Rectal Cancer Cure Rate: A Closer Look at Modern Treatment Strategies
The landscape of rectal cancer treatment has evolved significantly over the past few decades. With advances in surgery, radiation, chemotherapy, and personalized medicine, the hope of achieving a cure has become more than just a distant dream for many patients. However, understanding the tricky parts and tangled issues involved in treating rectal cancer remains essential for anyone seeking clarity about their condition and treatment options.
In this opinion editorial, we will take a closer look at the key aspects influencing rectal cancer cure rates. We will explore early detection methods, surgical advancements, combined modality treatments, and alternative treatment strategies. By breaking down the fine points of each treatment approach, we hope to provide a balanced view of where the field stands today and where it is headed tomorrow.
Understanding the Tricky Parts of Rectal Cancer Treatment
Rectal cancer, which originates in the final 12–15 centimeters of the large intestine, is distinct from colon cancer due to its unique anatomical location in the pelvis. This location requires specialized treatment approaches and careful management to achieve optimal outcomes. Because of its confined space, the cancer often requires a multidisciplinary approach that involves surgical, radiation, and medical oncology teams working together to figure a path through the challenging treatment landscape.
When discussing the cure rate for rectal cancer, several tangled issues need to be considered:
- Stage of Diagnosis: Earlier stages often respond very well to treatment, while more advanced stages present complicated pieces that require intensive therapy.
- Tumor Biology: The biological characteristics and genetic makeup of the tumor play a key role in both how aggressive the cancer is and how it responds to treatment.
- Treatment Strategy: Modern multimodal therapy, which integrates surgery, radiation, and chemotherapy, has been crucial in improving overall outcomes.
This combination of factors illustrates why the success in curing rectal cancer demands more than just a one-size-fits-all mentality. Instead, it requires a finely tuned strategy that is adaptable to the subtle details of each patient’s condition.
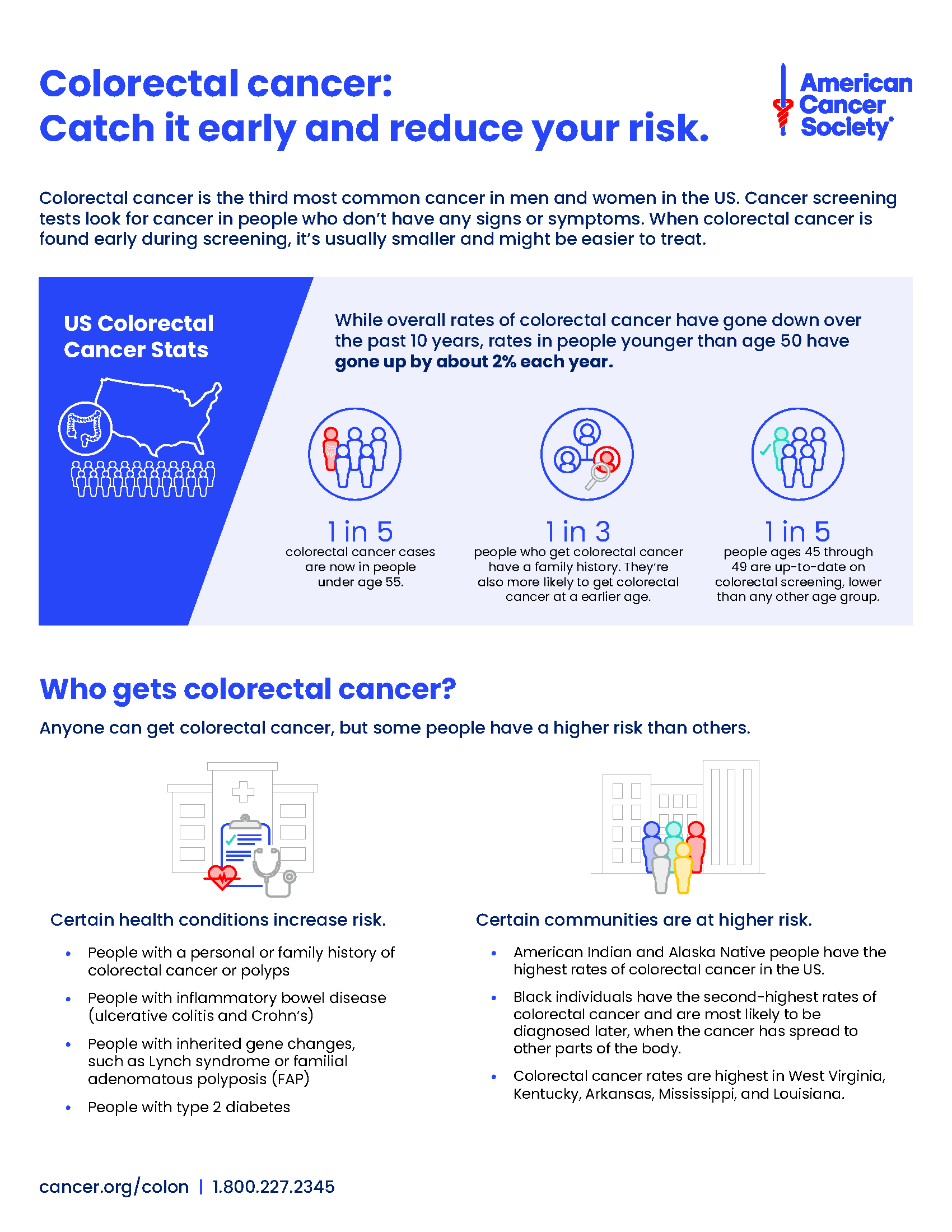
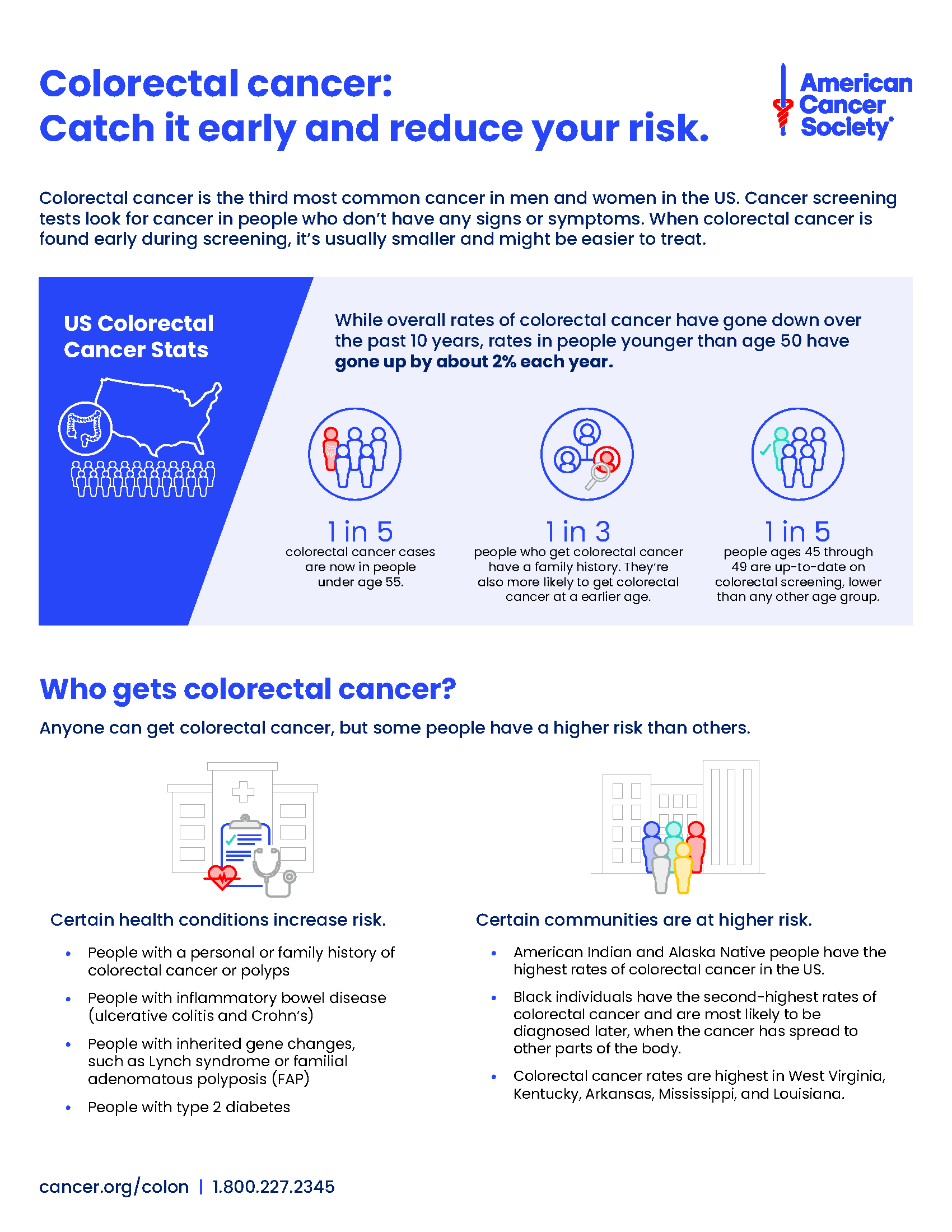
Early Detection and the Key Role of Screening Colonoscopy
One of the most essential elements in managing rectal cancer is early detection. Screening colonoscopy remains the most effective tool for finding rectal tumors before they develop deep roots or invade nearby structures. Early identification of the disease can often lead to a cure rate that far surpasses what is achievable at later stages.
Identifying rectal cancer early offers several clear benefits:
- Removal of Precancerous Polyps: Colonoscopy not only detects cancer but also allows for the removal of polyps that might develop into cancer in the future.
- Timely Diagnosis: Early symptoms, such as rectal bleeding, changes in bowel habits, or unexplained weight loss, alert patients to seek medical advice sooner.
- Improved Treatment Options: When tumors are identified while they are still confined to the rectal wall (Stage I), surgical treatment alone can achieve cure rates exceeding 90%.
Screening programs and heightened public awareness have been crucial in driving earlier diagnoses. Patient education and outreach are super important components in this battle against cancer, ensuring that those at risk can get the appropriate tests and begin treatment at the right time.
Surgical Advancements and Their Impact on Cure Rates
Surgery remains at the forefront of curative strategies in rectal cancer treatment. Modern surgical techniques have made headway in managing even the challenging parts of localized and locally advanced tumors. The adoption of procedures like total mesorectal excision (TME) has been transformational. With the removal of both the tumor and surrounding lymph nodes, the risk of local recurrence is significantly lowered.
Key improvements in surgical care include:
- Precision Techniques: Utilizing advanced imaging and preoperative planning, surgeons are better equipped to secure clean margins, a factor crucial for reducing recurrence.
- High-Volume Centers: Hospitals and cancer centers that specialize in colorectal surgery tend to yield better outcomes through accumulated experience and specialized interdisciplinary teams.
- Minimally Invasive Approaches: Laparoscopic and robotic surgeries have contributed to faster recovery times and lower rates of postoperative complications.
When discussing cure rates, it is important to note that, in Stage I disease, where tumors are confined to the rectal wall, surgical treatment alone can lead to long-term remission in 90% or more of cases. For more advanced stages, surgery is often combined with other treatment modalities to overcome the small twists that can arise from more complicated tumor biology or local spread.
Managing the Challenging Combined Modality: Radiation and Chemotherapy
Unlike colon cancer, rectal cancer often benefits from the integration of radiation and chemotherapy, particularly when administered prior to surgery. Neoadjuvant chemoradiotherapy has become the standard-of-care for Stage II and III rectal cancers. This approach shrinks tumors, making them easier to remove, and reduces the risk of local recurrence significantly.
There are several reasons why radiation and chemotherapy are critical in the management of rectal cancer:
- Tumor Shrinkage: Administered before surgery, chemoradiation reduces tumor size, increasing the likelihood of complete surgical resection.
- Reduced Recurrence: By lowering the local tumor burden, the combination significantly minimizes the chances of cancer reappearing in the pelvic region.
- Total Neoadjuvant Therapy (TNT): This innovative method, which involves both chemotherapy and radiation prior to surgery, has shown further improvements in survival rates and a higher chance of achieving a pathologic complete response—where no trace of cancer is detected at the time of surgery.
Clinical trials such as RAPIDO and PRODIGE-23 have provided encouraging data, suggesting that the right combination of treatment modalities can overcome many of the nerve-racking barriers typically associated with advanced rectal tumors.
Alternative Approaches: Watch-and-Wait Strategy in Rectal Cancer
For selected patients who achieve a complete clinical response following chemoradiotherapy, a non-operative, “watch-and-wait” strategy is emerging as an innovative alternative to immediate surgery. This approach offers the possibility of preserving rectal function and quality of life by avoiding surgical intervention while still ensuring excellent control over cancer.
The watch-and-wait strategy provides several potential advantages:
- Organ Preservation: By avoiding surgery, patients can maintain their normal bowel function and reduce postoperative complications.
- Quality of Life: Patients may experience less disruption in daily activities and overall well-being compared to traditional surgical approaches.
- Comparable Cure Rates: Early studies indicate that, in carefully chosen patients,
the long-term cure rates are comparable to those achieved through conventional surgery.
While the watch-and-wait model is not universally applicable and requires meticulous and ongoing monitoring, it offers a promising avenue for personalized care in rectal cancer management. It is an example of how personalized treatment plans can offer hope even in situations that at first glance might seem off-putting.
Challenges in Advanced and Metastatic Disease: Tackling Tangled Issues
When rectal cancer advances beyond the primary site and spreads to distant organs, cure becomes more challenging, though not entirely out of reach. Advanced stages of rectal cancer, particularly Stage IV, demand rigorous therapeutic interventions and a well-coordinated multidisciplinary approach.
Key challenges in advanced and metastatic rectal cancer include:
- Limited Scope for Curative Surgery: For patients with extensive metastatic lesions, especially in organs such as the liver or lungs, surgery might only be feasible in select cases where the metastases are resectable.
- Combination Therapies: For many patients, combination chemotherapy along with targeted therapies and immunotherapy may offer improved survival. Newer molecular profiling and precision oncology approaches have opened avenues for using drugs tailored to the specific genetic makeup of the tumor.
- Overcoming Resistance: Some tumors develop resistance to standard treatments. These nerve-racking challenges require ongoing clinical trials and research to discover more effective options.
Innovations in targeted therapy and the integration of immunotherapy have shown promise, especially for patients with certain genetic markers such as MSI-H. Although the overall goal of a complete cure is more elusive in advanced cases, the focus has shifted toward achieving functional cure, wherein long-term disease control and quality of life are optimized.
Personalized Medicine: The Promise of Tailored Treatment Strategies
The future of rectal cancer treatment lies in personalized medicine—an approach that tailors treatment strategies to the individual patient’s genetic profile and tumor characteristics. By examining the hidden complexities within each tumor, clinicians can better predict which therapies will be most effective.
Areas where personalized medicine is making a difference include:
- Genetic Profiling: Analysis of mutations such as KRAS, BRAF, and MMR status helps in predicting treatment response and overall prognosis.
- Immunotherapy: For patients with tumors characterized by high microsatellite instability (MSI-H), immunotherapy has emerged as a super important treatment option that can potentially improve outcomes dramatically.
- Targeted Therapies: Drugs designed to target specific molecular pathways in cancer cells provide a more focused attack on the tumor, offering hope where traditional therapies might have seemed overwhelming.
This approach not only improves the odds of achieving a cure in localized disease but also offers valuable insights into managing advanced and metastatic rectal cancer. The integration of artificial intelligence into imaging and pathology is another promising avenue, as it may help figure a path through the small distinctions that determine treatment success.
Patient Lifestyle Factors: The Other Side of the Equation
Beyond treatment modalities and technological advances, patient lifestyle factors have a critical influence on rectal cancer outcomes. Smoking, obesity, diet, and exercise habits can all affect tumor behavior, treatment tolerability, and recurrence risk.
Some key considerations related to lifestyle include:
- Nutrition and Diet: A balanced diet rich in whole grains, vegetables, and lean proteins can support overall health and aid recovery during and after treatment.
- Physical Activity: Regular exercise not only aids in maintaining a healthy weight but also improves cardiovascular health and reduces fatigue, which can be significant challenges during cancer treatment.
- Smoking Cessation: Quitting smoking is among the most critical changes patients can make, as smoking has been linked to higher recurrence rates and poorer overall outcomes.
In addition, psychological support, counseling, and involvement in support groups can help patients manage the nerve-racking emotional toll of a cancer diagnosis and its subsequent treatment. Overall, a holistic approach that combines aggressive treatment with supportive care and lifestyle modifications is proving to be integral in enhancing both cure rates and quality of life.
Future Directions: Revolutionizing Rectal Cancer Outcomes
The fight against rectal cancer is continually evolving, ushering in new treatment paradigms and research pathways. Several promising areas are poised to further enhance cure rates in the coming years:
New Radiotherapy Techniques: Innovative radiation methods such as intensity-modulated radiotherapy (IMRT) and image-guided radiotherapy (IGRT) allow oncologists to precisely steer through targeted areas while sparing surrounding healthy tissues. These advancements help reduce side effects and improve overall outcomes.
Integration of Artificial Intelligence: AI is beginning to play a transformative role in the field of oncology. From precision diagnostics to personalized treatment plans, AI tools assist physicians in getting around the complicated pieces of tumor assessment with greater accuracy.
Novel Drug Therapies and Immunotherapies: Ongoing clinical trials are testing next-generation drugs that offer the potential to overcome treatment resistance. Targeted immunotherapies, designed based on the tumor’s genetic makeup, are showing early promise and could redefine treatment for patients with challenging disease profiles.
Enhanced Screening and Early Detection Programs: Advances in imaging technology and biomarker research are setting the stage for earlier, more accurate diagnosis. The earlier a tumor is detected, the better the chance of achieving a long-term remission. Outreach programs and public education are essential in this ongoing battle, ensuring that patients are aware of the subtle parts of early cancer signs.
The global healthcare community continues to work through the small twists involved in refining treatment standards and integrating emerging scientific findings into clinical practice. Collaborative efforts among research institutions, pharmaceutical companies, and cancer centers around the world are accelerating the pace at which these innovations become standard care.
Real-World Impact and the Role of Multidisciplinary Teams
The treatment of rectal cancer is rarely a solo endeavor. Instead, it involves the thoughtful collaboration of colorectal surgeons, medical oncologists, radiation oncologists, radiologists, and supportive care teams. These multidisciplinary teams are key to making informed decisions and tailoring treatment strategies that are both aggressive and considerate of the patient’s overall well-being.
Some highlighted roles in this collaborative framework are:
- Surgical Teams: Focus on precise tumor removal and management of local disease.
- Radiation Oncologists: Craft radiation plans that maximize tumor eradication while minimizing collateral damage.
- Medical Oncologists: Coordinate systemic therapies and manage combination treatment protocols.
- Nurses and Supportive Care Staff: Provide ongoing patient care, both administratively and emotionally, as patients work through treatment.
It is the power of these integrated teams that offers the best chance for patients to not only overcome the intimidating challenges of rectal cancer but also to enjoy a sustained quality of life thereafter.
Balancing Treatment Risks and Long-Term Survivorship
No discussion of rectal cancer cure rates would be complete without addressing the nerve-racking risks associated with treatment. Every step in the treatment journey—from surgery to radiation to chemotherapy—carries potential complications and side effects. These can include bowel changes, fatigue, neuropathy, and emotional implications that span months or even years.
To manage these risks, healthcare providers employ rigorous follow-up protocols. These may include:
- Regular Imaging and Colonoscopies: To detect any signs of recurrence as soon as possible.
- Physical Examinations: Standard check-ups that help monitor the patient’s overall health.
- Supportive Care and Rehabilitation: Addressing the long-term physical and emotional effects of treatment is super important for enduring survivorship.
Patients who navigate these treatment phases often report that the benefits of state-of-the-art care outweigh the short-term struggles experienced during the treatment process. Continuous improvements in supportive care are designed to help patients figure a path to a healthy and rewarding life post-treatment.
Conclusion: A Hopeful Outlook for the Future of Rectal Cancer Treatment
The journey through rectal cancer treatment is filled with both challenges and opportunities. While the tricky parts of advanced tumor biology and the nerve-racking uncertainties of metastatic disease can feel overwhelming, advances in modern medicine have steadily improved the cure rate across all stages of rectal cancer.
Early detection through meticulous screening, sophisticated surgical techniques, optimized chemoradiotherapy protocols, and the promise of personalized medicine all contribute to a future where a cure is increasingly within reach for most patients. It is this delicate balance between aggressive treatment and holistic care that paints a hopeful picture—a picture where even the most confusing bits of rectal cancer management are met with innovative strategies and a resilient spirit.
As we look to the future, ongoing research and collaborative efforts among experts in the field will undoubtedly continue to refine treatment protocols, reduce side effects, and ultimately improve survival rates. The integrated approach to care, which combines technical expertise with supportive measures addressing both physical and emotional challenges, sets the stage for a more comprehensive and compassionate model of cancer care.
In today’s global fight against cancer, no barrier is insurmountable. With every new clinical trial, every interdisciplinary meeting, and every piece of emerging research, we take another step toward ensuring that patients can look forward to long, healthy lives beyond their diagnosis. The world of rectal cancer treatment is ever-changing, but one fact remains clear: hope is alive, and the outlook for rectal cancer patients is brighter than ever.
Ultimately, conquering rectal cancer is not just about eliminating a tumor—it’s about overcoming the tangled issues, managing the small distinctions in each case, and forging a path forward that embraces the full spectrum of patient needs. Whether through traditional surgery, cutting-edge targeted therapies, or innovative non-operative approaches, every effort brings us closer to turning rectal cancer from a formidable adversary into a manageable condition with lasting, meaningful remission.
For patients, caregivers, and healthcare professionals alike, staying informed about the evolving treatment landscape is key. As our understanding deepens and our therapies become more refined, there is every reason to believe that the story of rectal cancer treatment will continue to be one of progress, resilience, and, ultimately, victory.
In conclusion, the advancements in rectal cancer treatment offer a powerful message of hope. With thorough screening, individualized treatment approaches, and ongoing improvements in multidisciplinary care, rectal cancer is increasingly being seen not just as a deadly disease but as a challenge that can be met with courage, innovation, and a steadfast commitment to patient well-being. Now more than ever, the focus is on achieving sustainable outcomes that allow every patient to thrive after treatment.
It is our duty as healthcare professionals, researchers, and advocates to ensure that this progress continues. By supporting comprehensive cancer research, encouraging early detection efforts, and continuing to refine treatments based on both clinical evidence and individual patient needs, we can collectively work to reduce the impact of rectal cancer. The journey is far from over, but there is immense reason for optimism as we work together to steer through the complex pieces of treatment and carve out a future where a cure is not only possible but expected.
The evolving story of rectal cancer treatment is one of persistence, innovation, and hope. As we continue to confront the small twists and pitfalls along the way, the progress made so far serves as a beacon of light to all who have been touched by this disease. With every challenge met, we move closer to a future where rectal cancer’s impact is minimized, and the cure rate reaches new, encouraging heights.
Let us remain committed to this cause, supporting ongoing research, embracing multidisciplinary care, and advocating for every patient’s right to the best possible treatment. The path may be full of problems and nerve-racking turns, but together, we can ensure that the advancements in this field lead to enduring, life-saving progress for generations to come.
Originally Post From https://oncodaily.com/oncolibrary/rectal-cancer-cure-rate
Read more about this topic at
Rectal cancer – Diagnosis and treatment
Rectal Cancer Treatment – NCI