New Hope in Acute Myeloid Leukemia Treatment: A Look at Ziftomenib with 7+3 Chemotherapy
The emergence of ziftomenib in combination with the classic 7+3 chemotherapy regimen has captured the attention of the medical community. Recent data from the phase 1a/b KOMET-007 trial have shown an impressive 94% objective response rate for patients with newly diagnosed acute myeloid leukemia (AML) harboring NPM1 mutations or KMT2A rearrangements. In this opinion editorial, we aim to take a closer look at the trial results, examine the promising safety profile, and discuss what these early findings might mean for the future of AML treatment.
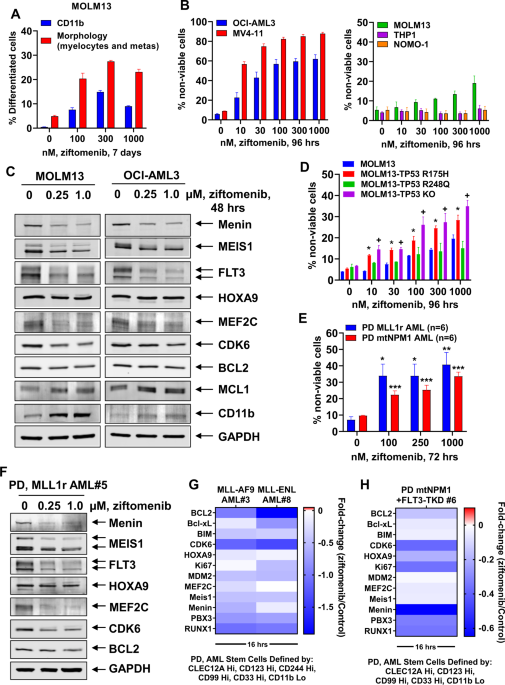
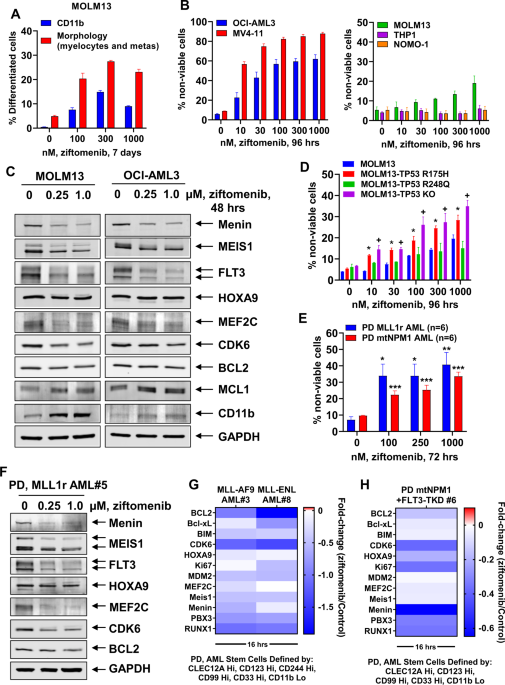
For many patients and practitioners, the journey through the tricky parts and tangled issues of AML therapy is marked by overwhelming uncertainties and nerve-racking decision-making. The introduction of ziftomenib—an innovative, highly selective, oral menin inhibitor—along with the well-established cytarabine and daunorubicin 7+3 induction regimen, has the potential to simplify some of the confusing bits of treatment management and improve outcomes dramatically.
Early Promising Response Rates: What Do the Numbers Tell Us?
The updated data from the KOMET-007 trial presented at the 2025 Society of Hematologic Oncology Annual Meeting reveals several key metrics that are cause for optimism. The trial reported a 94% objective response rate (ORR) when ziftomenib was added at 600 mg once daily to the standard 7+3 regimen. This dramatic figure includes a breakdown of 84% ORR in patients with NPM1 mutations and 74% in those with KMT2A rearrangements. Such high response rates provide a strong rationale for further exploration in phase 3 trials.
It is important for the community to consider not only the high ORR but also the depth of response achieved by patients. Many patients demonstrated deep clinical responses and achieved minimal residual disease (MRD) negativity, aspects that are critical for long-term remission and survival. When we dive into this data, it suggests that ziftomenib can potentially push many patients into a state of remission that was once thought to be elusive.
Detailed Breakdown of Response Metrics
By organizing the data into tables and bullet lists, we can better understand the major clinical outcomes:
| Parameter | Overall Data | NPM1-Mutated AML | KMT2A-Rearranged AML |
|---|---|---|---|
| Objective Response Rate (ORR) | 94% | 84% | 74% |
| Complete Remission (CR) and Related Responses | Majority achieved deep responses including CR, CR with partial hematologic recovery, and CR with incomplete hematologic recovery. | Data reflective of a robust response leading to durable remissions. | Similar trends with potential differences due to underlying disease biology. |
| MRD Negativity | CR MRD negativity achieved in 76%; CRc MRD negativity achieved in 73% | Median time to CR MRD negativity of about 4.5 weeks. | Comparable findings with slightly variable time frames for achieving MRD negativity. |
These results are not only encouraging from a statistical standpoint but may also represent a significant shift in how we approach front-line therapy in AML, especially among patients with these genetic characteristics.
Understanding the 7+3 Chemotherapy Regimen and Its Role
The journey through treating AML is full of complicated pieces, twists, and turns. The 7+3 chemotherapy regimen, which involves the administration of cytarabine for seven days and daunorubicin for three days, has long been a cornerstone in the treatment of AML. However, its application in the context of a novel targeted therapy like ziftomenib brings fresh hope for improved outcomes.
This combination is designed to maximize tumor kill while managing the tricky parts related to adverse effects. By introducing ziftomenib into the mix, researchers are aiming to harness the power of targeted inhibition of the menin protein, which plays a key role in sustaining the malignant state in NPM1-mutated and KMT2A-rearranged leukemias. The synergy of targeted therapy with intensive chemotherapy might well amplify the chances of achieving deep responses while keeping the burden of side effects manageable.
Key Elements of the 7+3 Regimen
- Cytarabine: A nucleoside analog that interferes with DNA synthesis, thereby killing rapidly dividing cells.
- Daunorubicin: An anthracycline antibiotic that intercalates into DNA and disrupts topoisomerase II activity, leading to apoptosis.
- Combination Benefits: The regimen’s success lies in its ability to impair leukemic cells from multiple angles, a vital approach that becomes even more promising when combined with targeted menin inhibition.
This standard of care, when paired with the novel oral inhibitor, demonstrates that modern oncology is not simply about adding new drugs, but about smartly combining therapies to dodge the tricky parts and complicated pieces that have made AML so challenging to treat in the past.
Clinical Safety and Manageable Adverse Effects
No new treatment strategy is complete without an in-depth look into its safety profile. The beauty of the KOMET-007 trial is not just in its high efficacy numbers but also in the manageable safety signals that were observed. Patients did experience some adverse effects, including febrile neutropenia (15%), decreased platelet count (15%), anemia (11%), and decreased neutrophil count (11%). Despite these adverse events, the safety profile aligned with what clinicians expect from intensive chemotherapy regimens.
There were instances of grade 3 adverse effects, including one notable case of differentiation syndrome in a patient with KMT2A-rearranged AML and two cases of grade 3 corrected QT prolongation. However, these events were managed effectively, suggesting that while the treatment comes with certain challenges, they are not insurmountable with proper clinical oversight.
Insights into the Safety Data
To get into the nitty-gritty of the safety data, consider the following summary:
- Febrile Neutropenia: Occurred in approximately 15% of patients. This side effect, though nerve-racking, was anticipated and managed with appropriate supportive care.
- Decreased Platelet Count and Anemia: Each noted in about 15% and 11% of patients, respectively. These effects are common in intensive chemotherapy and underscore the importance of close monitoring.
- Rare Cardiac Events: Two cases of grade 3 QT prolongation have led clinicians to keep a watchful eye on cardiac function with ongoing therapy.
The overall consensus among experts is that the benefits of this novel combination outweigh the risks. The data not only affirm the safety but also highlight the potential for this approach to manage AML effectively while addressing the more intimidating aspects of adverse events.
Patient Selection and Early Data from the KOMET-007 Trial
One of the keys to understanding the promise of this treatment lies in examining the patient demographics and baseline characteristics of the KOMET-007 trial. The study included adults aged 18 to 71, with a median age of 56. Nearly all patients had an ECOG performance status (PS) of 0 to 1, indicating that the trial largely involved individuals who were in relatively good health despite their diagnosis. This factor is critical when considering the intensity of both the standard chemotherapy regimen and the new targeted therapy.
The inclusion criteria were specific, ensuring patients had either a confirmed NPM1 mutation or KMT2A rearrangement. Co-mutations, such as FLT3 and IDH1/2, were also reported in a proportion of the patients, adding layers of complexity to the treatment decisions but also validating the regimen’s effectiveness across a diverse genetic landscape. In this context, the trial is a prime example of precision medicine in oncology—a strategy that matches targeted therapies to the specific genetic makeup of the disease.
Key Points on Patient Baseline Characteristics
- Age Range: 18-71 years, with a median age of 56 years.
- Performance Status: 90% of patients had an ECOG PS of 0-1, demonstrating that most were able to tolerate intensive therapies.
- Co-mutations: Presence of FLT3 and IDH1/2 mutations in 13% and 18% of patients, respectively.
- Treatment Setting: Both newly diagnosed and relapsed/refractory cases were included in different arms of the study.
The careful selection of patients ensures that the findings of the trial are both robust and applicable to a real-world setting. As more data are integrated, clinicians can better figure a path through patient selection criteria that maximize benefit while minimizing the risk of adverse outcomes.
Deep Clinical Responses and the Importance of Minimal Residual Disease
The ability to achieve deep responses in AML is a challenging goal that has significant implications for the prognosis of patients. The high levels of complete remission observed in the trial, along with the impressive rates of minimal residual disease (MRD) negativity—76% for CR MRD and 73% for CRc MRD—illustrate the potential of the ziftomenib combination to not only debulk the disease but also to maintain a state of molecular remission.
MRD negativity is one of those small distinctions that can make a big difference in long-term outcomes, offering a marker of successful treatment. The median time to achieve MRD negativity was around 4.3 to 4.5 weeks, which is relatively quick and indicates that the therapy effectively eliminates residual leukemic cells early in the treatment course.
The Role of MRD as a Prognostic Indicator
Understanding and tracking MRD is critical for predicting long-term outcomes. Here are some vital aspects of its importance:
- Early Clearance: Rapid achievement of MRD negativity offers hope for prolonged remission and potentially lower relapse rates.
- Improved Survival: Patients who achieve MRD negativity often experience longer durations of complete remission and overall survival.
- Therapeutic Adjustments: MRD can serve as an early indicator for adjusting treatment courses, ensuring that therapy remains appropriately aggressive or is de-escalated as necessary.
By achieving MRD negativity in most patients, the data from the KOMET-007 trial reveal a promising new method for working through the technical challenges of AML treatment. It suggests that not only is the leukemia being addressed by intensive chemotherapy, but the addition of ziftomenib is also pushing the cancer deeper into remission by reducing the hidden complexities that often lead to relapse.
Unpacking the Study Design: Insights from KOMET-007
The KOMET-007 trial is structured to answer several key questions regarding dosing, efficacy, and safety. The trial is divided into two parts: a phase 1a dose-escalation portion and a phase 1b dose-expansion phase. This layered approach allows researchers to first pinpoint the optimal dosing level—identified as 600 mg for ziftomenib—and then further explore its efficacy in combination with different chemotherapy backbones, including the standard 7+3 regimen, venetoclax/azacitidine, and venetoclax monotherapy in varied patient populations.
By maintaining such a comprehensive study design, the trial addresses the multiple twists and turns that clinicians face when introducing new therapies into established treatment paradigms. This design helps to figure a path through not only efficacy challenges but also the management of potential side effects.
Overview of the Trial Design
- Phase 1a (Dose-Escalation): In this portion, four different doses (100 mg, 200 mg, 400 mg, and 600 mg) were explored alongside the 7+3 regimen. The recommended dose was set at 600 mg after evaluating the safety and tolerability profiles.
- Phase 1b (Dose-Expansion): At the established dose of 600 mg, the safety profile was further examined with broader patient cohorts, focusing on efficacy endpoints such as complete remission and overall response.
- Primary and Secondary Endpoints: The trial focused on safety, dose-limiting toxicities in phase 1a, along with composite complete remission (CRc), overall survival (OS), and duration of response (DOR) as key secondary endpoints in phase 1b.
This layered approach illustrates how clinical trials in oncology are evolving to address the nerve-racking life-and-death decisions made every day in the treatment of AML. By carefully testing different dosing strategies and combination approaches, studies like KOMET-007 pave the way for more streamlined, effective, and safer therapies.
Managing Your Way Through Safety Concerns and Clinical Challenges
Whenever new treatment strategies are introduced, concerns over safety and tolerability naturally arise. However, it is reassuring that the safety signals observed in the KOMET-007 trial are largely in line with historical data for intensive chemotherapy. The manageable adverse effects help to ease the intimidating aspects of adding a novel agent to a tried and true regimen.
The challenge for clinicians now lies in steering through the overlapping issues of toxicity management while preserving the dose intensity necessary for effective AML eradication. This calls for a balanced approach that weighs the slight differences in side effect profiles against the substantial benefit of high response rates and early MRD negativity.
Strategies for Managing Side Effects
- Close Monitoring: Regular monitoring of blood counts and cardiac function, especially given the reports of febrile neutropenia and QT prolongation, is critical.
- Supportive Care: Implementing supportive measures such as growth factor support, transfusions, and antibiotics can help manage the side effects that come with intensive chemotherapy.
- Patient Education: Educating patients about the potential side effects and the expected course of treatment helps them feel more secure and decreases anxiety related to the treatment process.
- Risk-Benefit Analysis: Continuous assessment of the risk versus the benefit is key. In many cases, the high response rates and deep remission achieved may offset the potential for these manageable adverse effects.
These tactics exemplify how clinicians can find their path through the nerve-racking elements of intensive oncological treatment, ensuring that patient care remains both effective and holistic.
Looking Ahead: Implications for Future Phase 3 Trials
With the promising results of the KOMET-007 trial, many experts are optimistic about the advancement of ziftomenib into phase 3 testing. The upcoming phase 3 KOMET-0117 trial (NCT07007312) will be critical for confirming these early findings in a larger, more diverse patient population.
The move to phase 3 trials is a natural next step as the data support the novel combination not only as safe and tolerable but as highly effective in eliciting deep clinical responses. Moving forward, research will need to address lingering questions such as:
- How do these response rates translate into long-term overall survival and quality of life?
- Will the timing and achievement of MRD negativity continue to serve as a reliable predictive marker for durable remission?
- How can clinicians best figure a path through patient-specific factors such as age, co-mutations, and performance status to tailor therapy in real-world settings?
- What additional supportive care measures might further mitigate the manageable yet challenging side effects seen in these early trials?
These are questions that researchers, clinicians, and patients alike will be watching closely as further studies unfold. The answers may well guide us through the confusing bits of clinical decision-making and lead to a more nuanced understanding of AML treatment in the era of precision medicine.
The Future of Menin Inhibitors in AML Treatment
Menin inhibitors like ziftomenib represent an exciting frontier in the fight against AML. By targeting a protein central to the pathogenesis of NPM1-mutated and KMT2A-rearranged leukemias, these agents are changing the way we think about and manage the disease. While the journey is full of tangled issues and overwhelming challenges, the data so far suggest that menin inhibition might be a critical tool in overcoming some of the hidden complexities in AML therapy.
As with any new class of drugs, the integration of menin inhibitors into standard practice will require careful evaluation, monitoring, and adaptation. Yet the potential for this innovative approach to result in deeper responses and improved survival outcomes is both exciting and promising. In many ways, this could mark the beginning of a new era in targeted cancer therapy—one that truly addresses the fine points of disease biology with precision and care.
Potential Advantages of Menin Inhibition
- Enhanced Efficacy: The combination with 7+3 chemotherapy has shown that high response rates can be achieved in patients who historically have had limited treatment options.
- Rapid Achievements of MRD Negativity: Early clearance of residual disease may be predictive of longer remissions and improved survival prospects.
- Manageable Safety Profile: Despite the challenges associated with cytotoxic chemotherapy, combining these agents with targeted inhibitors can result in an acceptable safety profile that allows patients to tolerate the treatment.
- Precision in Targeting Disease: When therapy is personalized to the genetic makeup of the leukemia, the potential for improved clinical outcomes increases substantially.
These advantages underscore why ziftomenib and similar agents are generating such buzz—not just among researchers but also in clinical settings where every successful treatment option adds a new chapter to the evolving story of AML care.
Balancing Optimism and Caution in the Oncologic Landscape
While the data emerging from the KOMET-007 trial are promising, it is important to approach these findings with balanced optimism. The success of ziftomenib in early-phase trials must be validated by larger, randomized controlled studies to ensure that the observed benefits are both reproducible and durable over the long term.
This balanced view is especially important given the inherently nerve-racking nature of introducing any new treatment in oncology. For patients and caregivers alike, the idea of stepping into uncharted territory with novel agents can be intimidating. The clinical community must continue to work together to provide clear, transparent communication and robust data so that these new approaches can be integrated safely into existing treatment paradigms.
Points of Caution and Consideration
- Long-Term Outcomes: While early responses are promising, data on overall survival and quality of life over an extended period remain to be seen.
- Managing Side Effects: Even with manageable side effects, the overlapping issues related to intensive chemotherapy must be continually addressed through vigilant monitoring and supportive care.
- Patient Selection: As we work through the fine shades of patient eligibility and genetic factors, individualized treatment planning will be essential to maximize benefit while reducing unnecessary risk.
- Cost and Accessibility: Novel agents often bring up discussions about cost-effectiveness in broader healthcare systems, a practical challenge that must eventually be worked through.
By keeping these points in mind, clinicians and patients can move ahead with cautious hope—a mindset that is both realistic and forward-looking in a field where every small victory is celebrated as a step towards conquering a once overwhelming disease.
Final Thoughts: A New Chapter in AML Treatment?
The early promise shown by ziftomenib combined with 7+3 chemotherapy invites both enthusiasm and careful scrutiny from the oncology community. The impressive objective response rates and rapid MRD negativity signal that we may be on the brink of a significant breakthrough in the treatment of NPM1-mutated and KMT2A-rearranged AML. However, as with any new development in medicine, it is essential to figure a path through the complexities, the little twists, and the challenging side effects that come with novel treatment options.
As we continue to digest these results, the overall sentiment is one of cautious optimism. The potential for this therapy to redefine how we manage AML and to provide patients with a real chance at long-term remission is super important. With further trials—from phase 3 studies to long-term observational data—we will eventually gain the clarity required to steer through this exciting yet demanding landscape.
Key Takeaways for Clinicians and Patients
- High Efficacy: The combination of ziftomenib with a standard 7+3 regimen has yielded a remarkable 94% ORR overall, with notable deep clinical responses.
- Manageable Safety Profile: Although side effects such as febrile neutropenia and cardiac events were observed, they are largely manageable with current supportive care practices.
- Rapid MRD Negativity: Achieving MRD negativity in a median of 4.5 weeks signifies the potential for lasting deep responses.
- Future Prospects: The promise of this regimen, supported by robust early data, underlines the need for expanded phase 3 studies to confirm long-term benefits.
In conclusion, the evolution of new targeted therapies like ziftomenib represents a meaningful advancement in AML treatment—one that offers a beacon of hope for patients facing a daunting diagnosis. As the data mature and larger studies unfold, we stand at the cusp of what may become a new standard in managing one of the most challenging hematologic malignancies.
While the road ahead is still full of problems and key decision points, this breakthrough serves as a testament to the power of innovative combinations in modern oncology. The journey is far from over, but with each incremental step, we inch closer to unlocking improved survival and quality of life for patients battling AML.
Looking Forward: Integrating New Data into Everyday Practice
As we poke around the emerging data and take a closer look at the evolution of AML therapy strategies, the key is to continuously integrate new insights into everyday clinical practice. The experience of early-phase trials such as KOMET-007 not only informs us about the potential of novel combinations but also helps refine and optimize patient management protocols.
In practice, clinicians will need to work through the fine points of patient selection, monitoring, and managing the side effects that naturally come with intensive therapy. The promise of ziftomenib lies in its ability to complement established chemotherapeutic regimens and push the boundaries of what is medically achievable in AML care. By embracing a collaborative, evidence-driven approach, we can gradually find our way through the challenging bits and build a future in which even the most complicated pieces of AML treatment are tackled with confidence and precision.
Steps for Integrating New Therapies
- Regular Training and Updates: Clinicians must remain up-to-date with the latest clinical trial results and guidelines to adapt their practice strategies effectively.
- Multidisciplinary Collaboration: Involving oncologists, hematologists, pharmacists, and supportive care teams ensures that each patient gets tailored, holistic care.
- Patient-Centric Decision Making: Utilizing clear, jargon-free communication helps patients understand the benefits and risks, equipping them to be active participants in their treatment journey.
- Real-World Data Monitoring: Beyond the clinical trial setting, collecting and analyzing real-world data will be essential in verifying the long-term impact of these new therapies.
Integrating these strategies will be a dynamic process, one that requires balancing the excitement about potential breakthroughs with the discipline of rigorous clinical validation. As we work through the various layers of data, the ultimate goal remains clear: to improve patient outcomes and make formidable progress in the fight against AML.
A Collaborative Future for Oncology Research
The progress achieved by the KOMET-007 trial is a vivid reminder of how far we have come in the field of oncology. It represents not just a breakthrough in treatment options, but also a collaborative triumph—where researchers, clinicians, and patients alike contribute to a shared vision of precision medicine. Every new insight helps us sort out the confusing bits of treatment planning and builds on the collective knowledge required to transform daunting challenges into manageable tasks.
The next few years promise to be pivotal as larger trials expand our understanding of these promising regimens. The interplay between targeted therapy and conventional chemotherapy is creating a dynamic environment where innovation meets clinical rigor. This partnership between new scientific discoveries and time-tested treatment modalities is exactly what we need to drive oncology forward.
Opportunities for Future Collaboration
- Cross-Institutional Trials: Pooling data from various centers can help validate early findings and ensure that the benefits of new therapies are available to a broader patient population.
- Patient Advocacy and Education: Increasing awareness and understanding among patients about emerging treatments can empower them to actively participate in decision-making processes.
- Technology Integration: Leveraging advances in digital health and data analytics can accelerate the refinement of treatment protocols, ensuring that real-time data informs everyday practice.
By harnessing the power of collaborative research and interdisciplinary teamwork, the oncology community can continue to chip away at the tangled issues and confusing bits that have long defined AML treatment. This integrated approach is not only essential for scientific progress but also serves as a beacon of hope for patients everywhere.
Conclusion: A Transformative Step Forward in AML Management
In summary, the early-phase KOMET-007 trial highlights an exciting new chapter in the treatment of acute myeloid leukemia. The combination of ziftomenib with the established 7+3 chemotherapy regimen has demonstrated impressive response rates, rapid MRD negativity, and a manageable safety profile—even amidst the nerve-racking challenges that typify intensive cancer therapy. While there remain many small distinctions and unresolved questions to explore, the data signal that we are making significant progress in addressing both the biological and practical aspects of AML treatment.
For clinicians, patients, and caregivers alike, these findings offer a glimpse into a future where the barriers of complicated pieces and tangled issues in AML management might be effectively overcome. The journey will undoubtedly continue to present challenges, but with each new study, each carefully managed adverse event, and every robust response, we come one step closer to establishing a new standard of care in oncology.
Ultimately, the evolution of treatments such as this represents a critical moment in modern medicine—a transformative step toward therapies that are as precise as they are potent, as manageable as they are effective. It is a reminder that while the road ahead is loaded with issues, the combined efforts of researchers and clinicians can drive us forward into an era where the confusion of today gives way to the clarity of tomorrow.
Originally Post From https://www.onclive.com/view/ziftomenib-with-7-3-shows-early-promise-in-newly-diagnosed-npm1-mutated-kmt2a-rearranged-aml
Read more about this topic at
10 Acute Myeloid Leukemia Drugs to Watch Out
Study Highlights Promising New Treatment Option for …