Reinventing Breast Cancer Treatment: Embracing Personalized Hormone Therapy
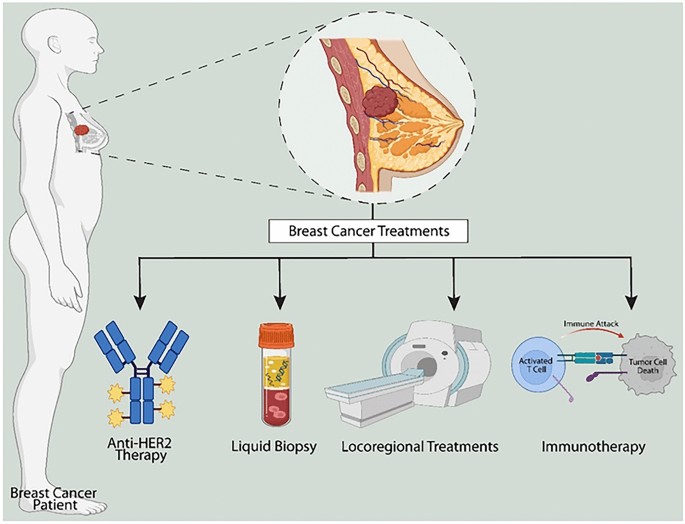
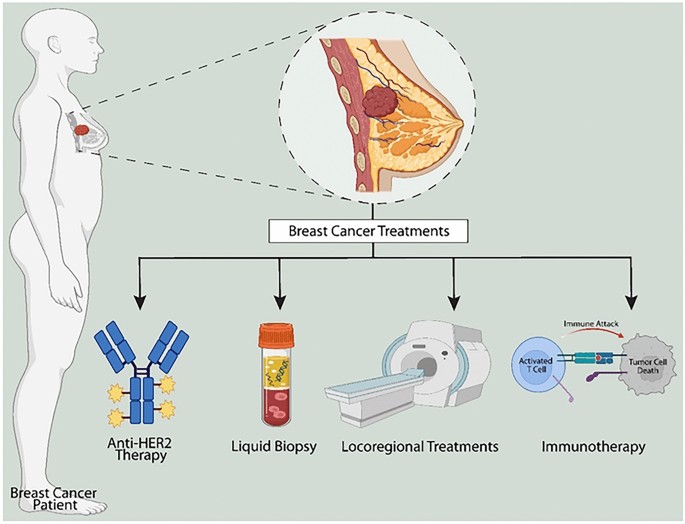
Breast cancer has long been recognized as one of the most common malignancies among women around the globe. While decades of research have improved our understanding and treatment of this disease, the journey is still punctuated by tricky parts and tangled issues. A prime example lies in the realm of hormone-dependent breast cancer treatment, where the effectiveness of tamoxifen—a staple drug for decades—can be limited for some patients. Recent developments from the Dr. Margarete Fischer-Bosch Institute of Clinical Pharmacology invite us to take a closer look at personalized therapy options that might well redefine treatment outcomes for many patients.
This opinion editorial aims to explore the evolution of personalized breast cancer treatments, particularly focusing on a new therapy approach that supplements tamoxifen with its active metabolite in cases where its efficacy is less than optimal. We will critically examine the scientific rationale behind this strategy, the clinical evidence emerging from recent multicenter studies, and how this innovative approach might shape the future of oncology treatment protocols.
Understanding the Tricky Parts of Tamoxifen Metabolism
One of the central challenges in hormone-dependent breast cancer treatment lies in the way tamoxifen is processed by the body. Tamoxifen works by preventing estrogen—a hormone known to drive the growth of some breast cancers—from binding to receptors on cancer cells. However, the effectiveness of the medication is deeply entwined with a series of metabolic events that convert tamoxifen into its more active form, (Z)-endoxifen.
Unfortunately, not every patient’s body is equally capable of oxygenating the drug into its potent variant. The enzyme CYP2D6 plays a key role in this conversion, and its activity is governed by the patient’s genetic blueprint. For approximately one-third of patients, this conversion proceeds at a slower or less efficient rate. These patients end up with lower levels of (Z)-endoxifen, which can inadvertently contribute to a higher risk of cancer recurrence. The chemistry and biology behind this are filled with fine points that researchers are only now beginning to fully appreciate, emphasizing the need for individualized treatment plans.
The genetic underpinnings of CYP2D6 variability create small distinctions in drug metabolism among patients. These slight differences in enzyme function might appear as little twists, yet they lead to significant implications in treatment outcomes. Field experts have long acknowledged that one-size-fits-all medication regimens can overlook these subtle, yet critical, differences.
Personalized Treatment: Supplementing with (Z)-Endoxifen
In the quest to enhance tamoxifen’s performance, researchers have turned their attention to a promising solution: directly supplementing (Z)-endoxifen. Under the project name TAMENDOX, this strategy involves adding the active metabolite to patients whose genetic profiles are such that their natural conversion process is inadequate. Essentially, rather than subjecting patients to the nerve-racking uncertainty of whether their bodies can muster the necessary biochemical changes, TAMENDOX ensures that a precise, therapeutic level of the active drug is delivered directly.
This targeted approach to hormone therapy has multiple appealing aspects:
- It directly addresses the off-putting bottleneck caused by CYP2D6 variability.
- It promises higher concentrations of active drug in the bloodstream, akin to what is observed in patients with naturally efficient metabolic pathways.
- It offers clinicians a way to tailor treatments, making use of the patient’s genetic background as a guide.
- It highlights the potential for personalized medicine to boost treatment effectiveness and potentially reduce the risk of recurrence.
By providing a supplemental route to achieve the necessary drug concentration, TAMENDOX is at the forefront of personalized medicine, marking a significant shift away from conventional treatment strategies.
Breaking Down the Clinical Evidence: A Closer Look at the Studies
The new approach was not merely a theoretical innovation; it was rigorously tested in a multicenter clinical study. The study, directed by the research team at the Bosch Health Campus in collaboration with 38 clinics across Germany, engaged a diverse group of 235 patients diagnosed with early-stage, hormone receptor-positive breast cancer. This broad base of participants allowed researchers to dig into the nitty-gritty of tamoxifen’s performance across different genetic profiles.
The study design was carefully calibrated to compare two groups: one that received tamoxifen in isolation (monotherapy) and another that received tamoxifen in conjunction with supplemental (Z)-endoxifen. To keep pace with the slight differences in individual metabolism, these patients were further stratified based on their genetic status and the levels of the drug measured in their bloodstream over a six-week period.
The outcomes were encouraging. The patients who received the combination therapy not only achieved the target drug concentration in their blood, but they did so in a manner that mirrored the levels typically found in patients who naturally metabolize tamoxifen efficiently. These results shine a spotlight on how personalized medicine can troubleshoot the tricky parts of an established therapy, thereby enhancing its effectiveness.
Overcoming the Confusing Bits: The Role of Genetic Variability
Genetics plays a super important role in shaping how the body responds to medications, and this is particularly evident with tamoxifen. The enzyme CYP2D6, which is crucial for converting tamoxifen into (Z)-endoxifen, displays varying levels of activity across different individuals. This variability can be a source of both challenge and opportunity. On one hand, it creates confusing bits in the treatment algorithm; on the other, it opens up avenues for tailored interventions.
Consider the following overview of what genetic variability means for tamoxifen metabolism:
| Metabolic Category | Description | Clinical Implication |
|---|---|---|
| Normal Metabolizers | Patients whose CYP2D6 enzyme functions adequately, ensuring sufficient conversion of tamoxifen to (Z)-endoxifen. | Standard tamoxifen monotherapy is generally effective. |
| Poor Metabolizers | Patients with genetic variations that reduce CYP2D6 activity. | Increased risk of suboptimal drug levels, heightening the chance of recurrence. |
| Intermediate Metabolizers | Patients with some reduction in metabolic function, leading to variable drug responses. | May benefit significantly from supplemental strategies like TAMENDOX. |
This table is intended to clarify the subtle parts of individualized drug response and highlight how personalized care can be sculpted around the patient’s genetic landscape.
The Impact on Premenopausal Women: A Much-Needed Treatment Alternative
The implications of enhancing tamoxifen therapy extend beyond addressing genetic differences—they also provide new hope for populations with limited treatment options. For example, premenopausal women with hormone-dependent breast cancer often face more restricted alternatives compared to their postmenopausal peers. Aromatase inhibitors, another class of hormone therapy drugs, are generally not recommended for younger women. In this landscape, a tailored approach using TAMENDOX can be a transformative option.
By ensuring that even those with inefficient drug metabolism can reach the necessary therapeutic levels, TAMENDOX offers a direct answer to a long-standing problem. This not only promises improved outcomes but also secures a more balanced approach to managing the broader spectrum of breast cancer cases.
When weighing the available therapeutic strategies, it becomes clear that personalized treatment is not merely a trendy buzzword—it is an essential step toward making sure that no patient is left behind due to genetic or metabolic peculiarities.
Evaluating Safety and Tolerability: Do the Benefits Outweigh the Risks?
Any new intervention must be scrutinized not just for its effectiveness but also for its safety profile. In the case of TAMENDOX, the clinical study revealed that the new treatment method was very well tolerated by patients. The side effects, which were mild and comparable to those observed in the tamoxifen-only group, suggest that adding (Z)-endoxifen does not introduce any new, overwhelming risks.
This finding is a considerable reassurance for clinicians and patients alike. Here’s a quick breakdown of the safety profile observed in the study:
- Side effects were reported at similar rates between the combination therapy and tamoxifen monotherapy groups.
- The overall tolerability was high, with most adverse events being categorized as mild.
- Patients, regardless of metabolic status, did not experience significant changes in quality of life solely due to the supplemented therapy.
From an opinion standpoint, the safety data are as critical as the efficacy measures. The fact that the new regimen did not introduce additional severe complications is a super important factor in its favor, potentially paving the way for broader clinical acceptance and regulatory approval.
Personalized Medicine: Bridging the Gap Between Research and Patient Care
One of the most exciting aspects of the TAMENDOX study is how it underscores the promise of personalized medicine—a field that has witnessed rapid growth in recent years. Personalized medicine is not just about tailoring treatments based on a patient’s genetic profile; it also involves making the best use of existing therapies by fine-tuning their delivery. In this context, addressing the tricky parts of drug metabolism in breast cancer treatment is an exemplification of how targeted intervention can lead to significantly better therapeutic outcomes.
There are several key points to consider when discussing this revamped approach:
- Individualized Treatment Plans: By taking into account the patient’s genetic makeup, oncologists can move away from a one-size-fits-all treatment model and instead craft individualized plans that meet specific metabolic needs.
- Enhanced Drug Efficacy: Supplementing tamoxifen with (Z)-endoxifen ensures that all patients, regardless of their genetic profile, achieve effective drug levels in the bloodstream.
- Reduction in Recurrence Risk: Improving drug efficacy is a critical component in reducing the overall risk of breast cancer recurrence, thus potentially extending the lives and improving the quality of life for many women.
This approach represents a significant shift in the thinking around breast cancer therapy. It reflects a broader trend in modern medicine: the growing recognition that successful treatment often hinges on accounting for both the visible and hidden complexities of human biology.
Getting into the Fine Points of Clinical Studies and Collaborations
It is important to understand that breakthroughs in medicine are rarely the result of isolated experiments. Instead, they emerge from extensive collaborations and multicenter studies—efforts that bring together the best minds in the field. The clinical study underpinning the TAMENDOX strategy is a prime example of how cooperation among various institutions can lead to significant advancements in patient care.
Key highlights from the study include:
- Involvement of 38 clinics spread across Germany, ensuring a diverse patient demographic is included in the analysis.
- A robust sample size of 235 patients, lending statistical power to the study’s conclusions and reinforcing the reliability of the findings.
- A carefully monitored six-week treatment period during which the drug levels in the bloodstream were meticulously recorded and analyzed.
Such collaboration is loaded with challenges—from aligning protocols across multiple centers to ensuring uniformity in data collection. Yet the successful execution of this study is a strong testament to how the medical community can come together to find solutions to the challenging bits of long-standing treatment dilemmas.
Understanding the Clinical Implications: What This Means for Future Therapies
The potential benefits of personalized hormone therapy extend well beyond breast cancer. The core principle of supplementing a drug’s active form to overcome a patient’s metabolic limitations could have far-reaching implications in other therapeutic areas where drug metabolism plays a key role.
Consider the following broader implications:
- Precision in Drug Dosage: This approach encourages clinicians to move toward dosage regimens that are fine-tuned according to the patient’s genetic and metabolic profile.
- Minimizing Adverse Events: By ensuring that each patient receives just the right amount of medication, there is potential to reduce the incidence of drugs being over- or under-dosed, thus lowering the risk of adverse events.
- Expanding the Reach of Existing Therapies: For drugs that have been limited by metabolic hurdles, supplement approaches like TAMENDOX open up a pathway to broaden their utility and improve their success rates.
This paradigm shift could lead to more tailored interventions not only in oncology but also in various other fields such as cardiology, neurology, and endocrinology—where genetic variability can similarly impact treatment effectiveness.
Addressing the Hidden Complexities of Personalized Drug Approaches
While the promise of personalized therapy is undeniable, it is not without its own set of delicate challenges. The research community must now figure a path through the tangled issues associated with drug development and regulatory approval. For interventions like TAMENDOX to truly benefit patients on a larger scale, several hurdles must be managed:
- Regulatory Scrutiny: New treatments require rigorous evaluation not only in clinical trials but also through regulatory bodies. Demonstrating safety and consistent efficacy is a must-have for any new drug addition.
- Cost and Accessibility: Personalized therapies, due to their tailored nature, can sometimes be more expensive. Ensuring that such treatments are accessible to all segments of society is a critical challenge.
- Physician Adoption: While early evidence may be promising, widespread acceptance by the medical community requires extensive education and training on how to integrate these new protocols within existing treatment frameworks.
The way forward is to encourage transparency in clinical data, foster collaborations between academic institutions and pharmaceutical companies, and maintain open lines of communication with patient advocacy groups. Addressing these points head-on is essential if we are to overcome the significant, though manageable, hurdles placed before us.
Reflecting on the Broader Movement Toward Personalized Medicine
The TAMENDOX study is not an isolated occurrence—it is part of a larger trend within modern healthcare that increasingly values patient-specific treatments over broad, undifferentiated approaches. This shift is emblematic of a broader movement that has the potential to revolutionize how we understand and treat diseases across the board.
Numerous factors are converging to drive this change:
- Advances in Genetic Testing: With the cost of sequencing becoming more accessible, physicians are now better equipped to identify genetic markers that predict drug metabolism efficiency and treatment response.
- Growing Clinical Data: Ongoing research continues to amass evidence that supports the superiority of personalized therapeutic approaches in enhancing treatment outcomes.
- Patient Empowerment: More patients are now informed about their own genetic profiles and are demanding treatment options that recognize their unique biological makeup.
- Technological Innovations: From data analytics to precision drug formulation, technology is rapidly transforming the ways in which personalized medicine can be delivered on a large scale.
This transformation is redefining what it means to treat a condition like breast cancer. No longer must patients settle for treatments that are based solely on broad categorizations. Instead, the proliferation of personalized options signifies a future where every patient’s therapy can be as unique as the genetic intricacies that define them.
Expert Opinions: Weighing the Pros and Cons
The innovative approach presented by the TAMENDOX study has sparked conversations among oncologists, pharmacologists, and healthcare policy experts alike. While the clinical results are impressive, there are still several nuanced issues that require deep reflection.
Here is a balanced look at the pros and areas needing further exploration:
- Advantages:
- Enhanced drug efficacy by ensuring sufficient levels of the active metabolite.
- Potential for reduced risk of breast cancer recurrence.
- A personalized approach that prioritizes individual patient needs.
- Comparable tolerability and safety profile to standard tamoxifen therapy.
- Considerations:
- Further research is necessary to validate long-term outcomes.
- Regulatory approval processes may present obstacles.
- Cost implications and accessibility for a broader patient population need to be addressed.
- The integration of genetic testing into routine clinical practice might require additional resources and training for healthcare providers.
When weighing these factors, it becomes clear that while TAMENDOX presents a significant technological leap, it exists within a broader clinical and economic landscape that is still adapting to the wide-scale implementation of personalized medicine.
Policy and the Future: Shaping the Next Chapter in Breast Cancer Treatment
Breast cancer treatment is on the cusp of a transformative era. With personalized medicine at the helm, there is a pressing need for policymakers, healthcare providers, and insurance companies to work together. This approach isn’t just about adopting a new drug—it’s about restructuring systems to better support individualized care.
The following steps could help usher in a future in which innovations like TAMENDOX become the norm rather than the exception:
- Streamlined Regulatory Pathways: Developing clear guidelines that allow for the rapid yet safe approval of personalized treatments will be a key factor in accelerating their availability.
- Insurance Coverage Innovations: Health insurers must adapt their policies to provide adequate coverage for genetic tests and individualized treatments so that patients do not bear prohibitive costs.
- Continued Clinical Research: Ongoing multicenter studies and post-market surveillance can help ensure that these therapies continue to meet the highest standards of efficacy and safety.
- Educational Initiatives: Equipping healthcare providers with the knowledge and tools needed to interpret genetic data and apply personalized protocols is essential for the successful integration of these new approaches into routine practice.
This multi-stakeholder approach is essential because the benefits of personalized therapy go far beyond improved clinical outcomes on paper. They represent a fundamental shift in how we conceptualize treatment success, making sure that every small distinction in a patient’s biology is recognized and catered to.
Challenges Ahead: Managing Your Way Through the Roadblocks
As promising as the TAMENDOX strategy appears, the journey ahead is riddled with its own set of intimidating challenges. There are several key areas where more work is needed to ensure that personalized hormone therapy reaches its full potential:
- Long-Term Outcome Data: While the early-phase study results are favorable, the long-term benefits compared to traditional tamoxifen therapy remain to be fully established through extended follow-up studies.
- Implementation in Diverse Settings: Clinical effectiveness in controlled study environments may differ from real-world scenarios. Therefore, it is important that future studies address how well these personalized approaches work across different healthcare settings and populations.
- Global Accessibility: Innovations in personalized medicine must eventually translate to diverse healthcare systems around the world. Efforts must be made to ensure that breakthroughs are not confined to high-resource countries alone.
- Cost-Benefit Analysis: Comprehensive analyses that weigh the increased cost of personalized treatments against the benefits of reduced recurrence rates and improved quality of life will be key to convincing decision-makers and payers.
These challenges, although complicated, are by no means insurmountable. They serve as a reminder that while the path to innovation is full of twists and turns, each step taken brings us closer to an era where medicine is as personalized and adaptive as the individuals it aims to treat.
A New Outlook on Breast Cancer Management
The TAMENDOX study has illuminated a promising path toward addressing a persistent problem in breast cancer management—namely, the uneven efficacy of tamoxifen due to individual metabolic differences. By supplementing the active metabolite directly, this new treatment approach not only levels the playing field but also hints at what the future of oncology might hold.
In summary, the key takeaways include:
- The recognition that genetic variability has a significant impact on tamoxifen’s effectiveness.
- The development of TAMENDOX as an innovative way to ensure patients receive the optimal therapeutic drug level.
- Strong clinical evidence supporting the efficacy and safety of combination therapy in achieving necessary drug concentrations.
- The potential for this personalized approach to offer critical treatment alternatives, especially for premenopausal women who have fewer options.
- An overarching movement toward personalized medicine that promises not only enhanced treatment outcomes but also a more patient-centric approach to healthcare.
As we look to the future, it becomes clear that personalized hormone therapy is not merely a fleeting trend, but a vital overhaul in the way we approach breast cancer treatment. It paves the way for a more adaptive, effective, and safe methodology that has the potential to dramatically improve the lives of countless women worldwide.
Conclusion: Steering Through the Future with Optimism
The journey of medical innovation is invariably marked by both breakthroughs and setbacks. The introduction of TAMENDOX represents a significant leap forward in addressing the subtle differences in drug metabolism that have long plagued traditional breast cancer treatment. By ensuring that each patient receives the active form of tamoxifen in the form that they need, this personalized approach is not only scientifically sound but also a practical step forward in personalized and precision medicine.
In our rapidly evolving medical landscape, tailoring treatments to the unique genetic makeup of each patient is no longer a futuristic concept but a present-day reality. As we take a closer look at therapies like TAMENDOX, we are reminded that progress in medicine is best achieved when innovation meets individualized care—bridging the gap between cutting-edge research and tangible clinical benefits. With continued research, collaboration, and adjusted policies to manage the challenges ahead, the future of breast cancer treatment promises to be brighter, more effective, and more humane.
This new approach might soon become a standard part of clinical practice, guiding physicians and patients alike as they steer through the maze of treatment options. In doing so, it reaffirms the immense potential that lies in personalized medicine—ensuring that every woman battling breast cancer receives a therapy that is as unique and individual as her own genetic fingerprint.
Ultimately, the promise of personalized hormone therapy is not merely about extending life but also about enhancing the quality of life. This advancement, supported by robust clinical research and a collaborative medical community, signifies a hopeful step forward in our collective battle against breast cancer. It compels us to celebrate innovation while remaining grounded in the many practical considerations of clinical implementation.
The dialogue between cutting-edge research and the practicalities of treatment protocols will continue to evolve, and each increment in progress offers us valuable lessons in the fine details of personalized care. For patients, clinicians, and researchers alike, these developments ignite a spark of optimism—a belief that by addressing the little details in drug metabolism, we can overcome the challenges that have long hindered the fight against cancer.
In conclusion, as we navigate through both the promising and sometimes overwhelming maze of breast cancer treatment options, the emergence of strategies like TAMENDOX offers not only hope but also a blueprint for future innovations. By directly tackling the problematic aspects of tamoxifen’s metabolic pathway head-on, the medical community embraces a more patient-centered future—one where every individual’s treatment is as unique as the challenges they face. This renewed focus on precision and personalization stands as a beacon for the next chapter in cancer care, suggesting that sometimes, the solution to a widespread problem lies in addressing the very small distinctions that make each patient different.
Originally Post From https://www.eurekalert.org/news-releases/1102148
Read more about this topic at
Tailored Tamoxifen Treatment for Breast Cancer Patients
Tailoring Adjuvant Endocrine Therapy for Premenopausal …