Immunotherapy in Breast Cancer: A Transformative Journey
The revolution in cancer treatment has ushered in a new era for many patients, and immunotherapy has emerged as one of the most promising options for battling breast cancer. As immune-based treatments gradually reshape oncology, discussions around its success rate have become increasingly common. In this opinion editorial, we take a closer look at how immunotherapy is changing the outlook for different types of breast cancer, discussing both the benefits and the challenges involved.
At the heart of immunotherapy is the process of activating the body’s own defenses to target and destroy tumor cells. While traditional treatment approaches like chemotherapy, hormone therapy, and targeted therapy have long been used, immunotherapy offers a different angle by directing the immune system itself to fight cancer. Digging into this subject reveals both straightforward successes and some tricky parts that researchers continue to try and understand better.
Understanding the Basics of Immune Checkpoint Inhibitors
Immunotherapy in the context of breast cancer largely revolves around the use of immune checkpoint inhibitors. These drugs work by blocking specific inhibitory pathways that cancer cells use to hide from the immune system. By doing so, they help the immune system recognize and attack the tumor cells more effectively.
Checkpoint inhibitors, such as atezolizumab and pembrolizumab, have marked the first substantial steps in this direction. They function by targeting molecules like PD-1 and PD-L1—components that, under normal circumstances, serve as important regulators of the immune response. However, cancer cells often exploit these molecules to suppress the immune system, thereby enabling unrestrained growth and spread. Steering through these complicated pieces means that once these barriers are removed, the body’s own defenses can get to work in a way that many traditional treatments cannot achieve.
For instance, in the treatment of triple-negative breast cancer (TNBC), which is notorious for its aggressive behavior, these drugs have shown impressive results compared to conventional therapies. As the most immunogenic form of breast cancer, TNBC generally has higher levels of tumor-infiltrating lymphocytes and elevated PD-L1 expression, making it particularly receptive to immune-based treatments.
Immune Checkpoint Therapy Benefits for Triple-Negative Breast Cancer
Triple-negative breast cancer is often the focus when discussing immunotherapy because it lacks the targets that are commonly found in hormone receptor–positive and HER2-positive cancers. The aggressive nature and limited treatment options for TNBC have spurred both clinicians and researchers to explore new therapeutic avenues.
Recent clinical trials have shown that in metastatic PD-L1–positive TNBC, combining immunotherapy with chemotherapy can produce an objective response rate of between 35% and 40%. Additionally, in early-stage TNBC, studies report that the combination can lead to pathologic complete response rates of over 60%, which is a significant improvement compared to the rates achieved with chemotherapy alone.
One of the pivotal studies, known as the IMpassion130 trial, showcased that patients treated with atezolizumab in combination with chemotherapy experienced notably longer progression-free periods. In numerical terms, median progression-free survival increased from 5.0 months with chemotherapy alone to 7.5 months when atezolizumab was added—translating to a 38% reduction in the risk of disease progression.
Similarly, pembrolizumab has proven its worth in a trial named KEYNOTE-355, where its combination with chemotherapy increased the median overall survival for patients with PD-L1–positive TNBC from 16.1 months to 23.0 months. These positive results have made pembrolizumab a key part of the treatment arsenal, especially for patients whose tumors express high levels of PD-L1.
Exploring the Early-Stage Therapeutic Potential
Immunotherapy shows even greater promise when applied in the early stages of breast cancer. Using this treatment modality alongside traditional chemotherapy before and after surgery is becoming increasingly popular. A well-known study in this space, the KEYNOTE-522 trial, demonstrated the benefits of this combined approach in patients with high-risk early TNBC.
The results were quite compelling. Patients who received the combined therapy of pembrolizumab and chemotherapy managed to achieve a pathologic complete response rate of 64.8% compared to 51.2% in the group treated with chemotherapy alone. Additionally, there was a notable improvement in three-year event-free survival rates—from 76.8% to 84.5%. Such statistics not only underscore the potential of immunotherapy in early-stage disease but also help to shape new treatment paradigms that could offer better long-term outcomes for patients.
Subtype-Specific Outcomes: Comparing Breast Cancer Types
It is important to note that the effectiveness of immunotherapy in breast cancer can vary widely depending on the specific subtype of the disease. While triple-negative breast cancer has emerged as the primary beneficiary, other subtypes have not shown the same level of responsiveness.
For instance, in HER2-positive breast cancer, attempts to combine checkpoint inhibitors with HER2-targeted therapies like trastuzumab have produced modest response rates—typically in the range of 10–15%. Meanwhile, hormone receptor–positive breast cancer, which is generally less immunogenic in nature, tends to show response rates of below 10%. Although these smaller numbers might seem discouraging, researchers are still testing new combinations involving CDK4/6 inhibitors and other agents to improve outcomes for these subtypes.
Below is a table that summarizes the typical response rates across various breast cancer subtypes based on current research:
| Subtype | Average Response Rate (Metastatic) | Pathologic Complete Response (Early-Stage) |
|---|---|---|
| Triple-Negative Breast Cancer | 35-40% (PD-L1–positive) | Above 60% |
| HER2-Positive Breast Cancer | 10-15% | Data emerging |
| Hormone Receptor–Positive Breast Cancer | Below 10% | Data emerging |
This differentiation in response underlines the need for a more personalized approach to immunotherapy, one that takes into account individual tumor biology, PD-L1 expression, tumor-infiltrating lymphocytes, and tumor mutational burden. These elements can help physicians better predict which patients are most likely to benefit from these treatments.
Combination Strategies to Overcome Inhibitory Pathways
While immunotherapy represents a significant step forward, it is not without its tangled issues and challenges. Not all patients respond favorably, and resistance—whether inherent or acquired—remains a daunting hurdle. One of the most promising approaches to overcome these challenges involves using combination strategies that target multiple biological pathways at once.
Among the most successful approaches is the combination of immunotherapy with chemotherapy. This strategy leverages the ability of chemotherapy to increase the release of tumor antigens, which in turn helps the immune system better recognize the cancer cells. Other emerging combinations include pairing immunotherapy with PARP inhibitors, particularly in tumors with BRCA mutations, as well as combining immune checkpoint inhibitors with radiotherapy. Radiotherapy, when used appropriately, can induce immunogenic cell death and thus further enhance the immune system’s ability to fight cancer.
Key bullet points to consider when evaluating combination strategies include:
- Chemotherapy + Immunotherapy: Elevates tumor antigen release, potentially increasing immune recognition and response.
- PARP Inhibitors + Immunotherapy: Especially beneficial for BRCA-mutated tumors, offering a synergistic attack on cancer cells.
- Radiotherapy + Immunotherapy: Induces immunogenic cell death, paving the way for better immune system activation.
- HER2-Targeted Therapies + Checkpoint Inhibitors: Aim to leverage the dual approach in enhancing immune activation in HER2-positive cancers.
These combination strategies offer hope for increasing overall success rates in patients who might otherwise see limited benefits from single-modality immunotherapy. However, each combination comes with its own set of challenges and potential side effects, meaning that careful patient selection and close monitoring are both critical and must be emphasized.
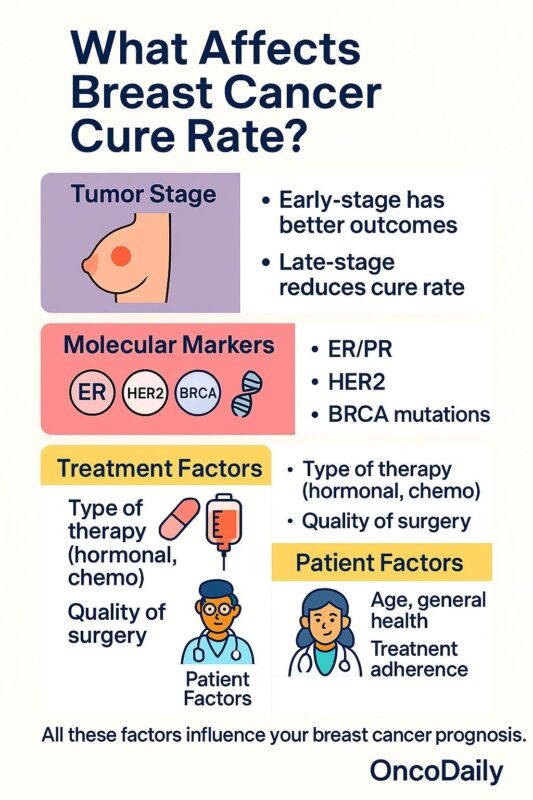
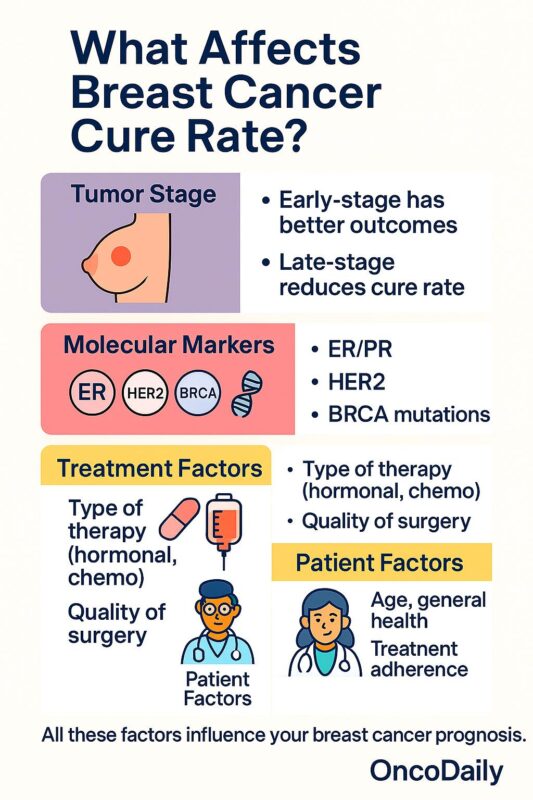
Factors that Influence the Success of Immunotherapy
Understanding why some patients respond so well to immunotherapy while others do not involves untangling several intertwined factors. Among these, PD-L1 expression emerges as one of the most essential markers. Generally, tumors with higher PD-L1 expression tend to respond better to immune checkpoint inhibitors, making this biomarker critical in guiding therapy.
Other elements that play a role include:
- Tumor-Infiltrating Lymphocytes (TILs): Their presence can indicate a more active immune environment within the tumor, which bodes well for the efficacy of immunotherapy.
- Tumor Mutational Burden (TMB): A higher TMB means that the tumor displays more neoantigens, which can help the immune system distinguish cancer cells from normal cells.
- BRCA Mutations: These genetic alterations not only contribute to the development of cancer but also might enhance the formation of neoantigens, thereby making the tumor more susceptible to immune responses.
These factors, when assessed together, provide a more nuanced picture of which patients might derive the highest benefits from immunotherapy. Therefore, clinicians increasingly rely on comprehensive diagnostic tests to figure a path through the fine points of immunotherapy treatment decisions.
The Safety Profile: Side Effects and Management
No discussion about immunotherapy would be complete without addressing its safety profile. While the prospect of mobilizing the body’s immune system against cancer holds tremendous promise, it can also lead to a range of immune-related side effects. These include issues like thyroid inflammation, pneumonitis, hepatitis, and skin reactions. Typically, these events occur in about 15–20% of patients and, while potentially overwhelming, are often manageable with proper intervention.
Compared to the long-term toxicities associated with traditional chemotherapy, immunotherapy generally offers a more favorable safety profile. The side effects tend to be less severe and more amenable to management with treatments such as corticosteroids. Nevertheless, clinicians must be vigilant, and patients should be well-informed about the possibility of these reactions so that they can seek timely treatment if needed.
Some of the notable points about managing immunotherapy side effects include:
- Early Detection: Routine monitoring of thyroid function, liver enzymes, and respiratory status is critical for early identification of side effects.
- Prompt Intervention: Using corticosteroids and other immunosuppressive agents can control immune-related adverse events once detected.
- Patient Education: Ensuring that patients are aware of potential side effects can lead to faster reporting and management, ultimately reducing the risk of severe complications.
- Personalized Management Plans: Individual differences in response and side effect tolerance mean that treatment plans should be tailored to each patient’s needs.
Emerging Trends: The Future of Breast Cancer Immunotherapy
The landscape of immunotherapy is not static. Rapid advancements in technology and a deeper understanding of the immune system continue to fuel innovation in this space. Researchers are now testing new immune checkpoint inhibitors that target alternative molecules such as LAG-3, TIGIT, and TIM-3. In addition, personalized cancer vaccines and CAR T-cell therapies aimed at breast-specific antigens like MUC1 and HER2 are under early investigation.
These evolving approaches are expected to broaden the applicability of immunotherapy beyond just TNBC, eventually extending benefits to patients with HER2-positive and hormone receptor–positive cancers as well. Importantly, the integration of genetic and immune profiling into routine clinical practice will help refine treatment plans further, ensuring that each patient receives a tailored approach that maximizes the likelihood of success.
In sum, the promise of immunotherapy rests not only on its current successes but also on its potential to evolve. While the present reality shows the greatest benefits in PD-L1–positive TNBC, ongoing research and continued clinical trials are set to tweak and improve treatment strategies further. This progress, although accompanied by some nerve-racking challenges, fuels hope for a future where immunotherapy could offer a universal edge in the fight against breast cancer.
Patient Perspectives and the Real-World Impact
Beyond the numbers and clinical data, the true impact of immunotherapy is best understood from the viewpoint of those who have experienced it firsthand. Many patients report a noticeable improvement in quality of life—a key benefit not always captured in clinical statistics. Even when side effects are present, the potential to extend survival and reduce the disease burden provides a compelling reason to opt for these treatments.
While some patients may feel intimidated by the complex treatment plans and the possibility of side effects, the successes observed in clinical trials are encouraging. These trials have not only paved the way for approval by regulatory agencies but have also instilled confidence among oncologists and patients alike, serving as a beacon of hope in times that can otherwise feel overwhelming.
A few real-world experiences shared by patients include:
- Improved Daily Functioning: Many have noted enhanced energy levels and a return to normal activities, even during treatment.
- Enhanced Mental Strength: The psychological boost of knowing that the immune system is actively fighting the cancer can greatly improve a patient’s outlook.
- Better Tolerance of Side Effects: With proper management, side effects are often less disruptive than those experienced with conventional chemotherapy.
- Hope for the Future: The progress and continuing improvements in treatment protocols instill optimism for patients facing long-term battle with the disease.
These testimonials underscore why a balanced discussion involving realistic expectations and clear communication about benefits and challenges is essential when considering immunotherapy.
Strategic Directions: How Oncologists Plan and Adapt
For clinicians, the decision-making process surrounding immunotherapy is filled with subtle details and a range of variables that need careful thought. Finding your way through the clinical trial data, past experiences, and the evolving landscape of immune checkpoint inhibitors is no small feat. Oncologists must often weigh the potential benefits against the risks when determining whether a patient is a good candidate for these novel treatments.
Some of the key strategic directions include:
- Biomarker Assessment: Routinely assessing PD-L1, tumor-infiltrating lymphocytes, and tumor mutational burden helps personalize treatment decisions.
- Collaborative Decision-Making: A multidisciplinary approach involving oncologists, radiologists, and pathologists ensures that all aspects of the patient’s condition are taken into account.
- Ongoing Monitoring: Regular follow-ups and imaging studies are critical in making sure that the patient is responding well and adjusting treatment plans as needed.
- Patient Involvement: Ensuring that patients understand the risks, benefits, and potential side effects helps them make informed decisions about their treatment options.
By adopting these strategies, oncologists are better able to figure a path through the fine points of immunotherapy treatment, offering hope to patients while managing potential challenges head on.
Bridging the Gap Between Research and Real-World Applications
One of the most encouraging aspects of modern immunotherapy is the way it is steadily moving from research centers into everyday clinical practice. The initial excitement surrounding immunotherapy trials has seeped into oncological practice worldwide. Yet, the transition is not free from its share of tangled issues and subtle details. Bridging this gap requires a constant feedback loop between research institutions and treatment centers.
Academic centers and community hospitals are beginning to work more closely together, sharing data and refining best practices. This collaboration helps ensure that the findings from clinical trials can be quickly and efficiently translated into better patient care protocols. Some of the main areas of focus include:
- Standardizing Biomarker Testing: Ensuring consistent measurement of PD-L1 expression and other critical biomarkers can help fine-tune patient selection for immunotherapy.
- Expanding Clinical Trials: Greater patient enrollment in diverse demographics helps to better understand the overall effectiveness of immunotherapy across various populations.
- Real-World Data Collection: Observing how patients fare outside of controlled clinical trial environments provides invaluable insights into efficacy and side effects in routine practice.
This pragmatic approach is essential to improve survival rates and quality of life across the spectrum of breast cancer patients. With continued scientific progress and a close-knit collaboration between researchers and practicing clinicians, immunotherapy is poised to become an even more effective tool in the fight against breast cancer.
Challenges and Opportunities: Balancing Hope with Realism
Although the advances in immunotherapy are promising, the journey ahead is still full of tricky parts and overwhelming challenges. The response rates seen in clinical trials are not universal, and a significant number of patients continue to demonstrate resistance to these treatments. However, these challenges open up avenues for further research and development.
One of the key opportunities lies in the refinement of combination strategies. By pairing immunotherapy with other treatment modalities, clinicians hope to overcome some of the nerve-racking resistance mechanisms exhibited by certain tumors. Ongoing research focuses on the following areas:
- Optimizing Dosage and Timing: Finding the right balance in treatment schedules to maximize benefits while minimizing side effects.
- Developing Novel Agents: Introducing new immune checkpoint inhibitors that target alternative pathways can potentially improve outcomes.
- Enhancing Patient Selection: Using advanced diagnostic tests to accurately predict which patients will benefit the most from these therapies.
- Educating Healthcare Providers: Continuous training and knowledge sharing about the latest advancements can help professionals steer through the evolving landscape of immunotherapy.
While the road ahead is undeniably complicated by various twists and turns, the opportunities presented by these emerging strategies provide renewed confidence in the fight against breast cancer. The balance of hope with realism remains a cornerstone of patient care, ensuring that patients receive treatments that are both innovative and tailored to their specific needs.
Conclusion: A Promising Horizon for Immunotherapy in Breast Cancer
In conclusion, immunotherapy represents a major leap forward in the realm of breast cancer treatment. The impressive success rates in PD-L1–positive triple-negative breast cancer, along with promising data from early-stage trials, underscore its potential as a game-changing modality in oncology. While challenges do exist, particularly with regard to hormone receptor–positive and HER2-positive subtypes, ongoing research and new combination approaches offer hope for improved outcomes across all forms of the disease.
The journey of immunotherapy is ongoing and filled with a mix of encouraging success and nerve-racking obstacles. As research continues to push the boundaries of what is possible, multidisciplinary collaboration and personalized treatment strategies will be key to ensuring the best possible outcomes for patients.
Ultimately, the future of breast cancer treatment certainly looks brighter with immunotherapy leading the way. With further scientific advances on the horizon and a steadfast commitment by the medical community, the immunotherapy success rate is expected to rise, offering a lifeline to patients across the entire spectrum of breast cancer. It is an exciting time in oncology—a time where hope, innovation, and perseverance are converging to redefine how we approach one of the most challenging diseases of our time.
For patients, their families, and clinicians alike, immunotherapy is more than just a treatment option; it is a beacon of progress that continues to inspire new strategies, collaborations, and, most importantly, renewed optimism for a cancer-free future.
Originally Post From https://oncodaily.com/oncolibrary/389562
Read more about this topic at
Immunotherapy before and after surgery improves …
New Immunotherapy Strategy Improves Outcomes in …