Respectful Treatment in Primary Care for People with Obesity
In the realm of primary care, patients with obesity often face a host of tricky parts and tangled issues that complicate their journey toward better health. An essential aspect of their care is the treatment they receive during routine visits. Recent research demonstrates that most adults with obesity prefer an appointment where they feel genuinely respected and heard by their healthcare providers, without the nerve-racking stigma of weight bias. This approach is not resource-intensive but calls for applying common-sense practices that focus on empathy and inclusivity.
The study, which gathered input from 250 adults with obesity and even allowed them to help craft an “ideal” primary care experience, emphasizes that factors like caring treatment, active listening, and respectful referrals are critical. By centering their care around these modest yet essential practices, providers can significantly boost patient satisfaction and trust.
Patient-Centered Approaches: Why Respect and Listening Matter
For many patients with obesity, the primary care visit can feel overwhelming or off-putting. The research highlights that when patients feel their doctor treats them with care and really listens to their concerns, the quality of the visit increases dramatically. In fact, survey respondents rated an ideal visit at 9.4 out of 10 compared to an average last visit score of 8.0, underscoring that respect and empathy are not mere add-ons—they are key drivers of a better healthcare experience.
Respect and attentive listening pave the way for improved communication between the patient and healthcare provider. It allows patients to feel validated, which can translate into better adherence to treatment plans, improved motivation, and fewer missed appointments. Additionally, this patient-centered approach helps reduce the intimidating aspects that people with obesity might associate with conventional medical consultations.
Building an Inclusive Environment in Primary Care
A major takeaway from the study is the necessity for healthcare facilities to transform their spaces into hubs of inclusivity. Patients have voiced that a mere smile or a polite statement detailing that “the doctor treats me with care and respect” can offset many of the nerve-racking concerns about receiving biased treatment.
Providers can work through the following strategies to create a safe and inclusive environment for patients with obesity:
- Training staff on the subtle details of respectful communication
- Implementing policies that discourage weight bias
- Creating waiting areas that accommodate every patient size comfortably
- Using inclusive language throughout the care process
These measures may seem like small steps, but they help patients feel valued from the moment they walk in, making a positive impression that lasts well beyond the appointment itself.
Strategies to Reduce Weight Bias and Stigma in Healthcare Settings
Weight bias is a persistent problem in many healthcare settings. Its impact can be daunting—not only does it result in negative perceptions, but it can also lead to patients feeling intimidated or dismissed. The study clearly shows that nearly all participants (over 95 percent) value a healthcare approach where the doctor listens intently and refers them to specialists who continue this respectful trend.
To further get into the ways we can chip away at weight bias, consider the following tactics:
- Ongoing Education and Training: Ensure all staff members, from receptionists to specialists, participate in workshops about sensitive language, empathetic communication, and the hidden complexities of obesity.
- Empowerment through Communication Tools: Utilize questionnaires and feedback forms that encourage patients to share their experiences. These tools help in continuously improving the patient-provider dialogue.
- Personalized Care Plans: Recognize that each patient has their own set of challenges and strengths. Tailored care plans help address the little details—those slight differences in how each person experiences obesity—making each treatment plan unique and effective.
By incorporating these measures, healthcare providers can start to dismantle the nerve-racking stigma that is so commonly associated with obesity, replacing it with a more supportive, compassionate framework in primary care.
Enhancing the Primary Care Experience: Practical Recommendations
While the research clearly highlights respect and effective listening as cornerstones of a positive primary care encounter for people with obesity, there are practical steps that can further enhance these interactions. Below is a table summarizing some of the recommended steps for healthcare providers:
| Step | Description |
|---|---|
| Patient Greeting | Start with a warm, non-judgmental greeting. Ensure that the environment—from the waiting room to the examination suite—exudes warmth and acceptance. |
| Active Listening | Focus on what the patient is conveying. Use reflective questions and confirm understanding to highlight that their concerns are being taken seriously. |
| Empathetic Communication | Avoid dismissive language. Validate the patient’s feelings and experiences, ensuring they feel heard and safe. |
| Inclusive Referrals | When referring patients to specialists, ensure that these professionals are also known for their respectful treatment of people with obesity. |
| Follow-Up Care | Encourage continuous dialogue. Regular follow-ups can help monitor patient progress and address any persistent small twists in their overall care plan. |
These practical strategies aren’t just about improving the immediate satisfaction of the patient; they play a pivotal role in fostering long-term trust and engagement within primary care settings.
Improving Communication: The Doctor-Patient Dynamic
The relationship between a doctor and their patient is built on mutual trust, respect, and clear communication. When patients with obesity feel that their opinions and experiences are respected, it opens up a channel for more honest and effective dialogue. This improved communication may lead to more accurate diagnoses, better adherence to treatment regimens, and overall improved health outcomes.
Below is a list of points that can help enhance this dynamic during a primary care visit:
- Sincere Body Language: Non-verbal cues, such as eye contact and a gentle tone of voice, communicate care and respect.
- Open-Ended Questions: Allow patients to share their concerns in full detail rather than simply answering ‘yes’ or ‘no.’
- Clarification and Feedback: Summarize the conversation to ensure both doctor and patient are on the same page.
- Empathy Over Judgment: Focus on understanding the patient’s point of view rather than labeling their struggles.
- Acknowledgement of Difficulties: Recognize that living with obesity can be riddled with tension and that many may experience feelings of guilt or shame.
By incorporating these communication strategies, healthcare providers can significantly improve the core of the patient-provider interaction, making the experience far less intimidating and almost therapeutic.
Empowering Patients: The Role of Active Participation
Patients with obesity increasingly desire not just better medical care, but also an active role in shaping it. When individuals take an active role—be it by providing direct feedback, participating in designing their care plan, or even being included in research studies—the outcome of their treatment improves. These positive results occur because patients feel a sense of ownership and control over their health.
Here are several ways primary care providers can empower patients:
- Involve in Decision Making: Rather than prescribing a top-down treatment plan, work collaboratively with the patient, discussing various options and their potential outcomes.
- Educational Support: Offer resources such as nutritional guides, exercise plans, and mental health support, which can help patients feel more equipped to handle their health challenges.
- Regular Feedback Mechanisms: Utilize surveys and focused group discussions which allow patients to share their experiences and contribute suggestions for improvement.
Through these initiatives, patients with obesity get into a dialogue that is as much about managing their condition as it is about steering through their everyday life challenges. This level of engagement is essential for overcoming the hidden complexities and nerve-racking weight bias that can often taint a routine visit.
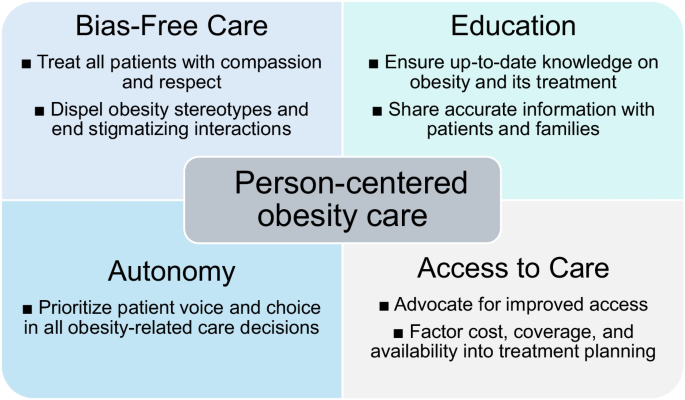
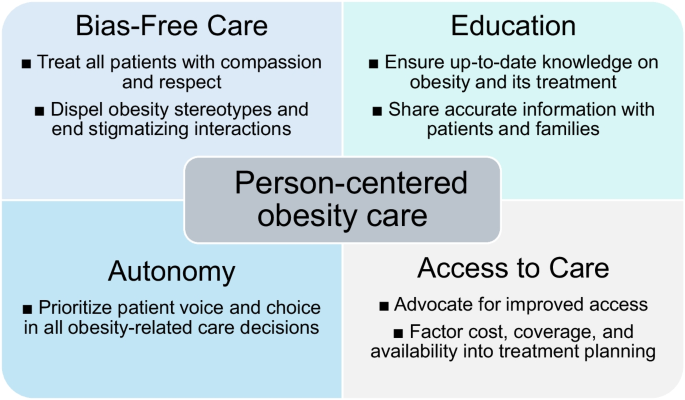
Comprehensive Obesity Management: Collaborative Care Practices
Effective obesity management requires a multi-disciplinary approach, which means that doctors, dietitians, mental health professionals, and even fitness experts need to work together as a cohesive team. Collaborative care not only addresses the physical aspects of obesity but also attends to the emotional and social challenges that come with it.
Below is a summary of how collaborative care works in practice:
- Medical Management: Involves regular visits, proper medication management, and a clear plan to address any comorbid conditions.
- Nutritional Guidance: Dietitians offer personalized meal plans that take into account individual preferences and health requirements.
- Behavioral Therapy: Mental health professionals help patients cope with the overwhelming stress and often confusing bits related to body image and self-esteem.
- Physical Activity: Fitness experts design exercise regimens that accommodate the subtle parts and little details of each patient’s physical condition.
- Social Support: Peer groups and support networks create safe spaces for sharing experiences and tackling the intimidating aspects of obesity management.
By pooling resources and expertise, primary care settings can mitigate many of the tricky parts and delicate turns that characterize obesity care, thus boosting the overall effectiveness of treatment programs.
Creating a Trust-Based Relationship with Healthcare Providers
Trust is a super important component of any healthcare relationship. For patients with obesity, feeling heard and respected can transform an otherwise nerve-racking appointment into a positive, affirming experience. When a patient trusts that their healthcare provider truly values their perspective, they are more likely to adhere to treatment plans and share vital information about their well-being.
Here are some best practices that can help establish and nurture trust:
- Consistency in Care: Regular follow-ups and consistent messaging reinforce the importance of the patient’s health and well-being.
- Transparency: Openly discuss all aspects of a treatment plan, including potential side effects and realistic expectations.
- Personalization: Tailor care plans to the unique situation of the patient, considering both their medical history and their lifestyle challenges.
- Warm Reception: From the first point of contact, every detail—from the waiting room ambience to the tone of staff interaction—should reflect inclusivity and genuine care.
An environment grounded in trust not only helps in addressing the patient’s health issues but also works to ease the fine points and hidden complexities that come with managing obesity. A trusted provider can help guide patients through rough patches and mixed feelings, giving them the confidence to figure a path toward a better life.
The Role of Continuous Feedback in Shaping Healthcare Delivery
Continuous feedback from patients is a cornerstone of evolving healthcare delivery. The survey in the study served as a shining example of how patient input can lead to a better understanding of what constitutes high-quality care in primary settings. When patients voice their experiences—both positive and negative—it allows healthcare providers to sort out the problematic areas and make necessary changes.
Feedback can be gathered through a variety of channels:
- Surveys and Questionnaires: These tools provide quantifiable data that can be used to measure patient satisfaction and pinpoint areas of improvement.
- Focus Groups: Direct interaction with a small group of patients offers a deep dive into their experiences and expectations.
- One-on-One Consultations: Allowing time during or after appointments for feedback ensures that patients feel they have been heard.
This continuous loop of feedback and improvement not only benefits the patient but also aids providers in staying updated with the latest expectations and best practices for inclusive and respectful care. By routinely revisiting and refining their approach, clinics can address the small distinctions and slight differences that can make all the difference in a patient’s experience.
Addressing the Overwhelming Challenges in Obesity Management
The journey of obesity management is often on edge for both patients and providers. The challenges include not only the physical aspects of weight management but also the emotional, psychological, and social hurdles that accompany it. Often, the twists and turns of this path may seem overwhelming, leaving patients stuck in a cycle of negative self-perception and mistrust.
Addressing these challenges requires a multi-faceted approach:
- Mental Health Integration: Including mental health professionals in the care team can help patients deal with emotional issues and boost their self-esteem.
- Tailored Nutritional Programs: Shifting focus away from generic advice, tailored programs consider the unique taste preferences, cultural background, and daily routines of the patient.
- Regular Physical Activity Guidance: Exercise should be prescribed in a way that feels safe and manageable, minimizing the intimidating prospects that come with over-ambitious routines.
- Monitoring and Adjustment: Treatment plans must be dynamic and responsive, taking into account both small distinctions in patient response and any new, nerve-racking issues that arise.
By taking a holistic view of health—one that includes both the physical and emotional dimensions—healthcare providers can empower patients to better manage their obesity in a supportive environment. This comprehensive approach is critical for breaking down the barriers that contribute to the overwhelming challenges many patients face.
Emphasizing Empathy Over Judgment in Healthcare
Central to a positive primary care experience is an empathetic approach that respects the person behind the condition. For patients with obesity, treatment that is loaded with judgment can make the clinical environment feel cold and unwelcoming. Instead, empathy should be at the forefront of every interaction.
Providers can adopt several measures to underscore empathy:
- Active Engagement: Engage patients in conversation beyond the clinical symptoms. Ask how they are feeling, what challenges they face daily, and listen without interruption.
- Non-Judgmental Language: Avoid words and phrases that carry negative connotations. Instead, opt for language that offers support and encouragement.
- Personalized Attention: Recognize the subtle parts of each patient’s case. Even the little details can have a significant impact on how comfortable they feel during their visit.
This focus on empathy not only improves the immediate care experience but can also have lasting benefits on long-term health outcomes by fostering a strong foundation of trust and mutual respect.
Reimagining Primary Care: A Call to Action
The findings from the study are a call to action for healthcare providers across the board. The evidence is clear: a primary care visit characterized by respectful treatment, genuine listening, and inclusive practices is a game changer for adults with obesity. By reimagining the traditional consultation process and incorporating common-sense practices, providers can significantly enhance the quality of care.
Moving forward, providers should work through the following action plan to elevate the care experience:
- Review Clinic Policies: Evaluate current policies on patient interaction and identify areas that may be riddled with tension or bias.
- Staff Training Sessions: Initiate regular training sessions focusing on empathy, patient-centered communication, and the fine points of respectful care.
- Create Feedback Loops: Implement systems to routinely collect and review patient feedback, and adjust practices accordingly.
- Design Inclusive Spaces: Audit the physical layout of clinics and waiting areas to ensure they are accommodating and welcoming for every patient.
- Foster Collaborative Care: Engage all relevant stakeholders—from primary care doctors to nutritionists and mental health professionals—to create a truly integrated care model.
By taking such steps, healthcare providers can figure a path that not only addresses the nerve-racking issues associated with weight bias but also builds a foundation for better overall health outcomes. The experience of a primary care visit, when redefined with respect and meaningful communication, becomes not merely a medical encounter but an empowering step on the road to wellness.
Reflections on the Changing Landscape of Obesity Care
There is a growing recognition in the medical community that obesity care must be more than the sum of its parts. From the fine shades of respectful communication to the subtle parts of collaborative treatment plans, the modern approach to obesity management is evolving beyond traditional treatment methodologies. It is a shift from viewing obesity as merely a clinical problem to appreciating it as a tangled issue that requires an integrated, empathetic, and patient-centered approach.
Healthcare providers now have an opportunity to transform the landscape through which patients with obesity experience primary care. This transformation involves rethinking long-held practices, acknowledging the hidden complexities of obesity, and embracing innovations that empower patients. In doing so, the aim is not just to treat a condition, but to champion a comprehensive, respectful, and humanistic form of care.
Key Takeaways for Healthcare Providers
Here are some crucial points that encapsulate the essence of respectful, inclusive care for patients with obesity:
- Respect and Listening are Non-Negotiable: A doctor’s ability to provide a listening ear and treat patients with sincere empathy can transform their experience.
- Inclusive Environments Build Trust: Physical spaces and institutional policies must support inclusivity, reducing the nerve-racking stigma often associated with obesity.
- Collaborative, Multi-Disciplinary Care is Essential: Combining insights from various healthcare professionals leads to a holistic treatment approach.
- Continuous Feedback is a Catalyst for Change: Regular patient input allows providers to adjust practices and keep up with evolving patient needs.
- Active Patient Participation Energizes the Process: Empowering patients to take part in decision making enriches their care experience and fosters better health outcomes.
By focusing on these key areas, clinicians can ensure that their approach is not only medically sound but also emotionally supportive, ultimately creating a care environment that is both effective and compassionate.
Looking Ahead: The Future of Primary Care for Obesity
As we look ahead, the future of primary care for individuals with obesity appears promising, provided that both clinical practices and societal attitudes continue to evolve. The insights from this study are just one piece of the puzzle—a reminder that the small, everyday interactions between a patient and their healthcare provider can make a world of difference.
Innovation in care delivery models, increased patient engagement, and comprehensive staff training represent super important steps forward. Together, these measures can help dismantle the confusing bits and nerve-racking stigma that have long plagued primary care visits for obesity patients.
In the future, we may see:
- More Personalized Care Plans: Thanks to advances in technology and data collection, care plans may become increasingly customized to address each patient’s unique needs.
- Enhanced Virtual Care Options: Telemedicine can offer a less intimidating medium for initial consultations and follow-ups, especially for those who might find in-person visits overwhelming.
- Stronger Community Support Networks: Establishing peer support groups and community health initiatives can further alleviate the issues of isolation and stigma.
- Greater Interdisciplinary Collaboration: The integration of behavioral health, nutrition, physical therapy, and primary care will likely become the new standard in obesity management.
Each of these future directions speaks to a broader vision of a healthcare environment where every patient, regardless of their body size, receives care that is respectful, comprehensive, and truly centered on their well-being.
Conclusion: A Call for Compassionate, Inclusive Healthcare
At its core, the journey toward improved primary care for people with obesity is about human connection. It is about moving away from practices laden with bias and toward an environment where every patient feels genuinely valued. By taking the time to get into the details of respectful treatment, active listening, and inclusive practices, healthcare providers can transform the intimidating experience of a primary care visit into one that is empowering and supportive.
The evidence is clear: when patients feel heard, seen, and respected, their overall experience improves—not only in terms of satisfaction but also in their willingness to engage fully with their healthcare journey. It is up to each stakeholder in the healthcare system to champion change, to figure a path through the tangled issues, and to create a future where compassionate, patient-centered care is the norm rather than the exception.
Healthcare is not just about managing symptoms or treating conditions; it is about understanding and addressing the little details that make each patient unique. As the medical community continues to adapt to the evolving needs of people with obesity, the hope is that every primary care visit will be a step towards a more inclusive, respectful, and effective healthcare experience—a true partnership in health.
Originally Post From https://www.pulmonologyadvisor.com/news/people-with-obesity-value-respect-and-being-listened-to-in-primary-care/
Read more about this topic at
How the Power of Listening can Empower the Workforce.
The Power of Listening to Cultivate Deep Respect for People