorrhea is a condition that has long been associated with significant personal and societal burdens. The evolving landscape of integrative medicine offers much-needed alternatives to conventional therapies, promising fewer side effects and a more natural route to pain relief. Recent research comparing MTrP-DN with traditional acupuncture and sham needling not only highlights the potential of these innovative techniques but also emphasizes the importance of rigorous, well-designed clinical trials in guiding treatment decisions.
Though there are several tricky parts inherent in managing such studies—from blinding challenges to ensuring consistent outcome measures—the insights gleaned pave the way for refining treatment protocols and enhancing patient care. By diving into the fine points and subtle details of needling therapies, the study provides a robust framework for understanding how these approaches can complement conventional methods.
Ultimately, embracing integrative techniques like MTrP-DN could lead to a significant shift in how primary dysmenorrhea is managed. As more clinicians learn to steer through the confusing bits and tangled issues of traditional treatment options, they will be better equipped to offer interventions that are both effective and accessible. The future of pain management in dysmenorrhea may well lie in the balanced combination of time-tested practices and innovative therapeutic strategies—a promising prospect that calls for ongoing research, collaboration, and patient education.
The trial stands as a testament to the potential of integrative medical practices to address not just the physical manifestations of disease but also the broader aspects of patient well-being. As we work through the ever-evolving twists and turns of medical research, the importance of evidence-based approaches cannot be overstated. New research directions, enhanced training protocols, and improved patient communication will be crucial in making integrative pain management a reality for countless women worldwide.
In summary, while challenges remain, the path toward improved management of primary dysmenorrhea through complementary therapies is becoming increasingly clear. With sound research design, detailed outcome assessments, and the relentless pursuit of better patient care, integrative treatments such as MTrP-DN and traditional acupuncture could soon occupy a central role in the therapeutic landscape. This evolution represents a hopeful step forward for patients and clinicians alike, promising a future where pain is managed more naturally, effectively, and sustainably.
Originally Post From https://www.dovepress.com/efficacy-of-myofascial-trigger-point-dry-needling-in-treatment-of-prim-peer-reviewed-fulltext-article-JPR
Read more about this topic at
The efficacy and safety of simple-needling for the treatment …
Effectiveness of dry needling of rectus abdominis trigger …