Digital Privacy and Healthcare: Balancing Cookies and Patient Trust
In today’s world of modern medicine and digital interaction, healthcare institutions are challenged to reconcile two seemingly disparate priorities: offering state-of-the-art treatment and safeguarding the patient’s digital footprint. As online healthcare portals routinely display cookie consent banners and privacy notices, it is important to remember that these web tools are as much about fostering patient trust as they are about data collection and analysis.
When you browse a reputable healthcare website, you might be greeted with a message explaining that cookies are used for running the site, improving your digital experience, and even tailoring personalized content. While the technical language behind these cookie disclosures might seem intimidating or even nerve-racking at first, their primary intent is to ensure that your online experience is smooth and secure.
Much like the complicated pieces in our body systems, the digital world of cookies is filled with twisted issues— from strictly necessary cookies that let you sign in or remember your navigation path, to performance cookies tracking which pages are visited the most. Although these processes might initially feel like a tangled web of confusing bits, they are essential in creating a seamless interaction between patients and their care providers.
Even for those who find these digital disclosures a bit off-putting, the reality remains that managing your cookie preferences is an act of empowerment, much like being proactive with one’s own health. By allowing patients to control their digital privacy, healthcare sites build trust and set the stage for a relationship that respects both personal data and personal health.
Predicting Breast Cancer’s Next Move: A New Era in Oncology
For decades, oncologists have been grappling with the tricky parts of breast cancer treatment – specifically, the challenge of a tumor’s ability to build resistance against targeted therapies. No longer are cancer specialists content to simply react after resistance develops; they are now making bold moves to predict ahead of time the pathways tumors might take.
Recent initiatives at leading cancer centers, such as Memorial Sloan Kettering Cancer Center (MSK), have sparked conversations about shifting the paradigm from a reactive stance to a proactive strategy. By leveraging cutting-edge technology including artificial intelligence (AI) and ultrasensitive liquid biopsies, researchers are taking a closer look at the subtle details that dictate cancer behavior.
Advanced Liquid Biopsy Techniques: Staying One Step Ahead
One of the most promising methods emerging in this new era of oncology is the liquid biopsy. These highly sensitive tests are designed to detect circulating tumor DNA (ctDNA) in the bloodstream – sometimes picking up just a few fragments among a million normal DNA pieces. To many, this might seem like delving into the nitty-gritty of molecular biology, but in truth it represents a game-changer for early detection of treatment resistance.
Liquid biopsies enable oncologists to catch the earliest signs of cancer cells beginning to resist treatment. Instead of waiting for a tumor to fully develop a resistance mechanism, physicians can now monitor small changes in a patient’s blood. This approach is akin to playing a strategic game of poker with cancer – trying to anticipate its next move before it fully unfolds. The potential benefits include not only better treatment selection but also the hope of preventing metastatic disease.
- Early detection of treatment-resistant cells
- Personalized therapy adjustments
- Improved patient outcomes through timely intervention
These advancements have garnered attention in the medical community as they promise a more targeted and timely response to the onset of cancer resistance. The use of liquid biopsy transforms the traditional reactive approach of waiting for treatment failure into one where cancer’s hidden moves can be intercepted early on.
Utilizing Artificial Intelligence in Breast Cancer Treatment
Another transformative tool in the fight against breast cancer is artificial intelligence. By incorporating AI, researchers are beginning to predict which patients are at higher risk of developing resistance to specific therapies. Through sophisticated machine-learning models that factor in both clinical data and tumor genomic features, the future of precision oncology is coming into sharper focus.
The integration of AI into clinical practice isn’t just about creating a high-tech solution for a tense, off-putting problem – it’s about harnessing modern computing power to sift through the fine points of patient data. By predicting outcomes for patients using CDK4/6 inhibitors in combination with hormone therapy, AI is helping to figure a path toward more effective and personalized treatment regimens.
Key benefits of AI in breast cancer treatment include:
- More accurate risk predictions for resistance
- Optimization of treatment regimens tailored to individual patients
- Potential reduction of unnecessary treatment side effects for lower-risk individuals
This proactive use of AI transforms medical interventions from being purely reactive to a strategy that anticipates the tumor’s behavior, thereby offering hope for improved overall survival rates and quality of life for patients struggling with breast cancer.
Learning from History: Landmark Discoveries in Breast Cancer Research
The journey to predict and intercept breast cancer resistance is not a sudden leap but rather a progression built upon years of groundbreaking research. The history of discoveries at MSK is a testament to persistent innovation and methodical investigation. By continuously tackling the tricky parts and subtle details of tumor behavior, researchers have established new protocols and treatment options that once seemed unattainable.
Consider the following timeline that illustrates key milestones in breast cancer research:
| Year | Discovery | Impact |
|---|---|---|
| 2013 | ESR1 gene mutations causing hormone therapy resistance | Laid the groundwork for targeted therapies like selective estrogen receptor degraders |
| 2018 | Genomic mapping of metastatic breast cancer | Enhanced understanding of tumor evolution and resistance strategies |
| 2020 | Liquid biopsy analysis identifying PTEN gene mutations | Improved ability to predict resistance to PI3K-targeting drugs |
| 2024–2025 | Use of AI to predict outcomes in HR-positive, HER2-negative breast cancer | Opened avenues for better-personalized treatment and early risk identification |
This timeline represents the evolution of breast cancer research – a journey replete with twists and turns, as oncologists and researchers piece together subtle details from each new study. With every new discovery, the approach to treatment shifts, increasingly favoring methods that dig into the early molecular changes before full resistance sets in.
Bridging the Laboratory and the Clinic: Translational Research and Real-World Impact
Translational research – the process of turning scientific discoveries into tangible treatments – is at the heart of modern oncology. In many ways, this work is akin to steering through a maze of complicated pieces and subtle details. Researchers must not only understand the basic science but also work closely with clinicians to bring lab innovations to the bedside.
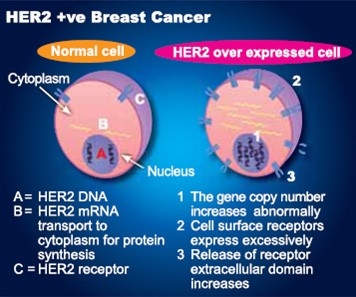
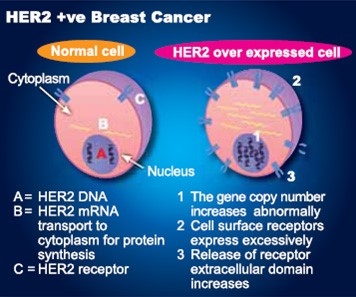
One powerful example is the development of the HERizon-Breast clinical trial. This trial aims to enroll patients with newly diagnosed HER2-positive metastatic breast cancer, employing a revolutionary liquid biopsy strategy. On one hand, this initiative represents a proactive step in cancer treatments; on the other, it exemplifies the collaborative spirit needed to translate lab breakthroughs into real-world therapeutic strategies.
What makes the HERizon-Breast trial so compelling is the refined approach to treatment – monitoring patients with both PET scans and next-generation blood tests. This method underscores the idea that understanding cancer’s subtle, hidden complexities can lead to early interventions that significantly improve patient outcomes.
Additionally, clinical trials are opening up new vistas for those fighting cancers previously considered incurable. By using FDA-approved drugs in novel combinations, researchers are aiming to intercept cancer resistance before it becomes an overwhelming challenge. Patients now have access to treatments that not only tackle the tumor directly but also prevent the cancer from evolving into a form that resists therapy entirely.
Collaboration: The Backbone of Modern Cancer Care
None of these advancements would be possible without the robust interdisciplinary collaborations among laboratory scientists, clinicians, and computational experts. In busy hospitals and research centers alike, the ability to find your way through the maze of small distinctions in molecular behavior is made simpler by teamwork. This kind of collaboration ensures that every new insight is rapidly transformed into improved treatment protocols.
Key areas where collaboration has provided breakthroughs include:
- Sharing data between labs and clinical practices
- Integrating AI-driven predictive models with patient treatment plans
- Designing clinical trials that incorporate both traditional and novel diagnostic tools
It is evident that when various experts join forces, even the tricky parts of cancer research – those that may seem filled with problems or completely on edge – can be managed effectively. The synergy between researchers and clinicians helps to ensure that each technological advancement directly benefits patients.
Dispelling Myths: Addressing Concerns and Uncertainties in Cancer Research
While these innovations herald a new era of proactive care, it is natural for the public to harbor concerns about the pace and direction of breast cancer research. Some might warn that using AI or ultra-sensitive diagnostics like liquid biopsies could lead to overtesting or overtreatment. However, a careful look at the evidence suggests that these methods actually refine treatment selection rather than simply increasing intervention unnecessarily.
One key consideration is that while predictive tools may seem intimidating at first, they operate on a principle of early detection – catching the first stirrings of a tumor’s resistance rather than waiting for full-blown therapy failure. In many respects, this proactive mindset is as essential as it is revolutionary. It not only allows for tailored treatment plans built on real-time molecular insights but also helps to reduce the caveats of blanket treatment strategies that might otherwise lead to unnecessary side effects.
For patients and their families, this means that the use of AI and liquid biopsy does not translate into additional risk or extra hassle. Rather, it provides a refined, patient-specific approach designed to keep treatment as effective as possible while sparing individuals the nerve-racking experience of treatment failure and subsequent adjustments.
Addressing the Hidden Complexities of Cancer Treatment Resistance
Even as these innovations generate enthusiasm, oncologists remain mindful of the subtle details and hidden complexities that characterize cancer’s behavior. For instance, resistance mechanisms are not uniform – they vary widely from patient to patient, and even within the same tumor over time. Understanding these little twists and tangled issues requires both state-of-the-art technology and a pragmatic look at the overall treatment plan.
The strategy of monitoring tumor DNA over time is an example of how the field is managing its way through the labyrinth of cancer’s evolutionary process. By taking multiple samples at different phases, researchers can piece together a chronological narrative of how a tumor adapts. This methodical approach ensures that treatment adjustments are based not on educated guesses but on quantifiable, evolving molecular data.
Watching these fine shades of change play out at the molecular level enables oncologists to refine how they use current therapies. The ultimate goal is not to provide an unnecessary treatment for every mutation detected, but rather to pinpoint which adaptations are truly pushing the tumor onto a resistant pathway. This precision is key. The process is not without its challenges, as the nuances involved are both complicated and, at times, overwhelming. Yet, each insight—no matter how minute—brings the medical community one step closer to a future where cancer management is as targeted as it is effective.
Personalized Therapy in a High-Tech Era: Future Perspectives for Breast Cancer Care
The convergence of precision diagnostics, artificial intelligence, and personalized therapy heralds a pivotal moment in breast cancer care. As oncologists move from a one-size-fits-all model to a more nuanced approach, the ability to fine-tune treatments based on an individual’s unique tumor profile is becoming increasingly critical. This shift represents more than just an evolution in treatment protocols—it symbolizes a fundamental transformation in how we think about cancer care.
In this evolving landscape, every patient is seen as a unique case with their own set of challenges. Rather than facing a standard protocol, they benefit from a treatment plan that takes into account both the overarching aspects of their disease and the specific molecular markers that define it. By leveraging innovative strategies such as AI-powered predictive models and liquid biopsies, oncologists are beginning to get into the fine points of personalized treatment in a way that was simply not possible a few years ago.
Some of the success stories emerging from clinical trials are already inspiring confidence within the medical community. Consider, for example, the strategic use of FDA-approved drugs in new combinations to preempt drug resistance. Under the HERizon-Breast trial, patients with HER2-positive metastatic breast cancer are being closely monitored with imaging scans and molecular blood tests. This ongoing analysis is designed to catch even the tiniest resistance markers early—allowing for immediate adjustments in therapy that can be truly life-saving.
The broader implication here is that both doctors and patients now have greater clarity and more options than ever before. This approach reduces the risk of unnecessary side effects while simultaneously enhancing the effectiveness of treatments. It epitomizes a future where every patient’s journey through cancer care is optimized according to individualized, data-driven insights. In this way, technology and human compassion come together to form a powerful alliance against one of medicine’s most challenging foes.
The Role of Patient Education in Embracing New Technologies
As the landscape of breast cancer treatment continues to evolve, patient education becomes a critical element in ensuring the success of these new technologies. It is essential that patients are not left in the dark about how tools like AI and liquid biopsies work, nor are they overwhelmed by the myriad digital interactions that characterize modern healthcare platforms.
Clear, accessible communication helps demystify the process. Educational resources that explain the role of cookies on healthcare websites, as well as the ways in which digital data is used to streamline patient care, can serve as an effective bridge between technological innovation and everyday usage. By offering transparent information, healthcare providers empower patients to take an active role in their treatment journey—ensuring that advanced tools are seen not as a source of anxiety, but rather as key components in a personalized, effective care strategy.
Some suggested ways to increase patient engagement include:
- Detailed patient brochures and online FAQs focused on new diagnostic tools
- Interactive webinars hosted by leading researchers and clinicians
- Personalized counseling sessions to address digital privacy and treatment details
When patients are well-informed, they are better able to make confident decisions regarding their care. This improved understanding reduces the nerve-racking sense of uncertainty that can accompany a cancer diagnosis and replaces it with a proactive, hopeful outlook.
Interdisciplinary Approaches: Integrative Medicine Meets High-Tech Cancer Research
It is equally important to acknowledge that the future of cancer treatment is not limited to high-tech interventions alone. Many experts advocate for an integrative approach that combines modern cancer therapies with alternative medicine and nutritional strategies. This holistic perspective is designed to manage the patient’s overall well-being while addressing the specific challenges of the disease.
In practice, the integration of conventional oncology with supportive therapies can help patients handle the overwhelming physical and emotional toll of a cancer diagnosis. For instance, while innovative treatments like targeted drugs, AI predictions, and liquid biopsies are crucial for managing the tumor itself, integrative medicine focuses on enhancing quality of life through nutritional guidance, stress management, and complementary therapies.
This comprehensive approach allows oncologists to steer through the maze of treatment decisions with a more rounded perspective – one that recognizes that battling cancer is not only about eradicating malignant cells but also about supporting the patient’s overall health. In effect, personalized therapy is broadened to include lifestyle adjustments and integrative care that address the whole person, not just the disease.
Key components of this approach include:
- Holistic nutrition counseling tailored to bolster immune function
- Mind-body therapies such as meditation and yoga to reduce stress
- Alternative treatments that complement conventional oncology protocols
By fusing the precision of modern medicine with the gentle support of integrative therapies, healthcare providers can create treatment plans that are not only effective but also nurturing. This multidimensional strategy offers patients hope and resilience, ensuring that every aspect of their care is thoughtfully addressed.
Empowering Patients Amid the Tense Journey of Cancer Treatment
As we reflect on the evolving landscape of breast cancer care, it becomes clear that the role of the patient is more important than ever. Empowerment through education, digital transparency, and personalized treatment approaches is becoming a cornerstone of modern healthcare. Rather than facing the challenge of cancer as an isolated battle, patients today are invited to join a community of experts, researchers, and caregivers dedicated to finding innovative solutions.
This sense of empowerment can ease the intimidating and sometimes overwhelming experience of navigating cancer treatment. When patients understand how technologies like liquid biopsy and AI are used to anticipate and prevent treatment resistance, they move from feeling at the mercy of a mysterious disease to feeling actively involved in steering their own care.
Empowerment also comes from knowing that the potential setbacks in treatment are not a dead end but rather an opportunity to refine and adjust the treatment strategy. Every nuanced detail and every small distinction in a tumor’s genetic makeup provides another clue for tailoring the most productive course of action. This approach champions patient agency, making the daunting process of treatment management a collaborative effort between the patient and the healthcare team.
Conclusion: A Future Shaped by Proactive, Personalized Care
The strides being made in breast cancer research represent more than just technological and clinical advancements; they mark a fundamental shift in how we understand, prevent, and treat one of today’s most challenging diseases. As innovations in AI, liquid biopsy, and integrative medicine continue to converge, the focus is shifting from merely reacting to cancer’s attacks to anticipating its moves and intercepting them at every step.
With each new study, each clinical trial, and every collaborative effort between researchers and clinicians, we are learning to manage even the trickiest parts of cancer treatment. Although there are still plenty of tangled issues and confusing bits to resolve, the journey thus far illustrates that overcoming resistance in breast cancer is not an insurmountable task.
As patients and healthcare providers alike adjust to this high-tech, personalized paradigm, it is important to remember that every digital interaction—from managing online cookie preferences to tracking nuanced tumor mutations—is designed with the patient’s best interests in mind. The future of cancer care is not only about advanced treatments and predictive models; it is about fostering an environment of trust, empowerment, and proactive well-being.
In summary, the evolution of breast cancer treatment underscores the need for a proactive approach that leverages every available tool—from high-precision diagnostics to integrative wellness practices—to stay one step ahead of the disease. As we move further into this new era of oncology, the commitment to innovative, personalized care remains the most promising avenue toward truly ending cancer for life.
It is our hope that as these technologies mature and become more widely adopted, every patient will have the opportunity to benefit from a tailored treatment plan that not only confronts the disease head-on but also supports their overall well-being. With each breakthrough, we are steadily working our way through the nerve-racking and off-putting challenges of cancer treatment, paving the way for a future where every patient can feel secure, informed, and empowered.
Ultimately, the story of modern oncological research is one of resilience, collaboration, and relentless innovation. By embracing advanced diagnostic tools, patient-centric digital interactions, and personalized treatment strategies, we are creating a healthcare environment where the ability to predict and prevent cancer resistance is no longer a distant dream, but an actionable reality. The journey is long and sometimes filled with complicated pieces, but every step brings us closer to a world where cancer is not just managed – it is cured.
Originally Post From https://www.mskcc.org/news/latest-research-into-overcoming-resistance-to-breast-cancer-targeted-therapies
Read more about this topic at
The path to least resistance – Cancer News
Latest Research Into Overcoming Resistance to Breast …