Chronic Hepatitis C and Pancreatic Cancer: Uncovering the Hidden Links
The debate about the tricky parts of modern medicine never seems to rest. Recent research has thrown a spotlight on chronic hepatitis C (HCV) and its connection to pancreatic ductal adenocarcinoma (PDAC). While this study looked specifically at a large group of U.S. veterans, it opens up a broader conversation about the hidden complexities behind virus-induced cancer risks and the unique challenges faced by specific patient populations.
In this opinion editorial, we take a closer look at the study’s findings, highlight how the risk factors interact, and explore potential future directions in the screening and treatment of HCV and pancreatic cancer. We also consider the implications these results may have on early detection models and healthcare strategies. Let’s dive in and figure a path through these complicated pieces, particularly in relation to veterans’ healthcare and general populations alike.
Understanding the Relationship Between Chronic HCV and Pancreatic Cancer
The study in question assessed over six million veterans tested for hepatitis C, comparing rates of PDAC among those with chronic HCV, patients who had been exposed to HCV, and those without any infection. A key observation was that chronic HCV infection was associated with a significantly higher risk of developing PDAC even after adjusting for well-known risk factors such as smoking, alcohol intake, diabetes, pancreatitis, and known liver disease.
The researchers reported an adjusted hazard ratio of 1.76 for chronic HCV and 1.18 for HCV exposure. When diving into the specifics, the risk varied by viral genotype. For instance, genotype 3 showed a notably greater adjusted risk compared with other genotypes, suggesting that the particular fine points of the virus characteristics may play a critical role in determining cancer risk. This finding indicates the importance of looking into the small distinctions within HCV infection when making healthcare policy or clinical decisions.
Exploring the Unique Risks in the Veteran Population
It is important to acknowledge that the veteran group studied has its own set of unique and tangled issues. Compared with the broader population, U.S. veterans might exhibit different patterns due to lifestyle choices, environmental exposures, and even genetic predispositions. These factors all contribute to an environment that is on edge, making healthcare strategies tailored for veterans especially crucial.
To better understand these risks, consider the following bullet list outlining some of the key characteristics of the veteran group:
- Predominantly Male Demographic: The veteran study group was over 90% male, a factor that may influence disease prevalence and progression.
- Age Profile: The median age for the cohort was 61.6 years, which could affect both the likelihood of HCV and the risk of developing PDAC.
- Ethnic Variations: About 65% of the participants were white, and close to 17% were Black, highlighting the importance of considering ethnic background when examining disease risk and outcomes.
- Exposure History: Many veterans have a unique history of exposures, including environmental and occupational hazards, that might interact with viral infections in unexpected ways.
These points are a reminder that while the study’s numbers do raise concerns, the underlying factors that drive these trends are complex. In other words, the association between chronic HCV and pancreatic cancer is layered with multiple intertwined risk elements that require further exploration.
Implications for Early Detection and Screening Strategies
One of the key takeaways from this research is the potential to refine early detection models for pancreatic cancer by incorporating HCV status, particularly among untreated patients. Early detection of PDAC is challenging because the disease is often diagnosed in its most advanced stages, when treatment options are limited and the outcomes can be quite grim.
In light of these findings, the following table summarizes how HCV infection could be used as an essential marker in early cancer detection strategies:
| Aspect | Details |
|---|---|
| HCV Status | Chronic infection vs. isolated exposure |
| Risk Stratification | Higher risk classification for patients with chronic HCV, pertaining specifically to genotype sensitivity |
| Screening Model Integration | Inclusion of HCV treatment history and exposure data to predict pancreatic cancer risk |
| Potential for Treatment Modification | Investigate if direct-acting antivirals (DAAs) reduce PDAC risk post-HCV treatment |
This table clearly outlines that the nuanced interaction between chronic viral infections and cancer formation is a promising area for developing key early detection methodologies that may reveal hidden pieces in the puzzle of pancreatic cancer development.
Re-evaluating HCV Screening Practices in Light of New Evidence
It is a well-known fact that both the CDC and the U.S. Preventive Services Task Force recommend at least one HCV screening in a lifetime for all adults. However, screening rates remain low due to several intimidating barriers including low socioeconomic status, limited healthcare access, lack of awareness, and social stigma surrounding HCV infection.
Critically, if further research confirms that treating HCV can lower the risk of pancreatic cancer, it may revolutionize the current approaches to both viral screening and cancer prevention. Recognizing the small twists in patient behavior and healthcare policies could lead to more effective interventions. Efforts to increase the awareness of these issues are essential for developing robust, all-encompassing public health strategies.
Direct-Acting Antivirals and Their Role in Reducing Cancer Risks
Modern medicine has seen a promising evolution with the advent of direct-acting antivirals (DAAs), which offer super important intervention strategies for chronic HCV infection. These medications have already transformed treatment outcomes for many patients by significantly reducing viral loads and improving liver function.
Now, researchers and clinicians are beginning to wonder whether these drugs could also lower the risk of pancreatic cancer in patients with chronic hepatitis C. While the current study did not directly answer this question, it raised the voice of forward-thinking colleagues who advocate for further work in this area.
Below is a bulleted list illustrating the potential benefits and outstanding questions regarding DAA use and pancreatic cancer risk:
- Potential Benefits:
- Lowering viral loads to mitigate downstream carcinogenic processes
- Improving liver function and reducing overall systemic inflammation
- Possibly altering the microenvironment that predisposes to cancer development
- Outstanding Questions:
- Can DAAs reverse already existing subtle tumor microenvironment alterations?
- What is the ideal timing for antiviral therapy to confer maximum protection against PDAC?
- Are there specific patient groups that might see more dramatic benefits from early DAA initiation?
These lists help to uncover both the promising opportunities and the tangled issues that remain when it comes to integrating DAAs into cancer prevention strategies. Consumers of health information—and indeed, healthcare practitioners—are keen to see if DAA-treated patients demonstrate lower rates of PDAC over time, and if so, this could lead to significant changes in preventive care practices.
The Broader Picture: Addressing the Tricky Crossroads of Viral Infections and Cancer
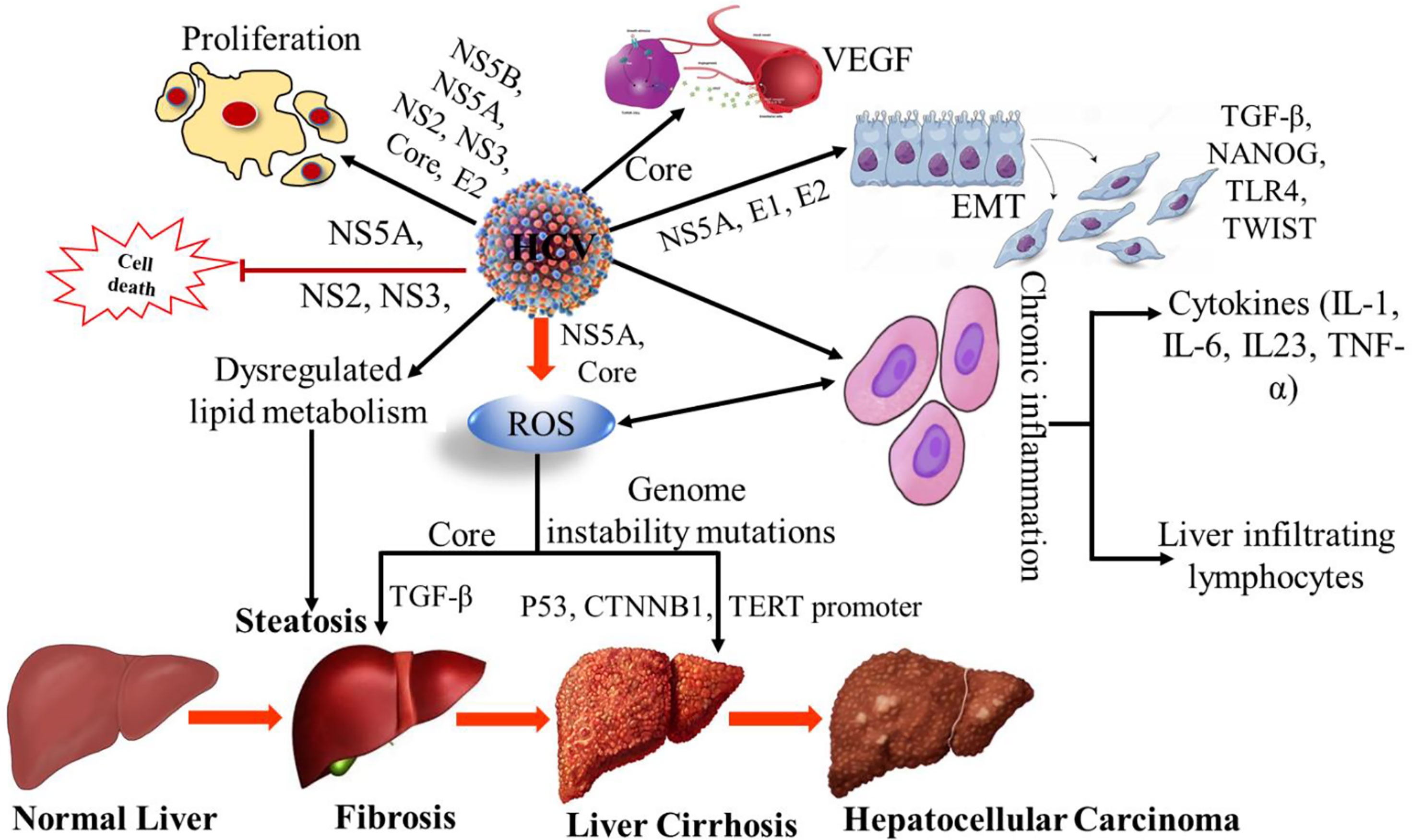
The relationship between viral infections and cancer is one riddled with tension and layered with subtle details. Chronic inflammation, cellular stress, and disruptions in DNA repair mechanisms all contribute to a high-risk environment for malignancies in vulnerable tissues. When discussing pancreatic cancer in the setting of chronic HCV, it is essential to appreciate these small distinctions.
This topic is full of problems, especially when considering how virus-related inflammation might accelerate cellular mutations in the pancreas. Many researchers have already started to piece together the nitty-gritty of how chronic viral infections spur the onset of cancers and what that means for managing patient risks in clinical settings. Here are some of the main points to consider:
- Chronic Inflammation: Prolonged HCV infection triggers sustained inflammatory responses, which may damage pancreatic tissue over time.
- Cellular Mutation Risks: The constant turnover due to inflammation may create a fertile ground for mutations that eventually result in cancer.
- Immune Evasion: HCV, like many viruses, has the ability to escape the immune system, adding another layer of confusion to how the body deals with developing malignancies.
- Synergistic Risks: When combined with other lifestyle risk factors such as smoking and alcohol use, the overall risk of PDAC becomes even more significant.
This multifaceted issue demands that the medical community work through the twists and turns by conducting further research in larger and more diverse populations outside the VA healthcare environment. It also calls for improvements in patient education, emphasizing how intertwined these health issues are.
Challenges in Data Interpretation and External Validity
Another important angle is the challenge of applying these findings to the broader public. Veterans, as a study population, present certain limitations because their healthcare backgrounds and lifestyle factors differ from those found in the general population. This factor makes it a bit nerve-racking to assume that the same risk levels apply universally.
Key issues that come up include:
- Demographic Differences: The age, gender, and ethnic makeup of veterans differ significantly from other groups. This needs a closer look before applying the study conclusions more broadly.
- Healthcare Access: Veterans often receive treatment through distinct healthcare systems (VA or VA-linked programs) that may not mirror the community-based practices outside these systems.
- Exposure Variations: Occupational exposures and unique lifestyle habits prevalent among veterans might not be as common in the general population.
Working through these observations, it becomes clear that to truly appreciate the impact of chronic HCV on pancreatic cancer risk, researchers must engage in further studies in non-veteran cohorts. This external validation is key to confirming the findings and determining their wider applicability.
Importance of Multidisciplinary Collaboration
One of the exciting prospects emerging from this research is the potential for multidisciplinary collaboration. Experts in hepatology, oncology, epidemiology, and even social services need to figure a path together to address both the tricky parts of HCV management and pancreatic cancer prevention.
This approach brings several advantages:
- Holistic Patient Care: Combining insights from various fields leads to better management strategies that address not only the direct effects of HCV but also the associated risk factors for cancer.
- Improved Early Detection: Insights from epidemiological studies can help refine screening programs, allowing for earlier interventions that are less intimidating for patients.
- Policy Development: Harmonizing the knowledge across disciplines supports the design of robust public health policies that reduce risk and improve outcomes.
When experts from different fields pool their knowledge and get into open discussions, they create opportunities to develop innovative solutions for these complex issues. The study, therefore, is not just an isolated piece of research; it is a call to action for a more integrated, patient-centered approach to disease prevention and care.
Patient-Centered Strategies and the Role of Education
Another critical takeaway from the research is the need for enhanced patient education regarding HCV infection and its potential link to pancreatic cancer. Many individuals remain unaware of the long-term health implications of HCV, partly due to the overwhelming stigma and nerve-racking misconceptions associated with the virus.
Effective patient education can help steer through the tangled issues by empowering patients with the knowledge they need to make informed decisions. Some key educational points could include:
- Understanding HCV: Clarifying the nature of a chronic viral infection, highlighting how it can quietly persist over years and gradually lead to more severe health complications.
- Early Detection and Screening: Emphasizing the importance of undergoing routine HCV screening, especially given the recommendations by public health agencies to have at least one screening in a lifetime.
- The Benefits of Treatment: Explaining how DAAs can play an essential role in managing HCV, potentially reducing downstream risks such as PDAC.
- Mitigating Lifestyle Risks: Promoting lifestyle modifications, like smoking cessation and moderation of alcohol use, that can further decrease the risk of cancer development.
Educational materials should be tailored to the audience, using easily understandable language and supporting visuals, such as infographics or decision trees that outline patient pathways for screening and treatment. Empowering patients in this way not only improves individual outcomes but also reduces healthcare costs by preventing late-stage disease presentations.
Community Outreach and Addressing Social Barriers
Community outreach plays a super important role where structured patient education meets real-world challenges. Many people with HCV, especially those from lower socioeconomic backgrounds, might not have ready access to reliable health information. This digital divide and the social stigma surrounding the condition can act as major roadblocks.
Efforts to overcome these barriers may include:
- Local Health Workshops: Organizing free or low-cost sessions in community centers can help educate individuals about HCV and its broader health implications.
- Collaboration with Nonprofits: Working with organizations that specialize in public health can increase awareness and provide necessary support services.
- Online Information Portals: Creating user-friendly websites and support forums where patients can ask questions without fear of judgment.
- Partnerships with Local Clinics: Encouraging local clinics to integrate HCV screening and counseling into routine care to reach a broader segment of the population.
By tackling these social and informational barriers head-on, healthcare providers can ensure that more people receive timely care—reducing the overall burden of both HCV and its potential complications, including pancreatic cancer.
Translating Research Findings Into Public Health Policy
The translation of research findings into public health policy is both essential and challenging. The current study’s results should act as a catalyst for reevaluating and potentially revamping screening protocols for HCV, especially in populations that are at higher risk for pancreatic cancer.
Policy makers could consider the following measures as they work through this process:
- Enhanced Screening Programs: Expanding HCV screening to include follow-up mechanisms that monitor at-risk individuals for signs of pancreatic or liver cancers.
- Access to DAAs: Improving patient access to direct-acting antivirals, particularly for underserved populations who might lack comprehensive health insurance.
- Tailored Health Campaigns: Launching public health campaigns that address the intertwined issues of viral infections and cancer risks, using clear and relatable language.
- Data Collection and Research Funding: Investing in further research to validate these findings in diverse populations, which could inform future adjustments to national guidelines.
By implementing policy changes based on new evidence, governments and healthcare institutions could find their way out of the confusing bits that have traditionally hampered effective treatment protocols. The success of such policies depends on the close collaboration between researchers, clinicians, and policy makers, all working through the twists and turns together.
Challenges and Opportunities in Policy Implementation
Of course, translating academic research into workable public health policies is not without its challenges. There are several confusing bits that need to be sorted out before any sweeping changes can be made:
- Resource Allocation: Securing the necessary funding and staff to support expanded screening programs can be a nerve-racking endeavor, particularly in settings with already stretched resources.
- Data Integration: Integrating data from diverse healthcare systems, such as the VA and private sectors, might prove complicated and require harmonized standards.
- Patient Engagement: Motivating patients to participate in screening and follow-up studies may be off-putting for some due to social stigma or misunderstanding about HCV.
- Timely Evaluation: Setting up systems for continuous evaluation and quick response to newly emerging data is critical, yet often challenging in bureaucratic environments.
Despite these challenges, the opportunities to create a more responsive and preventative healthcare system are immense. By investing in detailed patient education, improved screening protocols, and continuous data monitoring, public health policies can become a cornerstone in the fight against both chronic HCV infection and pancreatic cancer.
Future Research Directions and the Way Forward
The study raises as many questions as it answers. While the association between chronic HCV and PDAC is clear within the veteran population, the next steps involve confirming these results in more representative groups and further exploring the interplay between viral infections and cancer development.
Some key areas for future research include:
- Validation in General Populations: Conducting additional studies in non-veteran cohorts to verify if the same risk patterns hold true.
- Impact of DAA Treatment: Investigating whether treating HCV with direct-acting antivirals can meaningfully lower the risk of developing pancreatic cancer, and if so, what the optimal treatment window might be.
- Detailed Genotype Analysis: Exploring in greater detail why certain HCV genotypes, such as genotype 3, exhibit a higher risk profile compared to others. This may involve analyzing the subtle parts of viral behavior and host response.
- Early Detection Model Refinement: Integrating HCV status and other risk markers into predictive models designed for early detection of PDAC. Such models must account for the little twists of timing and patient lifestyle factors.
- Collaborative Research Networks: Forming networks that bring together clinicians, researchers, and policy experts to pool data and address these tangled issues in a comprehensive manner.
By investing in future research, we can better understand how to manage the overlapping risks associated with chronic viral infections and cancer. As research continues to evolve, it is super important for the medical community to keep its eye on how each new study informs patient care decisions and public policy.
Encouraging a Patient-Centric Research Agenda
One promising avenue for future research is to develop a patient-centric approach that takes into account the individual’s entire health landscape. Instead of treating chronic HCV as an isolated issue, researchers and clinicians should consider a more holistic perspective, incorporating factors such as:
- Genetic Predispositions: How does a patient’s genetic makeup influence both their susceptibility to HCV-related complications and their overall cancer risk?
- Lifestyle Choices: To what degree do behaviors like smoking and alcohol consumption amplify the risk posed by chronic HCV?
- Socioeconomic Factors: How do limited resources and access to care further complicate early detection and treatment strategies?
This patient-focused research could help design personalized intervention protocols that not only address viral infections but also reduce the overall burden of cancer. As we continue to get into this subject, the detailed study of individual patient scenarios will be as important as the broad trends observed in large-scale epidemiological studies.
Final Thoughts on Integrating Research, Practice, and Policy
In wrapping up our discussion, it becomes clear that the recent study linking chronic hepatitis C to an increased risk of pancreatic cancer is a call for action on multiple fronts. The findings force us to confront the tricky parts of viral oncology, emphasizing that healthcare providers must work through complex pieces to create effective, patient-centered solutions.
From a clinical perspective, the study highlights the importance of rethinking screening and early detection strategies. If future work confirms that effective treatment of HCV can lower PDAC risk, the implications could be transformative—not only for specialized populations like veterans, but for the general public as well.
Policy makers are also left with much to consider. Adjusting preventive care initiatives to include enhanced screening and timely treatment for HCV is not a small task. It requires careful integration of research findings, substantial resource allocation, and a collaborative mindset that involves multiple stakeholders. But the potential benefits—improved patient outcomes, reduced healthcare costs, and ultimately lower rates of a highly fatal cancer—are well worth the nerve-racking effort.
Moreover, the study reminds us of the necessity for comprehensive patient education and community outreach. By using clear language and providing reliable information, healthcare professionals can empower individuals to take charge of their health, thereby finding their path to better outcomes amid the tangles of modern medical challenges.
As we navigate the twists and turns of this evolving field, it is super important to remember that every step forward in research and patient care contributes to a broader understanding and, ultimately, better health outcomes for everyone. The road ahead is full of subtle details and complicated pieces, but with an integrated approach involving research, clinical practice, and informed public health policy, we can make meaningful progress in reducing the burden of both HCV and pancreatic cancer.
Looking Ahead With Optimism and Collaboration
While the journey to fully understand and fight the development of pancreatic cancer in patients with chronic hepatitis C is laden with challenges, there is ample reason for optimism. Collaborative efforts across disciplines, ongoing research, and enhanced patient engagement strategies can pave the way for groundbreaking advances in care.
As we continue to figure a path through the confusing bits and tangled issues of virus-induced cancers, the collective expertise of clinicians, researchers, policy makers, and patient advocates will be our strongest asset. Together, we can work toward a future where early detection and effective intervention dramatically improve patient outcomes, even in areas that once seemed overwhelmingly complex.
Ultimately, this study is not just a reminder of the dark corners within our current understanding—it is also a beacon pointing to future opportunities. Embracing these challenges with open minds and collaborative spirit will allow us to break down the barriers and ensure that every patient has the chance for a healthier future.
Originally Post From https://www.medpagetoday.com/hematologyoncology/othercancers/118541
Read more about this topic at
Pancreatic Ductal Adenocarcinoma After Hepatitis C Infection
Pancreatic Ductal Adenocarcinoma After Hepatitis C Infection


