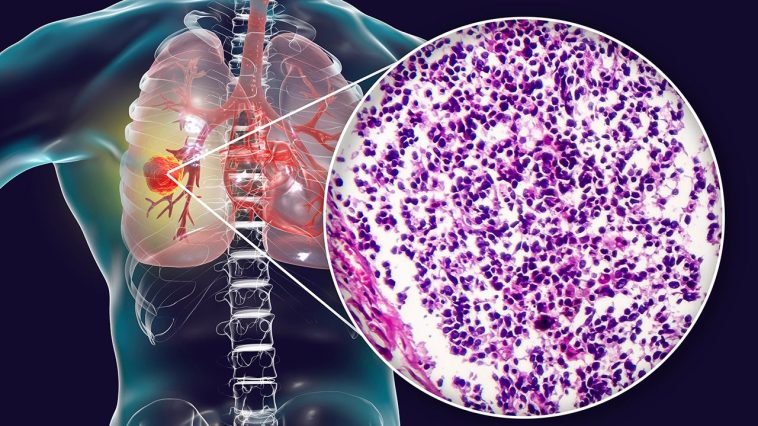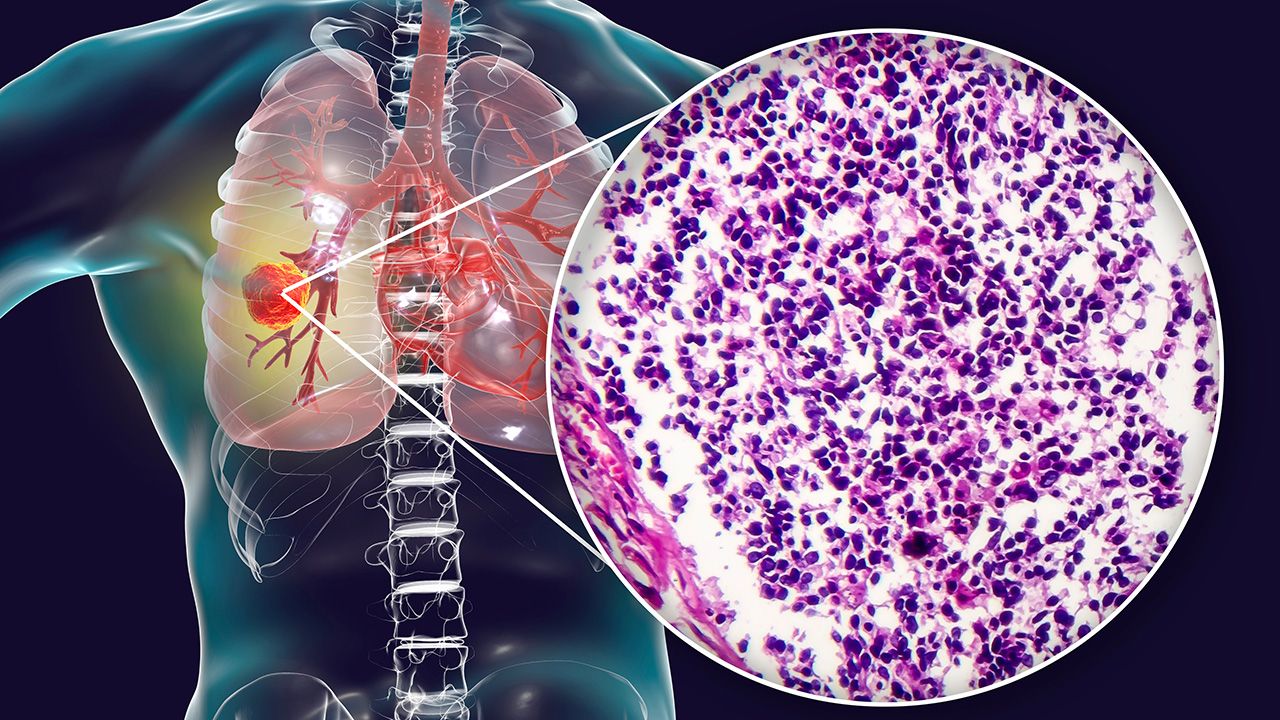
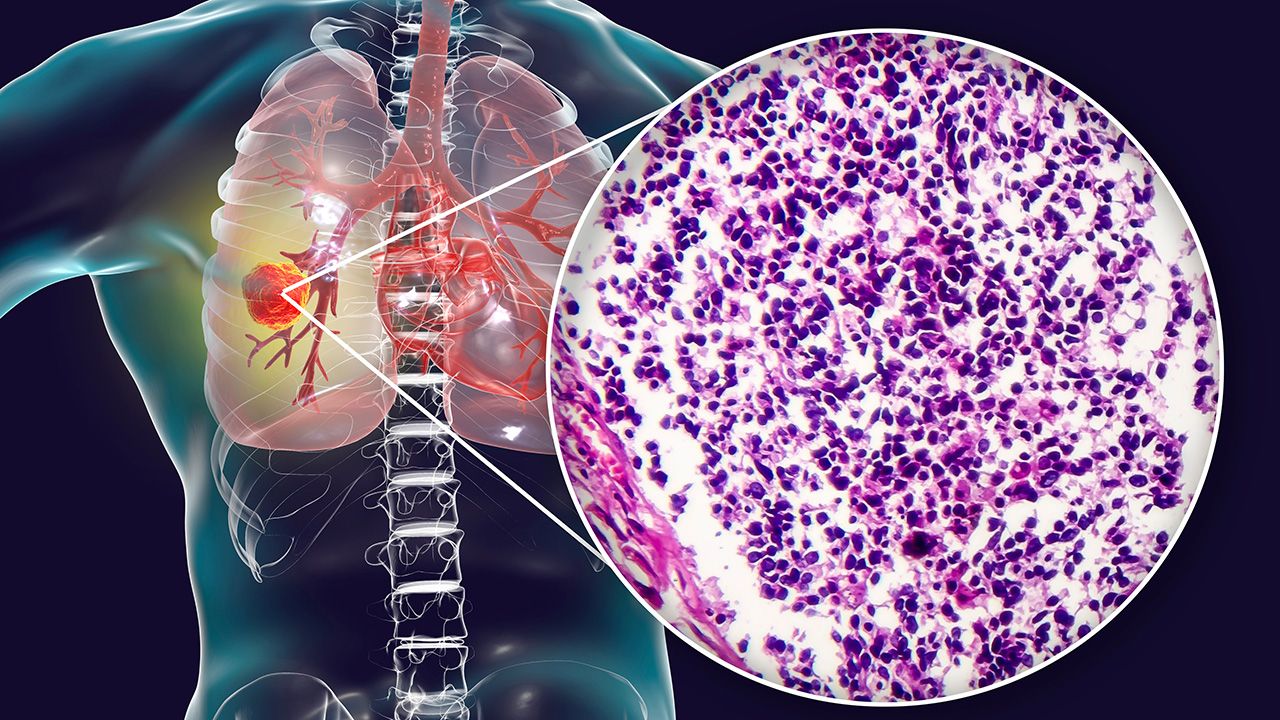
Revolutionizing Small Cell Lung Cancer Treatment: A New Era in Oncology
This opinion editorial examines the dramatic shifts underway in the treatment of small cell lung cancer (SCLC). With rapid advancements in immunotherapy and targeted agents, researchers and clinicians are uncovering approaches that seem almost revolutionary. As we take a closer look at this evolving landscape, it becomes clear that the integration of cutting-edge trials with patient-centered care is reshaping treatment paradigms. In this piece, we explore the exciting developments, the challenges of adopting these new therapies in community settings, and the importance of including patient perspectives in decision-making.
Emerging Immunotherapy Protocols: The New Frontline Strategies
Recent clinical trials, such as the IMpower133 and CASPIAN studies, have begun to transform first-line treatment for SCLC. These approaches, incorporating immunotherapy agents like atezolizumab and durvalumab alongside traditional chemotherapy regimens, are setting the stage for improved outcomes in patients. The enthusiasm is palpable, especially as evidence suggests that maintenance therapies combining novel agents, like lurbinectedin, can extend survival in carefully selected patient populations.
Subheading: Detailed Overview of Frontline Immunotherapy Trials
The IMpower133 regimen – a combination of carboplatin, etoposide, and atezolizumab – and its counterpart from the CASPIAN trial, have both shown promise in the frontline setting. These trials demonstrate how immunotherapy can be seamlessly integrated with chemotherapy to offer better overall survival outcomes for patients. The trial findings, presented at major oncology meetings, have been seen as a much-needed breakthrough in a field where treatment options were once extremely limited.
One of the promising aspects involves the IMforte trial, a study that evaluates the addition of lurbinectedin to maintenance atezolizumab. In this trial, investigators reported an overall survival benefit of nearly three months, providing hope for patients who have no brain metastases and are in robust condition after induction therapy. For clinicians, these improvements, though they might seem like simple extensions in survival time, represent significant progress given the aggressive nature of SCLC.
Subheading: How Novel Agents Like Tarlatamab are Transforming Second-Line Therapy
As frontline treatment methods evolve, significant developments in second-line therapy are emerging as well. Tarlatamab, a bispecific antibody that engages the T-cell system by binding to both DLL3 and CD3, is creating buzz among oncologists for its impressive response rates. With data suggesting a 35% to 40% response rate and a disease control rate reaching up to 70%, tarlatamab is swiftly becoming a go-to option in the second-line setting.
Despite some tricky parts – such as the need for initial inpatient monitoring due to potential cytokine release syndrome and neurotoxicity – ongoing research is already exploring ways to manage these side effects in outpatient settings. This evolution means that the patient experience may soon be less intimidating, marking a crucial step forward as clinicians seek to integrate new therapies without complicating the patient’s day-to-day life.
Sophisticated Clinical Trials and the Promise of Precision Oncology
One of the most compelling developments in SCLC treatment is the move toward precision oncology. By harnessing biomarkers and understanding the subtle details of SCLC biology, modern trials are attempting to tailor therapy based on disease subtypes. For example, the SWOG S2409 PRISM trial, a cooperative effort involving multiple esteemed cancer centers, is leveraging tissue samples taken during frontline induction therapy to classify SCLC into specific subtypes. This approach aims to assign patients with more refined therapies based on whether they are, for instance, A, N, P, or I subtypes, with additional considerations given to markers like SLFN11.
Subheading: The Role of Biomarker-Directed Therapy in SCLC
Although the fine points of using biomarkers in SCLC remain challenging, ongoing trials are trying to figure a path through the tangled issues and contradictory data. By subdividing patients into those more likely to benefit from a PARP inhibitor or an NK cell activator such as monalizumab, researchers are inching closer to personalizing treatment in scenarios where a one-size-fits-all approach once dominated. This level of customization promises to deliver more effective care, particularly for patients in high-risk categories, such as those with brain metastases.
Subheading: Benefits and Challenges of Antibody Drug Conjugates (ADCs)
Another innovative category of treatments gaining traction is antibody drug conjugates (ADCs). These therapies, which marry the targeting capacity of antibodies with the cell-killing effect of cytotoxic agents, have shown impressive activity rates – sometimes up to 50% in heavily pretreated patients. For instance, the SEZ6 antibody, ABBV-706, has demonstrated extraordinary efficacy in second-line therapy with response rates peaking at 80% in certain patient groups. With these agents, clinicians are beginning to replace or supplement components of traditional chemotherapy, potentially reshaping the frontline treatment approach entirely.
Patient Perspectives and the Importance of Reported Outcomes
No discussion about modern SCLC treatment would be complete without the patient voice. Recently, there has been an increasing emphasis on integrating patient-reported outcomes into everyday clinical practice. This push for a patient-centric approach is crucial because it allows healthcare providers to adapt therapies not only based on clinical trial data but also based on the actual experiences of patients undergoing treatment.
Subheading: Direct Patient Feedback and Shared Decision-Making
Employing patient-reported outcomes means that patients are given a more active role in their treatment plans. For example, oncologists are now taking into account not only the survival benefits of a particular therapy but also the small distinctions in life quality as recounted by those living with SCLC. Through active community engagement and regular feedback sessions, clinicians are better equipped to weigh the benefits of a new therapy against its potential side effects, especially those tricky, nerve-racking side effects that might otherwise deter a patient from continuing treatment.
Subheading: The Role of Technology in Capturing Patient Experiences
Modern technology – be it apps or web-based surveys – plays a super important role in collecting patient data. By regularly tracking symptoms and recording treatment-related adverse effects, physicians can receive real-time updates that help them adjust treatment plans more dynamically. This approach not only enhances patient care but also contributes to the growing body of real-world evidence that can inform future research and optimize treatment pathways.
Community Oncology: Bridging Academic Advances with Everyday Practice
While clinical trials conducted in large academic centers continue to inform best practices, translating these breakthroughs into community-based settings remains a challenge riddled with tension. Many community oncologists face hurdles not only in keeping up with rapid advances but also in implementing complex treatments that may have logistical and financial challenges.
Subheading: Education and Outreach as Key Solutions
To overcome these obstacles, education and effective communication are key. It is crucial that treatment advances are shared in simple language that is relevant to everyday clinical practice. Regular educational sessions, focused webinars, and collaboration between academic researchers and community oncologists are vital. These steps help ensure that even those practitioners working in resource-limited settings can offer their patients the most current and effective treatment strategies available.
Subheading: Implementing Clinical Trials in Community Settings
Another approach to overcoming these challenges is the design of clinical trials that are more pragmatic. New studies are increasingly allowing the inclusion of diverse patient populations, such as those with asymptomatic brain metastases or those who have already started treatment with chemotherapy. By enabling early intervention and reducing many of the off-putting barriers that once restricted trial participation, these studies are making it easier for community centers to be active participants in the evolution of SCLC care.
Managing Side Effects: A Patient-Centered Approach
Even as new therapies offer hope, managing their side effects remains a critical concern. The potential for immune-related adverse events can be both intimidating and nerve-racking for patients and caregivers alike. However, with careful monitoring, proactive management, and patient education, even the most complicated pieces of these treatment regimens can be handled safely and effectively.
Subheading: Outpatient Monitoring and Early Intervention Strategies
Historically, the first doses of therapies like tarlatamab necessitated inpatient monitoring for conditions such as cytokine release syndrome and neurotoxicity. However, recent advancements are beginning to pave the way for outpatient protocols that ensure patient safety without the added stress of hospital stays. This means that while the potential side effects are still there, the scary aspects are being steadily managed as clinicians find creative ways to monitor patients more flexibly.
Subheading: Comprehensive Adverse Event Management
Effective management of adverse events involves a combination of careful dose adjustment, supportive therapies, and patient education. When patients are armed with the information they need to promptly report symptoms, healthcare teams can intervene at the earliest signs of trouble. This proactive approach not only helps in mitigating the effects of side effects but also preserves the overall quality of life for patients during treatment.
Looking Ahead: Future Directions in SCLC Treatment
As the field of oncology moves forward, several key areas demand further exploration if we are to truly transform patient outcomes in SCLC. Understanding the biology of this aggressive disease is paramount, as is developing more refined strategies to sequence therapies based on individual patient profiles.
Subheading: Enhancing Our Understanding of Tumor Biology
One of the most promising avenues in the fight against SCLC is the continued exploration of its biology. By digging into the hidden complexities of tumor genetics and the subtle parts of cellular behavior, researchers are uncovering clues that may eventually lead to even more targeted and effective therapies. These insights will likely inform not only the development of new agents but also the strategies for combining and sequencing existing ones.
Subheading: The Promise of CAR T and Other Immunomodulatory Therapies
There is also growing interest in exploring CAR T-cell therapies and other immunomodulatory approaches as potential game changers in SCLC care. Although currently in the early stages, these innovative treatments offer the prospect of teaching the immune system to recognize and eliminate cancer cells more effectively. Moving these approaches from experimental trials to standard care could represent a significant turning point in the management of high-risk patients.
Subheading: Designing Future Clinical Trials with Broad Applicability
Future research must focus on trials that include diverse patient populations to truly reflect real-world scenarios. The goal is to create studies that not only generate robust data on efficacy and safety but also account for the subtle differences that can affect outcomes in various subgroups. By designing studies that are less restrictive and more inclusive, researchers can help ensure that new treatments reach a broader segment of the SCLC patient community.
The Role of Multidisciplinary Communication in Advancing SCLC Care
An essential piece of this evolving puzzle is seamless communication among oncologists, researchers, nurses, and other healthcare providers. The sharing of trial results, real-world outcomes, and patient feedback fosters an environment where different perspectives can coalesce into coherent treatment strategies. This multidisciplinary approach is not only super important in academic centers but it is equally crucial for community-based practitioners who depend on clear, accessible updates to guide their decisions.
Subheading: Multidisciplinary Tumor Boards and their Impact
Multidisciplinary tumor boards, where diverse specialists come together to review patient cases, play a critical role in integrating new treatment data into clinical practice. These forums allow for the exchange of ideas regarding the best ways to tackle SCLC, bridging the gaps between complicated trial data and practical applications. Such platforms also provide a space to discuss and troubleshoot those tricky parts that arise in real-world scenarios.
Subheading: Streamlining Communication Channels for Rapid Information Flow
Given the pace at which treatments are evolving, streamlining communication channels is of paramount importance. Effective use of digital platforms, regular updates via professional networks, and participation in conferences all contribute to ensuring that frontline providers are armed with the latest insights. This ongoing dialogue helps to foster an environment where advances in therapy can be implemented with confidence even in community settings.
Table: Key Developments in SCLC Management
| Area of Innovation | Recent Advances | Implications for Patients |
|---|---|---|
| Frontline Immunotherapy |
|
Extended survival and improved outcomes |
| Maintenance Strategies |
|
Better progression management |
| Second-Line Therapies |
|
Higher response rates in pretreated populations |
| Precision Oncology |
|
Personalized treatment based on tumor subtype |
Conclusion: Shaping the Future of SCLC Treatment
The future directions in small cell lung cancer care are both exciting and challenging. As oncology teams continue to dig into the nitty-gritty of tumor biology, devise strategic treatment sequences, and harness the power of immunotherapy, the field is poised for transformative changes. Despite the many twists and turns along the way, clinicians are steadily moving toward an era where survival gains and improved quality of life are achievable goals.
It is clear that bridging the gap between academic breakthroughs and everyday community practices will require a steadfast commitment to education, communication, and patient engagement. As new agents and trial results continue to reshape therapeutic algorithms, the collaborative efforts between researchers and community oncologists will be super important in delivering these advances to the patients who need them most.
Ultimately, embracing these novel therapies is not just about extending survival—it’s about providing hope and tangible improvements in the day-to-day lives of patients battling SCLC. While the road ahead may seem overwhelming at times, each incremental discovery and clinical advancement brings us one step closer to turning a once grim diagnosis into a manageable condition. By working through the tricky parts together, the oncology community is making meaningful strides toward a future where SCLC can be effectively tamed.
As we continue to figure a path through the evolving landscape of lung cancer treatment, both clinicians and patients can take solace in the fact that advances are coming at a rapid pace. Structured clinical trials, revamped treatment algorithms, and the invaluable insights gained from patient-reported outcomes will collectively help guide the way forward. The integration of innovative immunotherapies and precision medicine approaches heralds a new dawn in SCLC care—one that promises not only longer survival but also a better quality of life for those on this challenging journey.
In summary, the evolution of SCLC treatment is a testament to the power of research, collaboration, and patient engagement. As we move forward, it is imperative that every stakeholder – from the scientist in the lab to the nurse on the floor, and the patient at the center – remain engaged in a constant process of learning and adjusting. Such an approach will allow us to steer through those heady challenges and ultimately realize the promise of our modern, evolving therapeutic strategies.
By staying informed, sharing insights, and conducting further research into both the fine details and broad trends of SCLC biology, the oncology community can ensure that no patient is left behind. Just as progress in other forms of lung cancer has taught us the value of personalized care, SCLC is now on the brink of its own transformative era. With focus, passion, and a shared vision of improved outcomes, the journey toward redefining SCLC treatment is well underway.
As we continue to take a closer look at emerging therapies and patient-centered care strategies, it remains essential to remember that every new discovery not only transforms clinical practice but also reaffirms our commitment to those facing this aggressive disease. With each innovative trial and every breakthrough in understanding, we build a future where the management of small cell lung cancer is both effective and compassionate.
It is an exciting time for oncology—a time when every small twist and challenging turn in research is a stepping stone leading toward a brighter, healthier future for patients worldwide. Together, let us embrace these advances and work steadily to overcome the obstacles, ensuring that the innovations in SCLC treatment translate into real-world benefits for every patient on this journey.
Originally Post From https://www.cancernetwork.com/view/understanding-paradigm-changing-events-in-small-cell-lung-cancer-care
Read more about this topic at
The ADRIATIC study: revolutionizing the standard …
ME08 Revolutionizing the treatment of small cell lung cancer