Innovative Cancer Pain Management Strategies in Modern Oncology
In recent years, the treatment of cancer pain has become an essential, yet often overlooked, pillar of comprehensive oncology care. With treatment advances leading to longer survival rates, an increasing number of patients now face the tricky parts and tangled issues associated with bone metastases and treatment-related pain. A newer initiative—a multidisciplinary tumor board focused on cancer pain—is challenging traditional treatment approaches by prioritizing pain management with the same urgency as addressing the underlying cancer. This opinion editorial explores how innovative strategies, collaborative teamwork, and a patient-centered approach can transform the way we handle one of oncology’s more confusing bits.
Although pain has always been an issue for cancer patients, the emerging reality is that pain is not just a side effect of cancer—it is a critical component that can affect every aspect of a patient’s quality of life. As patients live longer because of breakthroughs in cancer therapies, the nerve-racking problem of pain management, particularly in cases involving bone metastases, has become a super important focus. This novel tumor board initiative, launched at University of Miami’s Sylvester Comprehensive Cancer Center, represents a groundbreaking strategy to treat cancer pain aggressively and strategically, ensuring that patients do not have to figure a path between cancer treatment and pain relief.
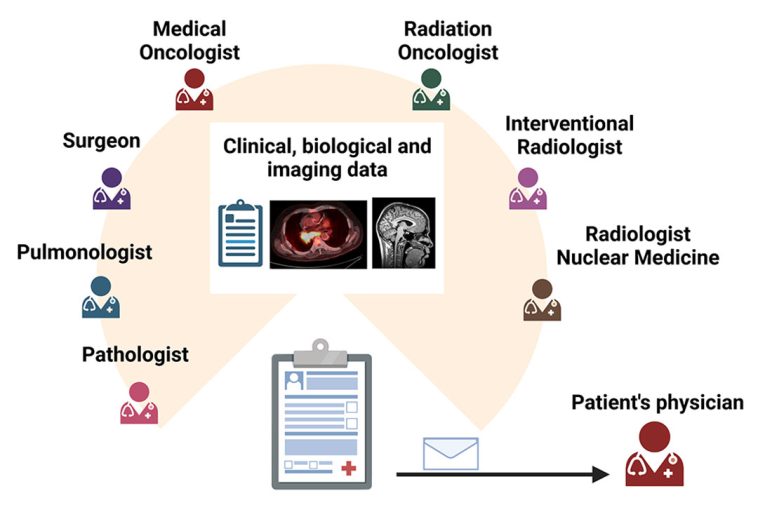
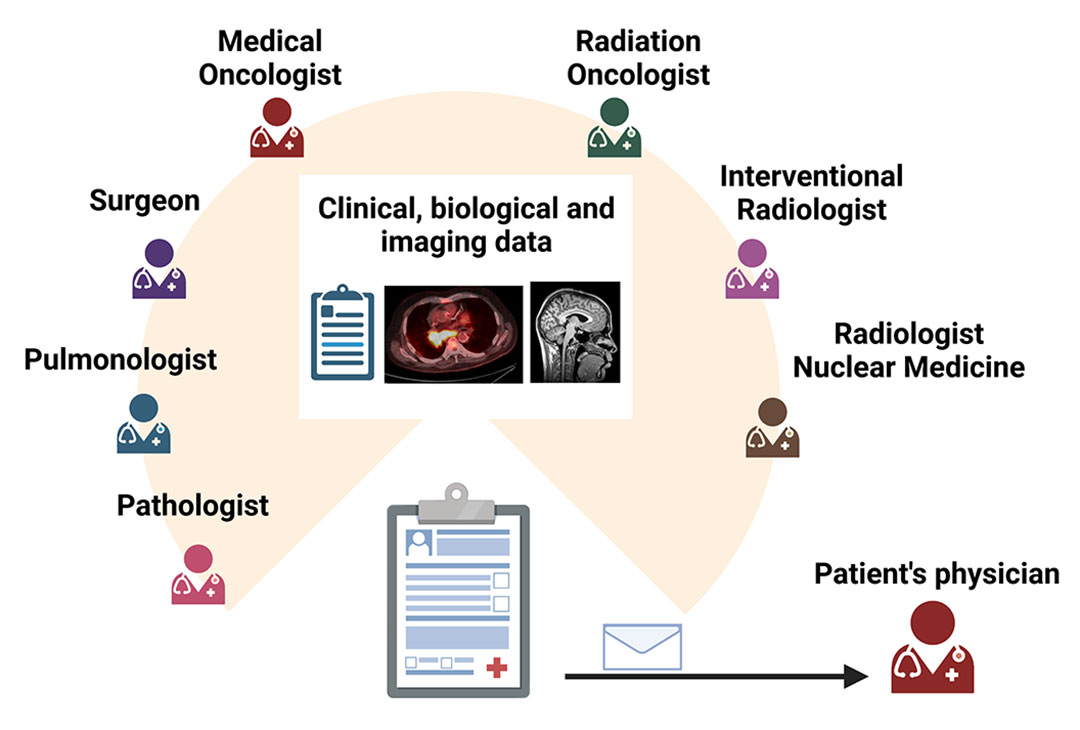
Collaborative Teamwork: A Multidisciplinary Approach to Pain Relief
At the heart of this pioneering initiative is the idea that no single specialty has all the answers when it comes to managing pain in cancer patients. Instead, a diverse group of experts has come together to work through the challenging twists and turns that come with cancer pain management. With specialists in medical oncology, radiation oncology, palliative care, anesthesia, pain medicine, orthopedic surgery, and neurosurgery pooling their insights, the board creates individualized pain management strategies that go well beyond the standard tumor board discussions.
Bridging the Gap Between Cancer Treatment and Pain Management
One of the most significant achievements of this multidisciplinary board is its ability to bridge the gap between aggressive cancer treatment and effective pain management. Traditionally, cancer-focused tumor boards have concentrated on the disease itself, often leaving the confusing bits of pain management to be handled separately or even neglected. This new approach ensures that both the cancer and the pain are treated concurrently, thereby reducing the use of heavy opioids and minimizing potential side effects.
According to experts like Dr. Alan Alper Sag, an associate professor of interventional radiology, the board’s initiative was born from everyday observations and hallway conversations among various specialists. “What if the disease was pain?” Dr. Sag asks. This seemingly simple question prompted a radical shift in perspective: to consider cancer pain as a standalone problem that requires its own dedicated strategy. This approach is not only more holistic but also provides a direct pathway to reducing opioid escalations and enhancing patients’ overall well-being.
Key Benefits of a Multidisciplinary Strategy
There are several reasons why a multidisciplinary approach to cancer pain management is a game-changer:
- Improved Quality of Life: Patients receive targeted pain relief methods that allow them to enjoy a better day-to-day experience while undergoing demanding cancer treatments.
- Reduced Opioid Dependency: By integrating opioid-sparing strategies and alternative pain relief measures, the board helps mitigate the nerve-racking side effects associated with high opioid doses.
- Enhanced Communication and Education: Bringing together professionals from diverse medical backgrounds fosters an environment rich in dialogue where fine details and subtle differences in treatment approaches are openly discussed and optimized.
- Accelerated Decision-Making: The board’s focus on immediate pain management planning helps to cut down the nerve-wracking delays that usually burden the decision-making process in cancer care.
Opioid-Sparing Solutions and Alternative Therapies in Cancer Pain
Cancer-related pain management has long relied on opioids, often in high doses, to offer relief. However, opioids themselves come with a host of intimidating side effects: drowsiness, nausea, constipation, and even depression or delirium can significantly impact a patient’s quality of life. In an era where patients are living longer and experiencing more treatment-related issues, relying solely on opioids is a strategy loaded with problems.
Exploring Alternative Methods for Pain Relief
In this context, many care providers and experts are beginning to take a closer look at multimodal analgesia and other image-guided interventions. Techniques such as nerve blocks, neuromodulators, and carefully administered radiation treatments represent promising alternatives that may offer immediate and long-lasting relief. These approaches can provide a tailored solution that suits an individual patient’s needs without the overwhelming reliance on opioids.
For instance, one case discussed by Dr. Sag involved a young man with metastatic colon cancer suffering from severe pelvic pain, which traditional treatments had failed to alleviate. Instead of further increasing opioid doses—a solution that only exacerbated side effects—the board explored a focal outpatient CT-guided nerve block and ablation. The success was immediate and striking, as the patient experienced complete relief during the procedure. Such cases underscore the potential benefits of stepping away from the classic opioid-centric methods and adopting a broader approach that integrates various techniques.
Advantages of Non-Opioid Strategies
The advantages of non-opioid pain management methods extend well beyond immediate pain relief. Some of the key benefits include:
- Immediate Feedback During Interventions: Procedures like nerve blocks allow patients to experience pain relief even as the treatment is underway, providing reassuring and immediate positive feedback.
- Long-Term Quality of Life Improvements: With reduced exposure to high opioid doses, patients face fewer side effects and are more likely to maintain a stable quality of life even as they continue with their cancer treatment.
- Customized Pain Management Plans: By considering the unique history, imaging, and prior treatment responses of each patient, the multidisciplinary team can craft well-informed, individualized care plans.
Below is a table summarizing the comparison between traditional opioid-based management and non-opioid alternatives:
| Aspect | Traditional Opioid-Based Approach | Non-Opioid Alternatives |
|---|---|---|
| Pain Relief Onset | Often delayed; requires dose titration | Can be immediate (e.g., nerve blocks) |
| Side Effects | High risk of drowsiness, nausea, and more | Fewer systemic side effects |
| Quality of Life | Pain may persist despite high doses | Better daily functioning and comfort |
| Long-Term Outcomes | Potential for opioid dependency | Opioid-sparing strategies reduce dependency risks |
Personalized Care: Integrating Patient Histories and Imaging Data
An essential strength of the tumor board model focused on cancer pain is its emphasis on personalization. By combining detailed patient histories with advanced imaging data, the board members are able to figure a path that is tailored specifically to each patient’s issue. This means that even in cases of treatment-resistant pain, the medical team can count on a collaborative effort to pick through the mixed signals and confusing bits that have traditionally hindered effective pain management.
Importance of Multidisciplinary Communication
The educational and communicative aspects of the board are among its greatest assets. The open, hallway-like conversations where specialists from different fields share insights can help illuminate small distinctions that might otherwise be missed. These fine shades of clinical details—once relegated to separate specialist realms—are brought together in a single forum, allowing the team to work through tricky parts and make well-rounded decisions that have a positive impact on overall patient care.
One striking example involves cases where the board analyzed imaging results alongside a patient’s treatment history. By reviewing the images, specialists identified that further radiation or surgery was not always a viable option, particularly if the maximum radiation dose had already been administered or if the patient had exhausted available chemotherapy regimens. Instead, the board could consider alternative pain management options, such as image-guided injections or nerve stimulator placements that target the pain at its source.
Case Studies Demonstrating Impact
Over the past several months, the tumor board has addressed approximately 40 patient cases, ranging from those with bone pain to those suffering from visceral discomfort. One memorable case concerned a patient with treatment-resistant cancer in the head and neck region. Here, a coordinated strategy involving oral and maxillofacial surgeons, otolaryngologists, and radiation oncologists led to a tailored plan that successfully reduced the patient’s pain levels while keeping the patient’s ongoing cancer treatment on track.
This case underscores the board’s philosophy: in many instances, even if one cannot treat the cancer directly, treating the pain can provide a big win for the patient. When patients know that an entire team dedicated itself to understanding and managing their pain, the relief isn’t just physical—there’s also a profound boost in their emotional and psychological well-being.
Patient-Centered Outcomes: Quality of Life and Beyond
At its core, the tumor board’s initiative is about more than just medical intervention—it is about ensuring that patients enjoy a better quality of life. Cancer pain can be both physically debilitating and emotionally overwhelming. When pain is allowed to persist, patients often feel as though they are caught in a never-ending cycle, unable to engage fully with life or even with the treatment that could save them.
Empowering Patients Through Collaborative Care
Patients have expressed immense gratitude when they learn that a dedicated, multidisciplinary team is actively discussing their case to provide the best possible pain management strategy. Knowing that experts are coming together to figure a path through their tangled issues can be tremendously uplifting. The nerve-racking anticipation of a pain crisis can be greatly reduced when patients are provided with clear, well-organized treatment plans that balance cancer care with the need for effective pain relief.
By prioritizing quality of life, the board has effectively underscored the importance of treating the whole patient—body and mind. This patient-centered focus is especially critical in advanced cancer care, where every little twist or complicated piece of relief matters. It also fosters better overall patient engagement, as patients who feel supported are more likely to be proactive in managing their symptoms and adhering to their treatment plans.
User-Friendly Communication and Support
Alongside forming a comprehensive treatment strategy, the board is also committed to educating both providers and patients about the options available. By using plain language and avoiding overly technical jargon, the group assures that even the most intimidating aspects of cancer pain management are made accessible and understandable. Whether it’s discussing the fine points of interventional radiology or the subtle parts of multimodal pain therapy, the team’s dialogue is characterized by openness and a willingness to dig into every detail.
To better communicate these strategies with patients, many institutions have started providing detailed guides and flow charts outlining the available treatment options. These visual aids help patients and their families to get a clearer picture of how each option might impact their pain and quality of life.
Implementing a Modern Template for Pain-Focused Tumor Boards
The approach taken by the University of Miami is not isolated. Similar efforts at esteemed institutions like Brown University and Emory University have shown promising results. What sets these boards apart is their commitment to creating a modern template that other centers can use to construct their own pain-focused tumor boards. This template involves several key components:
- Core Team Formation: Assemble a committed group of specialists who are enthusiastic about addressing cancer pain head-on.
- Inclusive Case Submission: Open up case discussions to providers across different inpatient and outpatient settings to capture a wide range of patient experiences.
- Data-Driven Discussions: Incorporate patient imaging, treatment history, and current symptoms into every discussion.
- Guideline Integration: Align with established guidelines such as those from the National Comprehensive Cancer Network (NCCN) to ensure that care plans are evidence-based.
Below is an example of a simplified workflow that many institutions can follow when creating their own pain-focused tumor board:
| Step | Actions |
|---|---|
| Case Referral | Physicians from various departments submit cases that involve persistent pain during cancer treatment. |
| Data Collection | Gather patient history, imaging results, and current treatments. |
| Multidisciplinary Meeting | Specialists review the case and consider all possible interventions. |
| Plan Development | Create a patient-specific strategy combining multiple treatment modalities. |
| Implementation & Follow-Up | Apply the treatment plan and monitor patient outcomes, adjusting as needed. |
Steps for Institutions to Get Started
For institutions interested in initiating a similar program, the following steps can help steer through the process:
- Identify Unmet Needs: Begin by organizing internal discussions to identify which aspects of cancer pain management are most challenging within your patient population.
- Review Best Practices: Examine the NCCN guidelines on adult cancer pain and study the experiences of pioneering institutions.
- Build the Team: Recruit specialists from as many relevant disciplines as possible, starting with a core group of dedicated individuals.
- Establish a Clear Process: Define submission protocols for cases and set a regular meeting schedule for the tumor board.
- Foster Open Communication: Ensure that every decision is well documented and that all team members remain open to sharing insights and learning from each case.
The Broader Implications for Cancer Care
The emergence of pain-focused tumor boards represents a significant shift in how we approach cancer care. It pushes us to reconsider traditional methods by emphasizing a well-rounded treatment model that values pain management as much as direct cancer therapy. This integrated strategy is particularly important in today’s healthcare environment, where the treatment landscape is full of tricky parts and subtle differences among patient experiences.
Impacts on Healthcare Systems
Implementing a multidisciplinary pain management strategy has broad implications:
- Shortened Hospital Stays: Effective outpatient pain management can reduce the likelihood of hospital admissions due to pain crises, thereby easing the burden on healthcare facilities.
- Cost-Effectiveness: By reducing opioid use and preventing complications, healthcare systems may see improved cost management.
- Enhanced Provider Satisfaction: Physicians and specialists benefit from a cohesive environment where they are able to share insights and learn from each other, reducing the isolation that might come from working within siloed specialties.
- Improved Patient Outcomes: Ultimately, the integrated approach not only alleviates pain but also supports continuous cancer treatment, which is essential for long-term survival and health maintenance.
These impacts highlight how a modern, patient-centric treatment model can serve as a blueprint for changing the broader practice of oncology. By treating pain with the same urgency and precision as cancer itself, we create a model of care that truly addresses the holistic needs of patients.
A Call to Action for Health Practitioners
For practitioners across the oncology spectrum, the message is clear: it is time to take a closer look at how pain is managed in patients with cancer. Whether you are a medical oncologist, a radiologist, a surgeon, or a palliative care specialist, consider the possibility of collaborating with colleagues who may not traditionally be involved in your tumor boards.
Discuss these ideas at departmental meetings, reach out to analogous groups at other institutions, and most importantly, take a proactive role in crafting a strategy that puts the patient first. The goal is to replace off-putting delays and nerve-racking decisions with a system that is responsive, innovative, and above all, compassionate.
Lessons Learned and Future Directions
As institutions continue to implement these tumor boards, there are several lessons we can extract from early experiences:
- Sustained Collaboration Is Key: Continuous, open communication among specialists is crucial for refining pain management strategies and ensuring that treatment plans remain adaptable over time.
- Flexibility in Approach: Recognizing that every patient’s case comes with its own set of little twists, an adaptable strategy that evolves with emerging evidence and patient feedback is essential.
- Emphasis on Education: Educating both healthcare providers and patients on the available pain management options is a must-have component for successful implementation. This helps dispel fears and builds confidence in the collective expertise of the care team.
- Data-Driven Decisions: Leveraging patient data—from imaging studies to treatment histories—allows for a tailored approach that is both evidence-based and highly personalized.
Looking forward, the model of a pain-focused tumor board is likely to expand. As more institutions adopt these strategies, we can expect to see shared insights, collaborative research, and an even greater emphasis on reducing the tricky parts and tangled issues associated with managing cancer pain. The move towards integrating alternative pain management techniques, in combination with established treatments, promises to break new ground in oncology care.
Potential Challenges Ahead
Despite its promise, the model is not without its challenges. Some of the intimidating obstacles include:
- Resource Allocation: Implementing a multidisciplinary board requires dedicated time and human resources, which can be a stretch for smaller institutions.
- Cultural Shifts: Shifting from traditional, cancer-centric tumor boards to inclusive, pain-focused discussions may be off-putting for some specialists who are used to established protocols.
- Consistency in Guidelines: Aligning on treatment guidelines across different specialties can sometimes be complicated by slight differences in perspective and clinical experience.
These challenges, however, are not insurmountable. With strong leadership and a commitment to the shared goal of improved patient care, institutions can work through these nerve-racking issues. The key is to stay focused on the end goal: enhancing quality of life for patients battling both cancer and its associated pain.
Integrating Alternative Medicine and Nutrition in Cancer Pain Management
An additional layer to the comprehensive approach toward managing cancer pain involves exploring alternative medicine and nutritional strategies. In many cases, patients benefit from a well-rounded treatment strategy that includes not only medical interventions but also complementary approaches that help address the body’s overall response to pain and stress.
Complementary Therapies and Their Role
Alternative medicine techniques such as acupuncture, mindfulness meditation, and yoga have been increasingly recognized as useful adjuncts in managing chronic pain. These methods are not intended to replace conventional treatments but rather to provide additional support. They offer solutions for the confusing bits and little details that conventional treatments might overlook, particularly when traditional pain management strategies are running on empty.
For example, acupuncture has been shown to stimulate nerves and muscles, potentially altering pain signals to the brain, while mindfulness meditation and yoga can reduce stress hormone levels, thereby helping patients cope with the psychological burden of pain. Included in a comprehensive pain management plan, these alternative methods may play a pivotal role in soothing both the body and mind.
Nutrition’s Part in Alleviating Pain
Nutrition is another super important element that is sometimes left out of the standard oncology discussion but can have significant effects on pain and inflammation. Diets rich in anti-inflammatory foods, balanced with essential vitamins and minerals, may reduce systemic inflammation and help control pain levels. Nutritional interventions can synergize with standard treatments, lessening the overwhelming side effects of high-dose therapies and supporting overall health.
Key nutritional strategies include:
- Emphasizing Whole Foods: Fresh fruits, vegetables, whole grains, and lean proteins provide the nutrients needed for recovery and reduce inflammation.
- Omega-3 Fatty Acids: Found in fatty fish, flaxseeds, and walnuts, omega-3s have been shown to have potent anti-inflammatory properties.
- Antioxidants: Foods high in antioxidants, such as berries, dark leafy greens, and nuts, can help protect cells from damage, potentially reducing pain.
- Hydration and Electrolytes: Maintaining adequate hydration levels is essential to keep the body’s systems functioning smoothly, which may, in turn, alleviate pain symptoms.
Integrating nutritional guidance into the overall patient management plan helps address not just the immediate pain but also the underlying factors that might be contributing to it. This holistic view of patient care is reflective of the modern template being developed by pain-focused tumor boards.
Fostering a Culture of Continuous Improvement
One of the most exciting aspects of this new approach is its inherent adaptability. Each case reviewed by the tumor board presents an opportunity for the medical team to learn, adjust, and refine treatment protocols. Over time, this iterative process is likely to result in the discovery of even more effective pain management strategies that can be shared across the broader healthcare community.
Ongoing Education and Feedback
The board’s format encourages a feedback loop where every discussion helps refine best practices. Regular meetings, the sharing of success stories, and discussions of cases that pose particularly confusing bits all contribute to a dynamic learning environment. As clinicians continue to compare notes at national conferences and through interdisciplinary collaborations, the collective expertise grows, laying the foundation for future innovations in pain management.
This ongoing education is a key component of ensuring that the latest research, technological advances, and clinical insights are integrated into care plans. It is a process that not only enhances patient outcomes but also builds professional confidence among the specialists involved—a crucial factor when tackling nerve-wracking problems in a high-stakes environment such as cancer treatment.
Measuring Success: Metrics and Outcomes
Effective management of cancer pain through a multidisciplinary approach is not simply about individual anecdotes; it requires robust data collection and the analysis of patient outcomes. Metrics such as the following are essential:
- Pain Reduction Scores: Standardized pain assessment tools can help quantify improvements in patient pain levels over time.
- Opioid Consumption: Tracking opioid usage before and after implementing alternative strategies can provide clear evidence of the benefits of these approaches.
- Patient Satisfaction: Surveys and interviews with patients provide insights into how well the pain management strategies are working from a quality-of-life standpoint.
- Hospital Admission Rates: A decrease in pain-related hospital admissions can serve as a practical measure of success for outpatient pain management protocols.
Institutions that adopt these metrics will have a clearer picture of what works best, allowing them to adjust guidelines and share successful protocols with the wider community. Over time, the adoption of such measures may help standardize the approach to cancer pain management across multiple healthcare networks.
Conclusion: A Patient-First Approach for the Future of Oncology
In conclusion, the innovative initiative of a dedicated pain-focused tumor board represents a significant leap forward in how we manage one of the most challenging and nerve-racking aspects of cancer treatment. By tackling the overwhelming problem of cancer pain head-on with a multidisciplinary team approach, healthcare providers are not only ensuring continuity of cancer care but also significantly improving patient quality of life.
This integrated strategy emphasizes the importance of personalized care, teamwork across various specialties, and the incorporation of alternative therapies and nutritional guidance. Each of these elements plays a critical role in transforming the treatment landscape, enabling physicians to work through the small distinctions, subtle parts, and complicated pieces of cancer pain management in a way that is both comprehensive and compassionate.
For healthcare institutions ready to chart this new course, the message is clear: begin with a core group of dedicated professionals, foster a culture of continuous learning and collaboration, and prioritize patient well-being above all else. The steps may involve navigating through tricky parts and untangling complex issues, but the rewards—a better quality of life for patients and a more cohesive, informed care team—are well worth the effort.
As we move forward, the hope is that this modern template for addressing cancer pain will inspire further research, innovation, and widespread adoption. With each new case discussed, every patient who experiences relief, and every team member empowered by shared knowledge, we edge closer to a future where cancer treatment is not only about fighting the disease but also about ensuring that every patient can live as comfortably and fully as possible.
Ultimately, the success of such initiatives will depend on our collective commitment to putting patients first. When an entire team of specialists comes together, not just to treat cancer but to manage its quiet, persistent companion—pain—the impact goes far beyond clinical outcomes. It fosters a sense of hope, trust, and resilience that is invaluable in the journey through cancer care.
This collaborative approach, with its focus on clear communication, constant feedback, and integrated care planning, serves as a powerful reminder that the small distinctions can make all the difference. And as more institutions adopt this proactive model, the legacy of these pioneering efforts will be seen in the improved lives of countless patients—proof that sometimes, the best treatment is one that treats the whole person, not just the disease.
Originally Post From https://www.healio.com/news/hematology-oncology/20251022/tumor-board-aims-to-treat-cancer-pain-with-same-urgency-as-the-malignancy
Read more about this topic at
The Multidisciplinary Team in Pain Management
Multidisciplinary pain management program (MPP)