Introduction: Supplement-Drug Interactions in Older Adults – An Overlooked Challenge
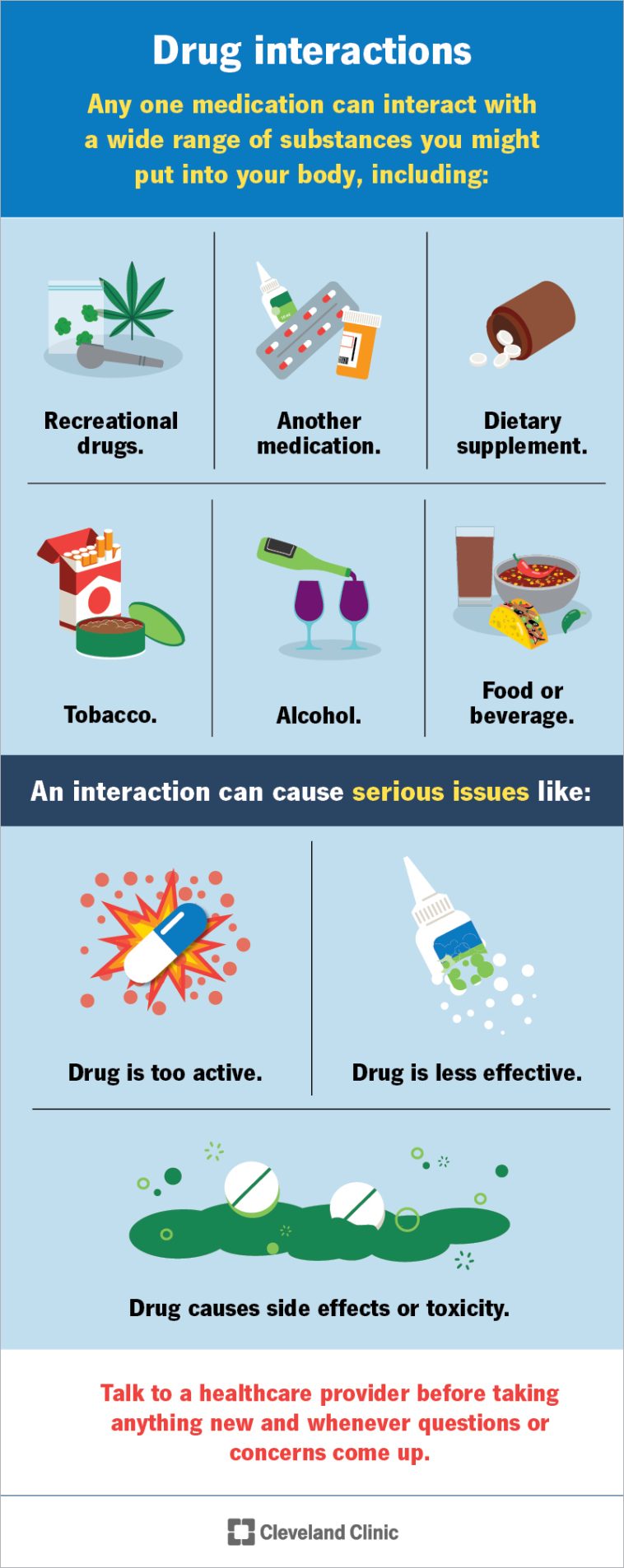
The aging population is booming, and with it comes an increasing number of older adults who mix prescription medications with dietary supplements. This op-ed takes a closer look at the tangled issues of supplement-drug interactions in senior patients. While many in our society perceive nutritional supplements as natural and therefore safe, the hidden complexities of combining them with prescription drugs can lead to unexpected and sometimes dangerous outcomes. In this piece, we will dive in to explore the key findings, review the risk factors, and suggest proactive strategies that can help healthcare providers and patients alike.
There exists a paradox in modern medicine: as the number of older adults increases, so does the phenomenon of polypharmacy – many patients taking five, six, or more medications at a time. In an effort to boost their overall health or manage minor conditions, many seniors also add dietary supplements to their regimen. However, the interaction between these supplements and prescription drugs is not always straightforward, and often the communication between patients and their healthcare professionals is less than ideal. By examining this topic from multiple angles, we hope to shed light on both the potential risks and the actionable strategies necessary for ensuring medication safety.
Rising Trends: The Growing Use of Nutritional Supplements in Senior Patients
Recent studies indicate that between 23% and 82.5% of older adults use dietary supplements alongside their prescription medications. It seems that with increasing age, many patients are on a mission to add what they perceive as “natural” remedies to their everyday routine. With factors such as chronic illness, malnutrition, and the overall burden of multiple medications in play, it is no wonder that many seniors are leaning toward complementary methods to manage their health.
Studies conducted in various regions—including the United States, Europe, and Asia—consistently show that older adults, particularly those with cardiovascular diseases or multiple chronic conditions, are prone to using supplements like garlic, ginkgo biloba, calcium, iron, and even fish oil. These supplements are often thought to be a panacea for minor health issues, yet when combined with prescription drugs, the outcomes can be unpredictable.
Some of the key points regarding trends in supplement use include:
- High prevalence of concurrent use with prescription medications
- The belief in natural remedies as “safer” alternatives despite the potential risks
- A gap in effective communication between patients and their healthcare providers about supplement use
- An underrepresentation of standardized screening for supplement intake in routine medical history-taking
This surge in supplement use is a double-edged sword. While supplements can offer benefits, the potential for interactions with established medications is significant—especially when the supplements in question alter blood coagulation or drug absorption.
Understanding the Risk: Common Interactions That Pose Real Threats
One of the most critical areas needing attention is the interaction between blood-thinning medications and supplements that affect coagulation. For instance, anticoagulants like warfarin or antiplatelet drugs such as aspirin can interact with supplements like garlic, ginkgo biloba, and fish oil. The concern is that such pharmacodynamic interactions may dramatically lower blood clotting ability, thus increasing the risk of bleeding complications.
The tricky parts of dietary supplement interactions do not stop there. There are also pharmacokinetic issues to consider, such as the influence of minerals like calcium and iron, which may chelate and reduce the absorption of medications like levothyroxine or beta-blockers. Here, the little details become critical: a seemingly minor lapse in timing between taking a supplement and a prescription can mean the difference between effective treatment and a hazardous reduction in medication efficacy.
Below is a table summarizing some of these high-risk interactions:
| Supplement | Common Prescription Medication | Potential Interaction |
|---|---|---|
| Garlic | Warfarin | Increased bleeding risk due to enhanced anticoagulation |
| Ginkgo Biloba | Aspirin | Heightened risk of bleeding; additive antiplatelet effects |
| Calcium | Levothyroxine | Reduced drug absorption leading to diminished therapeutic effect |
| Iron | Various medications | Potential for binding and reduced bioavailability of key drugs |
| Fish Oil | Antiplatelet agents | Increased risk of bleeding, particularly during surgery |
These are just a few examples of how the combination of supplements and prescribed drugs can create tangled issues in treatment, illustrating both the subtle parts and the concerning consequences that may arise from unsupervised supplement use.
Polypharmacy and the Overwhelming Burden on Elderly Patients
Polypharmacy is a term that has become increasingly common in discussions around older adult care. When a patient is on multiple medications, the whole system may feel like a maze with many confusing bits hidden in each turn. Many older adults, who are often navigating complex healthcare regimens, face extra layers of risk when the addition of nutritional supplements is factored into the mix.
Some key observations regarding polypharmacy and supplement use in older adults include:
- Over half of the elderly take five or more medications concurrently.
- High supplement consumption is seen among those trying to manage multiple chronic conditions.
- There is a substantial subjective burden associated with keeping track of all medications and supplements, leading to potential non-adherence to prescribed regimens.
- The complexity grows as many are self-medicating with over-the-counter supplements without informing their doctors.
For many patients, this scenario is not only overwhelming but also filled with nerve-racking uncertainties about whether they might be inadvertently reducing the efficacy of their prescribed treatments. Therefore, the need to find one’s way through the labyrinth of polypharmacy is critical, and healthcare systems must take steps to offer better support systems and clearer guidance.
Communication Gaps: The Hidden Problems in Patient–Provider Relationships
One of the most nerve-racking aspects of supplement-drug interactions is not just the pharmacological effects but the systemic breakdown in communication between patients and their healthcare providers. Despite the clear risks associated with mixing supplements and drugs, many older adults do not disclose their supplement use during consultations. Likewise, medical professionals often do not consistently ask about supplement intake.
This communication failure often leaves clinicians completely in the dark about potential risks, and patients continue on a path loaded with issues that could lead to adverse effects or even serious clinical complications. In many cases, the oversight is not intentional—it is simply born from the absence of routine and structured screening approaches.
The following bullet list highlights some reasons why the communication gap persists:
- Patients may assume that “natural” supplements are automatically safe and do not require disclosure.
- Doctors may focus primarily on prescription medications and neglect to ask comprehensive questions about over-the-counter and alternative remedies.
- There can be a cultural reluctance or simply a lack of awareness that supplements might interact with modern drugs.
- The use of self-reported questionnaires in many studies has revealed that patients do not always feel comfortable discussing their full supplement routine.
Bridging this gap is a super important step in tackling the potential hazards posed by unsupervised supplement use, ultimately ensuring that the healthcare team has all the necessary information to advise patients effectively.
Strategies for Safer Use: Standardized Screening and Patient Education
Given the risks highlighted, it is clear that both patients and clinicians need to take more proactive measures. One critical strategy is the adoption of standardized screening tools for supplement use during every patient encounter, particularly at the time of medication reconciliation. Healthcare providers should incorporate a dedicated section into patient intake forms or electronic health records (EHRs) that specifically inquires about all dietary supplements, herbals, and over-the-counter products.
Such standardization ensures that the hidden pieces of a patient’s medication profile are not overlooked. By routinely “taking the wheel” on these details, clinicians can better detect potential interactions before they become a serious issue.
Furthermore, patient education plays a critical role. Educational campaigns could address the following key points:
- The risks of taking supplements without professional guidance.
- Strategies to space out the intake of prescription drugs and supplements (for example, waiting at least two hours between taking different products).
- Clear instructions on what combinations might lead to increased bleeding, reduced drug absorption, or other adverse effects.
- The importance of an honest discussion about all supplements being used, regardless of their natural origin.
The following table provides examples of educational topics for patient leaflets or online resources:
| Topic | Key Points for Patients |
|---|---|
| Understanding Your Medications | Learn about each prescription, its purpose, and how supplements may alter its effects. |
| Safe Supplement Use | Discover which supplements have been shown to interact with common medications and how to time their use properly. |
| Communication Tips | Guidelines for discussing supplement use with your doctor openly and honestly. |
| When to Seek Help | Recognize symptoms of potential drug interactions and understand when to contact your healthcare provider immediately. |
This proactive approach is not only designed to address the current gaps but also to empower patients to be active participants in their care, thus reducing the chance of harmful interactions.
High-Risk Groups: Who Should Be Extra Cautious?
Most research and studies on supplement-drug interactions indicate that certain subgroups of older adults are particularly vulnerable. Patients aged 75 and older, women, those with chronic diseases like cardiovascular complications, and individuals managing multiple health conditions are at a higher risk of encountering adverse interactions.
The reasons for this increased risk include:
- A higher likelihood of polypharmacy and a larger number of daily medications.
- The presence of physiological changes related to aging that alters the absorption and metabolism of drugs.
- A greater probability of combining prescription drugs with over-the-counter supplements without adequate medical supervision.
For these high-risk groups, the stakes are even more significant. The potential for negative outcomes is not simply theoretical: studies have shown that a notable percentage of older adults experience potential drug interactions that could lead to hospitalizations, more serious complications, or even death. Clearly, extra vigilance and targeted interventions are essential for these patients.
Healthcare providers can assist by initiating more frequent and detailed reviews of medication lists, emphasizing the timing between different products to prevent interference with drug absorption, and using clinical decision support systems in EHRs that flag potential interactions as soon as they arise.
Real-World Impact: Clinical Implications and Patient Benefits
The clinical ramifications of supplement-drug interactions extend beyond the pharmacological effects. The potential adverse interactions can lead to emergency room visits, hospitalizations, increased health care costs, and, in some cases, serious morbidity or mortality. While research suggests that actual clinical harm is concentrated among a limited number of high-risk combinations, it is still essential to be aware of even the small distinctions between potential and actual harm.
A closer look reveals several clinical implications:
- Bleeding Risks: Combining anticoagulants and supplements that inhibit platelet aggregation can lead to dangerous bleeding events.
- Reduced Efficacy: When minerals such as calcium interfere with the absorption of thyroid medications, treatment may become ineffective, leading to poor clinical outcomes.
- Drug Toxicity: In scenarios where supplement ingredients add to the side effects of medications, patients may experience symptoms that mimic toxicity, complicating diagnosis and treatment.
- Increased Burden: The sheer number of medications and supplements can overwhelm patients, leading to non-adherence and further complicating their health management.
These points underline the fact that while the theoretical risk is large, actual harm often occurs in specific, predictable circumstances. By identifying and more closely monitoring these “tricky parts,” healthcare professionals can effectively mitigate risks and improve overall patient safety. In many cases, the benefits of integrating standardized screening protocols and collaborative care approaches might well outweigh the challenges posed by these complicated pieces of interactions.
Bridging the Gap: The Role of Digital Health and Pharmacist-Led Management
In recent years, technological advances and the growing role of clinical pharmacists in healthcare management offer promising solutions to the issues at hand. Digital health tools, such as electronic health records that automatically flag potential interactions and decision support tools, are indispensable in ensuring no detail gets overlooked when doctors “take the wheel” in managing medication regimens.
Pharmacist-led medication therapy management (MTM) stands out as an essential component in addressing supplement-drug interaction risks. Pharmacists are medication experts who have the time and expertise to dig into every little twist of a patient’s medication history. They can perform comprehensive reviews, identify hidden complexities, and advise on how to correctly space the intake of various medications and supplements.
Key advantages of integrated digital health strategies and pharmacist-led management include:
- Enhanced detection of potential interactions through real-time alerts.
- Better coordination between multiple healthcare providers to ensure unified treatment plans.
- Empowering patients with clear, understandable explanations and step-by-step guidelines.
- Reducing the subjective medication burden by optimizing and simplifying drug regimens.
By working together, interdisciplinary teams can help older adults find their way through the maze of modern pharmacotherapy. This combination of technology and human oversight represents a practical solution to reduce both risks and the intimidating complexity of drug-supplement interactions.
Addressing the Overlooked Issue: Implementing Routine Supplement Screening
The evidence is clear—systematic screening for supplement use in older adults is not just optional, but a must-have measure. Here are some practical steps that can be implemented:
- Integrate Supplement History: During every clinical encounter, add clear questions in both paper and digital forms regarding the use of vitamins, minerals, nutraceuticals, and herbal remedies.
- Standardize Timing Recommendations: Advise patients to wait a designated period (for example, two hours) between taking medications and supplements.
- Use of Checklists: Develop checklists for both patients and providers to ensure no supplement is overlooked. This may include guides on which supplement-drug combinations to avoid.
- Continuous Education: Offer workshops and informational sessions where healthcare professionals and patients alike can learn about the subtle parts and the fine points of supplement-drug interactions.
The table below suggests a possible checklist that clinics could use during appointments:
| Checklist Item | Description |
|---|---|
| Current Prescription List | Review all drugs and medical conditions. |
| Supplement Inventory | Document all nutritional supplements, herbals, and OTC remedies. |
| Timing and Dosage | Record when each supplement and medication is taken. |
| Potential Interactions | Flag any known risky combinations (e.g., garlic with warfarin). |
| Follow-Up Plan | Schedule a review to adjust regimens if new supplements are added. |
These measures can transform the standard practice from one of passive vigilance to an active, informed approach that makes the most of both technology and clinical expertise.
Combining Evidence-Based Practice with Patient Empowerment
At the heart of tackling supplement-drug interactions is the need to combine evidence-based clinical practice with patient empowerment. Older adults should be encouraged to ask questions and to share all the details of their supplement routines with their healthcare providers. As patients become more informed, they can better understand the potential twists and turns that come with mixing multiple substances, and consequently, they may be more inclined to adhere to guidelines provided by their healthcare teams.
Patient empowerment can be achieved through:
- Clear Communication: Use plain language that avoids confusing jargon so that the patient can truly get into the nitty-gritty of the guidelines.
- Support Groups: Create forums where older adults can share experiences and learn from each other about safely managing their supplements and medications.
- Access to Reliable Resources: Provide links and materials from reputable sources that explain the risks and benefits of various supplements.
- Regular Reviews: Encourage periodic reviews of medication regimens, especially when a new supplement is added to the regimen.
Such approaches not only improve safety but also help to ease the anxiety that many older patients feel about managing multiple medications. As patients learn to work through these issues with greater ease, the overall healthcare experience becomes less overwhelming and more collaborative.
Looking Toward the Future: Research Gaps and Opportunities for Improvement
Despite the wealth of data available, significant research gaps remain. Many studies have relied on cross-sectional designs and self-reported data, which, although useful, do not provide definitive causal relationships between supplement use and adverse drug reactions. Future research should aim to undertake longitudinal and intervention-based studies that track patients over time, thereby allowing clinicians to identify specific moments and combinations where harm is most likely.
Key future research priorities include:
- Longitudinal Studies: Designing prospective cohort studies that follow older patients over years to observe the long-term outcomes of supplement-drug interactions.
- Randomized Controlled Trials: Conduct trials that test the efficacy of standardized screening protocols and pharmacist-led medication therapy management in reducing adverse interactions.
- Pharmacokinetic and Pharmacodynamic Research: Invest in studies that clearly map the subtle details of how supplements alter drug metabolism and absorption.
- Diverse Population Samples: Include broader demographics from low- and middle-income countries to get a global perspective on safe supplement use.
Addressing these research gaps is not merely an academic exercise, but a critical step in ensuring that our healthcare guidelines are based on robust, real-world evidence. In turn, this will enable the development of more reliable, evidence-based clinical guidelines that help older adults truly get around the tricky parts of supplement and prescription drug use.
Conclusions: Taking the Wheel Toward Safer Medication Practices
The issues surrounding supplement-drug interactions in older adults are not only clinically significant but are also steeped in everyday complexities that patients and providers alike must address. With rapidly growing numbers of seniors facing polypharmacy, the potential for dangerous interactions—from bleeding risks with anticoagulants to reduced efficacy resulting from mineral interference—remains a serious public health challenge.
Improving the situation requires a multi-pronged approach: standardized screening for supplements, improved digital health tools and pharmacist-led interventions, and robust, ongoing patient education. These steps are all essential if we are to steer through the maze of potential interactions safely. Equally, enhancing the dialogue between healthcare providers and patients about the fine points of supplement use can alleviate many of the nerve-racking uncertainties associated with current practices.
Ultimately, the responsibility rests on both the healthcare system and the patients. Clinicians must actively work to integrate supplement histories into every interaction, while patients should take a proactive role in disclosing all aspects of their health regimens. By bridging the communication gap and employing evidence-based strategies, it is possible to reduce the often-overlooked risks embedded within this full-of-problems scenario.
In a landscape where modern medicine and alternative remedies intersect, finding your path to safety demands cooperation, continual education, and a commitment to vigilance. The steps taken today not only influence the immediate health outcomes of older adults but also shape a future where medication safety is a cornerstone of quality healthcare. As the demographic shift continues, our ability to work through these challenging, complicated pieces together will ultimately determine the efficacy of treatment regimens and the wellbeing of our most vulnerable populations.
This op-ed is a call to action for healthcare providers, policymakers, and patients alike—a reminder that while supplements can offer benefits, their safe use in conjunction with prescription medications is a delicate balance, requiring our persistent attention and care. It’s a message that, with the right tools and commitment, we can indeed make our way through the twists and turns of modern healthcare safely and effectively.
By embracing a proactive, interdisciplinary approach, we take a critical step toward mitigating the risks of supplement-drug interactions, ensuring that our seniors receive the comprehensive and careful care they deserve. Let us work together to ensure that the dialogue remains open and that every detail—no matter how tangled or intimidating—is addressed with clarity, precision, and compassion.
Originally Post From https://www.cureus.com/articles/408452-pharmacological-interactions-between-nutritional-supplements-and-prescription-medications-in-older-adults-a-comprehensive-review
Read more about this topic at
Dietary Supplements: What You Need to Know – Consumer
What doctors wish patients knew about vitamins and …