Mental Health and Obesity: Exploring the Connection
Obesity is often seen as a physical issue caused by dietary habits and inactivity, yet the tangled issues of mental health play an essential role in shaping eating behaviors. Recent insights reveal that the emotional side of obesity is full of problems that extend far beyond the number on the scale. Understanding how feelings, stress, and psychological challenges influence food choices can help both patients and clinicians figure a path toward lasting change.
The relationship between mental health and obesity is not straightforward. Instead, it is made up of a mix of little details and subtle parts that are often overlooked. Many individuals struggling with obesity face overwhelming emotional challenges like stress, anxiety, and depression – conditions that can lead to unhealthy eating patterns and, in some cases, disordered eating behaviors. In this opinion piece, we take a closer look at the connection between mental health and obesity and how clinicians can use a more compassionate approach to help their patients overcome these nerve-racking hurdles.
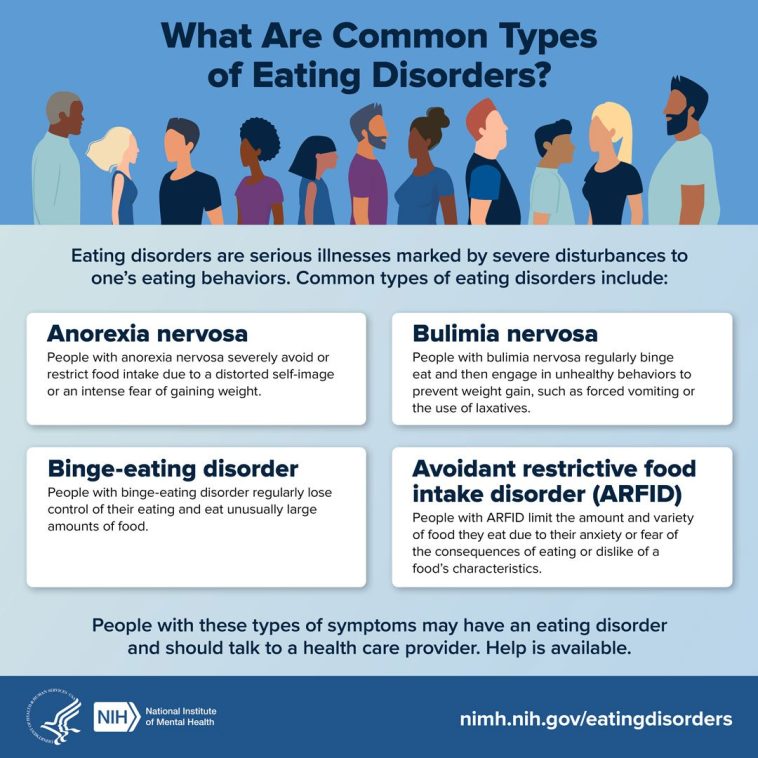
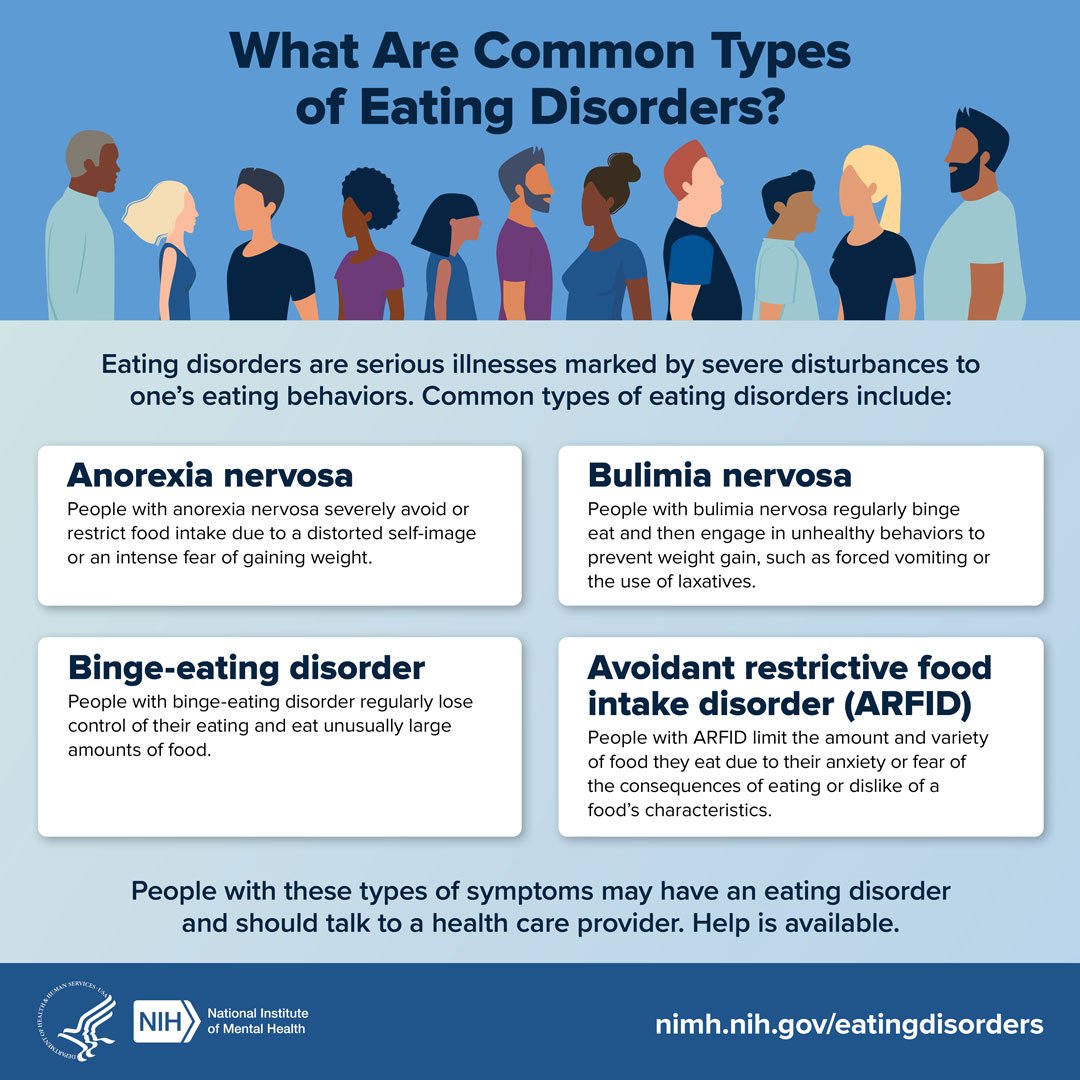
Disordered Eating: More Than Just Food
Disordered eating is often misinterpreted as a problem of willpower or poor food choices. However, these behaviors are frequently rooted in psychological factors such as emotional regulation difficulties, early life adversity, or chronic stress. For many, food becomes a tool for dealing with overwhelming feelings – a method to cope when life feels intimidating or when the weight of emotional burdens is simply too heavy to bear.
Emotional eating, binge eating disorder, night eating syndrome, and grazing are common behaviors observed among individuals with obesity. They are not just about overindulgence or lack of discipline, but rather represent attempts to self-soothe during periods of stress or low self-esteem. The hidden complexities behind these patterns reveal that food is more than a physical substance to be consumed – it is both a comfort and, at times, a trap.
Recognizing these disordered eating patterns requires that clinicians not only focus on physical health but also the undercurrents of emotional distress. In many cases, emotional stressors mingle with dietary behaviors to create a cycle that is hard to break without addressing the psychological well-being of the individual.
How Chronic Stress Influences Eating Behaviors
Chronic stress is notorious for setting off a cascade of bodily reactions that can affect metabolism and eating habits. When the body is under constant pressure, cortisol levels increase, and this hormone can lead to abdominal weight gain and reduce insulin sensitivity. This is just one of the tricky parts of understanding why many patients with obesity struggle to maintain a healthy weight.
Furthermore, high cortisol levels can make patients more susceptible to cravings for high-calorie, fat-rich, or sugar-rich foods. When stress becomes a regular part of life, the allure of these foods can become irresistible, often resulting in binge episodes. For individuals dealing with anxiety, the hypervigilance around food can sometimes cause them to create overly strict or inflexible dietary regimens, which, when broken, lead to feelings of guilt, shame, and ultimately, more uncontrolled eating.
It is essential to note that the relationship between stress and eating is full of problems – not just physiological, but also psychological. Addressing both sides of the coin is super important for anyone looking for a way to manage weight and improve overall health.
Unpacking the Psychological Factors Behind Food Addiction
A controversial yet increasingly discussed aspect in obesity medicine is food addiction. Many experts believe that the pleasure centers in the brain, fueled by dopamine and other reward pathways, respond similarly to certain foods as they do with substances like drugs. Highly processed foods, laden with sugar and fat, can trigger these reward pathways, leading some individuals into a cycle very similar to that seen in addictive behavior.
While food addiction is still debated in many clinical circles, the idea underscores the point that disordered eating behaviors involve a complex mix of neurobiological factors and psychological urges. The little twists in our brain chemistry that occur with chronic overeating serve to reinforce patterns that are exceptionally difficult to break. Just as with other forms of addiction, patients often need specialized support to untangle these patterns.
Using a combination of nutritional guidance, behavioral therapy, and sometimes pharmacological interventions, clinicians can help patients gradually rewire these reward systems. In turn, this can lead to healthier relationships with food and a reduction in compulsive eating behaviors.
Screening for Disordered Eating: Tools and Techniques
One of the critical components of managing obesity is the ability to spot disordered eating behaviors early. This is especially important because these behaviors are often hidden behind layers of emotional stress and internalized shame. Health professionals are encouraged to use validated screening tools that can bring these issues to light.
Some of the most commonly used instruments include:
- Binge Eating Scale
- Eating Disorder Examination Questionnaire (EDE-Q)
- SCOFF Questionnaire
In addition to structured screening instruments, open-ended questions play a key role in the diagnostic process. Questions such as, “Do you ever feel out of control with your eating?” or “Are there moments when you eat even if you’re not hungry?” can help bring the hidden complexities of a patient’s behavior to the forefront. By working through these inquiries, clinicians can start to piece together a more complete picture of the factors driving a patient’s obesity.
Moreover, establishing a trusting environment where patients feel comfortable discussing their mental health issues without fear of judgment is crucial. This sort of safe space encourages honesty and self-reflection, paving the way for more effective treatment plans.
Behavioral Therapies: A Comprehensive Approach to Treatment
Once disordered eating is identified, it is key for treatment to focus on both the physical and the psychological aspects of obesity. Several behavioral therapies have proven effective in addressing the overlapping issues of mental health and eating behaviors. It’s important to remember that effective treatment is not about a one-size-fits-all solution, but rather finding the right mix of strategies that work for each individual.
Among the integral treatment approaches are:
- Cognitive Behavioral Therapy (CBT): Known as the gold standard for treating binge eating disorder and emotional eating, CBT helps patients reframe negative thoughts, develop healthier coping skills, and establish more structured eating patterns.
- Dialectical Behavior Therapy (DBT): Particularly effective when past trauma or emotional dysregulation are major factors, DBT supports patients in managing their feelings while learning to tolerate distress without resorting to self-soothing through food.
- Mindful Eating Approaches: By diving into the fundamental concepts of hunger and satiety, mindful eating encourages patients to focus on the eating experience without judgment. This includes paying attention to how various foods affect energy levels, mood, and overall health.
- Motivational Interviewing: This method helps patients build internal motivation for change by exploring their own reasons for wanting to improve. It is particularly useful for individuals who feel stuck or overwhelmed by their current habits.
- Structured Meal Planning and Self-Monitoring: By reinforcing regular eating schedules and allowing patients to keep track of their food intake, these methods bring an element of routine that can alleviate some of the nerve-racking uncertainties associated with disordered eating.
Integrating these behavioral therapies into a comprehensive treatment plan requires collaboration among healthcare providers, including nutritionists, mental health specialists, and primary care physicians. Such a multifaceted approach not only helps to untangle the mind–body issues at play but also creates an environment where long-term success is within reach.
Creating a Collaborative Environment for Better Outcomes
Success in obesity management often hinges on a multidisciplinary approach where doctors, therapists, and nutritionists work together to address both the physical and emotional factors contributing to weight gain. Collaboration within medical teams leads to more nuanced care – care that takes into account the patient’s overall well-being rather than just their weight.
A collaborative treatment plan might include:
| Component | Description |
|---|---|
| Medical Evaluation | Assessing physical health, hormonal levels, and other metabolic markers that may be influenced by chronic stress or mental health conditions. |
| Mental Health Assessment | Screening for anxiety, depression, and past traumas that may be affecting eating behaviors. |
| Nutritional Counseling | Providing tailored dietary advice that considers both metabolic needs and emotional triggers. |
| Behavioral Therapy | Implementing CBT, DBT, or mindfulness-based approaches to help reshape eating habits and manage stress. |
| Physical Activity | Developing a physical activity plan that is both enjoyable and sustainable, improving overall fitness and reducing stress. |
The benefits of a team-based approach are clear: a more consistent and compassionate framework for overcoming the tricky parts of obesity that stem from mental health issues.
Stress Management Techniques for Long-Term Weight Maintenance
It is critical that individuals striving to overcome obesity not only address their dietary habits but also learn efficient ways to manage stress. The connection between stress and weight gain is full of problems that are often underestimated. When stress isn’t managed properly, it can lead to a vicious circle of unhealthy eating and further weight gain.
There are several strategies for reducing stress that can be coupled with obesity treatment:
- Relaxation Practices: Techniques such as deep breathing, meditation, or progressive muscle relaxation can help lower cortisol levels.
- Regular Physical Exercise: Aside from its benefits in burning calories, exercise acts as a natural mood booster by releasing endorphins, which can help reduce feelings of anxiety and depression.
- Structured Routines: Establishing a daily schedule that includes time for self-care, work, and leisure activities can reduce unpredictability and the discomfort often associated with excessive stress.
- Social Engagement: Meaningful interactions with friends, family, or support groups help build resilience against stress and create an environment where mental health can flourish.
- Professional Counseling: Enlisting the help of a psychologist or counselor can provide tailored strategies for managing stress. This is especially useful for individuals whose anxiety or depression has reached overwhelming levels.
By incorporating these techniques, patients can better handle the emotional twists and turns that often exacerbate both eating disorders and obesity. More than ever, tailored mental health support plays a key role in ensuring that individuals have the tools they need to confront life’s challenges head-on.
Cultural Considerations in Obesity Treatment
Obesity treatment is not one-size-fits-all. Cultural beliefs and traditions significantly influence how people view food, body image, and mental health. Recognizing these perspectives is critical for clinicians aiming for patient-centered care. What works well for one group may be less effective for another due to varying cultural understandings of health and well-being.
For instance, social events and family gatherings might center around rich, calorie-dense dishes. Together with cultural norms that emphasize robust body types as a sign of prosperity or health, these factors can make it challenging for individuals to adopt healthier eating habits. Clinicians must be aware of these subtle differences and be ready to adapt treatment strategies accordingly.
Culturally tailored interventions might involve:
- Developing nutritional plans that incorporate traditional foods while balancing calorie intake.
- Encouraging culturally specific physical activities, such as community dances or group sports.
- Collaborating with community leaders to reduce stigma and promote mental health wellness.
By taking into account these cultural twists and turns, healthcare providers can help individuals maintain a healthier lifestyle without feeling as though they are abandoning important cultural traditions.
Addressing the Gaps in Our Understanding
Despite significant progress in the field of obesity medicine, several confusing bits remain unresolved. One such gap is the lack of consensus on the diagnostic criteria and treatment strategies for food addiction. While the idea of food addiction provides a compelling explanation for some eating behaviors, more research is needed to establish standardized guidelines that can be applied in clinical practice.
Furthermore, rigorous, long-term studies that analyze psychological predictors of success in obesity treatment are still scarce. The tricky parts in this area reveal that much is left unknown about the interaction between mental health and eating behaviors over extended periods. Addressing these uncertainties will require further interdisciplinary collaboration and robust scientific inquiry.
Another significant issue is the underutilization of integrated care models where behavioral health specialists work side by side with physicians. Many patients continue to face barriers to accessing mental health services, which are critical in managing both the emotional and physical aspects of obesity. Finding effective ways to combine these disciplines is not only key for patient outcomes but is also a super important factor for future research and policy development.
Empowering Patients Through Education and Support
Empowering patients to take charge of their mental and physical health is an essential component of successful obesity treatment. Education plays a central role in this process by offering individuals the knowledge they need to manage their own well-being effectively. When patients understand the little details behind their eating behaviors, they are more likely to embrace changes, rather than feel intimidated by the process.
Several approaches can help empower patients, including:
- Workshops and Seminars: Organized sessions on nutrition, stress management, and mindful eating can provide hands-on strategies for everyday life.
- Peer Support Groups: Sharing experiences with others who are on a similar journey can reduce feelings of isolation and provide new perspectives on overcoming challenges.
- Online Resources: From webinars to interactive apps, digital resources can offer continual education and support beyond the doctor’s office.
- Individual Counseling: One-on-one sessions allow for personalized advice that takes into account each patient’s unique challenges and goals.
With a well-rounded approach to patient education, individuals gain not only the insights they need but also the confidence to manage their health proactively. This, in turn, contributes to more sustainable outcomes, as patients feel more in control of the changes they are making in their lives.
Integrating the Obesity Medicine Association’s Four-Pillar Approach
A promising framework in the world of obesity treatment is the four-pillar approach advocated by the Obesity Medicine Association (OMA). This strategy is based on four central components: nutrition, physical activity, behavioral therapy, and medical interventions. When these elements are integrated thoughtfully, they form a comprehensive treatment plan that can address both the biological and psychological twists and turns of obesity.
Each pillar plays a distinct role:
- Nutrition: This pillar is about more than just restricting calories—it is about establishing a healthy relationship with food. Tailored nutritional advice that considers individual needs, preferences, and cultural influences is critical.
- Physical Activity: Regular exercise is not only essential for burning calories but also helps in reducing stress and boosting mood. A sustainable physical activity routine can go a long way in managing weight and overall health.
- Behavioral Therapy: Addressing the mental health aspects of obesity through therapies such as CBT or DBT can help patients overcome the psychological barriers that contribute to disordered eating.
- Medical Interventions: These include both traditional and emerging treatments that cater to the unique metabolic and physiological needs of individuals. In some cases, medication or surgical options may be considered to complement other treatment methods.
Using the four-pillar approach allows clinicians to steer through the nerve-racking challenges associated with obesity by addressing the condition from multiple angles. This not only increases the likelihood of successful outcomes but also provides patients with a well-rounded strategy that includes emotional support, nutritional balance, and medical care.
Practical Tips for Clinicians and Patients
For clinicians dealing with the entangled aspects of obesity and mental health, a few practical guidelines can help streamline the treatment process. Similarly, patients can benefit from these strategies to develop healthier habits and more positive self-images.
Consider the following tips:
- Encourage Open Dialogue: Create an environment in which patients feel comfortable discussing their stress, emotions, and eating behaviors without fear of judgment.
- Implement Routine Screenings: Make the use of validated screening tools a regular part of obesity assessments to ensure early detection of disordered eating patterns.
- Personalize Treatment Plans: Recognize that each patient’s journey is unique. Use a combination of behavioral therapy, nutritional counseling, and physical activity tailored to individual needs.
- Stay Updated on Research: The field of obesity medicine is constantly evolving. Clinicians should keep abreast of the latest studies and treatment guidelines to improve patient care.
- Foster a Collaborative Network: Integrate inputs from nutritionists, mental health professionals, and specialist physicians to provide a more holistic treatment plan.
These actionable steps serve as a reminder that addressing obesity – with all its twists and turns – requires a multifaceted strategy. By managing both the body and the mind, clinicians can offer a path forward that is realistic, compassionate, and ultimately effective.
The Road Ahead: Research, Policy, and Compassionate Care
Looking into the future, there is significant hope for improvements in the ways we treat and understand obesity. Ongoing research is starting to shine a light on the fine points of how emotional stress, mental health disorders, and the neurobiology of reward contribute to eating behaviors. These advances are expected to inform more effective and nuanced treatment protocols.
Policy changes are also needed to ensure that integrated care models become standard practice. This includes better access to mental health services and more funding for obesity research. It is only through collective effort – incorporating insights from scientific research, clinical practice, and patient experiences – that we can address the nerve-racking challenges associated with obesity.
The ultimate goal is to foster a culture of compassionate, evidence-based care where patients feel empowered to take control of both their physical and emotional health. By persistently working through the confusing bits and tackling the intertwined issues head-on, the healthcare community can help ensure that the journey to wellness is less intimidating and more attainable for everyone.
Conclusion: Embracing a Comprehensive, Compassionate Approach
In sum, the relationship between mental health and obesity is layered with tangled issues that touch on everything from stress and anxiety to cultural norms and individualized treatment approaches. Recognizing that disordered eating is more than just a matter of willpower, and understanding the subtle complexities of human emotion, is super important for both clinicians and patients alike.
Through careful assessment, compassionate communication, and the integration of behavioral and medical therapies, a more holistic and effective treatment plan can be established. The future of obesity treatment depends on our willingness to get into the details of these problems, research them further, and embrace approaches that consider the mind and body as an inseparable whole.
Ultimately, by addressing the psychological underpinnings of obesity alongside its physical components, healthcare providers can help patients overcome the nerve-racking challenges that impede their path to a healthier life. With continued research, improved policy, and a commitment to compassionate care, the journey toward overcoming obesity is practically within reach – one thoughtful, collaborative step at a time.
Originally Post From https://www.healio.com/news/primary-care/20250922/how-mental-health-impacts-obesity-and-eating-behaviors
Read more about this topic at
Mind in Metabolism – A Comprehensive Literature Review …
Mood, Metabolism, and the Mind: Why Mental Health Also …