An Emerging Perspective on Managing Overlapping Autoimmune Disorders
In recent years, the medical community has been increasingly faced with tangled issues surrounding the management of autoimmune conditions that affect multiple organs. A recent case report involving a 36-year-old woman with plaque psoriasis coexisting with primary sclerosing cholangitis and ulcerative colitis has sparked considerable discussion. This case highlights the potential of alternative therapeutic options—and specifically, apremilast—as a promising treatment avenue. While this is only one case, it calls for a broader conversation about the challenges and possibilities that come with managing multi-system autoimmune diseases.
From a broad perspective, overlapping autoimmune diseases are not just a collection of individual ailments. They are a convergence of immune-mediated disorders that share some hidden complexities in their underlying mechanisms. The patient’s experience, for example, underscores the tricky parts encountered when the autoimmune system targets multiple organs. These complications include managing side effects, ensuring stable liver function, and effectively controlling inflammatory symptoms. With chronic conditions such as psoriasis, inflammatory bowel illness, and autoimmune liver disease converging, it becomes essential to figure a path that not only relieves symptoms but also promotes long-term wellness.
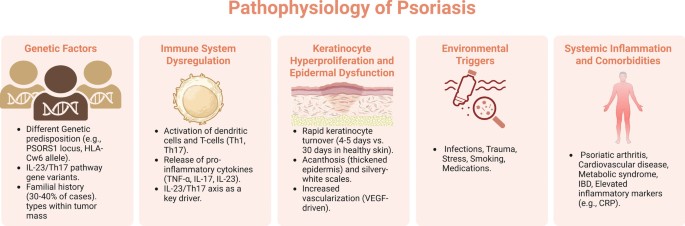
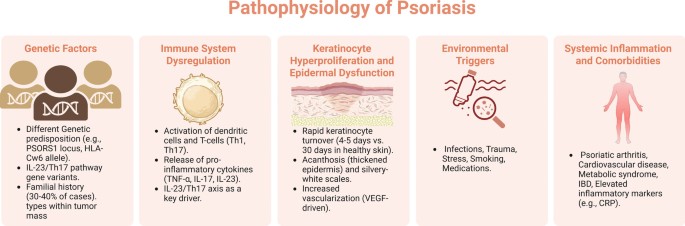
Understanding the Interplay Between Autoimmune Conditions
When conditions such as psoriasis, primary sclerosing cholangitis, and ulcerative colitis appear together, it creates a full-of-problems scenario. Each disorder, when isolated, presents its own set of challenges; however, when combined, the small distinctions in their immunopathogenic mechanisms can create a nerve-racking puzzle for healthcare providers. Although these are all recognized as immune-mediated inflammatory disorders, understanding the subtle parts of how they affect one another on a systemic level is still a work in progress.
In the case at hand, layered challenges emerged as the patient’s symptoms evolved over a number of years. With over a decade of visible psoriatic lesions, alongside several years of liver dysfunction and more than a year of chronic diarrhea, the clinical presentation demanded a comprehensive assessment. Traditional treatment methods—including oral steroids and adalimumab—proved insufficient in managing her condition. This underscored a pressing need to dive in and look into alternative treatment strategies that could address multiple underlying issues concurrently. It is in these tangled issues that the spotlight falls on apremilast and its innovative approach to treatment.
Examining the Role of Apremilast in Autoimmune Therapeutics
Apremilast has made news headlines as a novel therapeutic option that offers a fresh angle in treating psoriasis. Its significance is amplified when the condition coexists with other inflammatory conditions such as autoimmune liver disease and inflammatory bowel disease. The drug operates by modulating the immune response, thus potentially addressing several of the hidden complexities involved in multi-system inflammation.
One of the key advantages of apremilast is its ability to target the key inflammatory pathways that are common across multiple autoimmune conditions. For many patients who have not responded well to more conventional therapies like steroids or biologics (for example, adalimumab), apremilast represents a beacon of hope. In the featured case, after a rigorous 48-week trial on apremilast—titrated to 60 mg per day—the results were nothing short of dramatic.
A brief overview of the patient’s journey with apremilast includes the following highlights:
- Complete clearance of psoriatic lesions
- Remarkable reduction in pruritus or annoying skin irritation
- Stabilization of liver function despite pre-existing dysfunction
- A significant decrease in diarrhea frequency, leading to improved quality of life
- No serious or adverse events reported
These outcomes not only suggest that apremilast can serve as a super important therapeutic alternative but also raise interesting questions about how we might manage overlapping autoimmune conditions in a more holistic manner. The patient’s positive response encourages both clinicians and researchers to get into the details of how such treatments might be optimized for broader usage in multi-organ autoimmune disease management.
Exploring the Hidden Complexities in Multi-System Autoimmune Diseases
The clinical case we are discussing is like peeling an onion—each layer reveals additional, slightly different issues that require attention. Working through these issues involves understanding a range of subtle details: from the fine points of immunologic signaling to the less obvious clinical manifestations that can affect the liver, skin, and gastrointestinal tract simultaneously. This is not just about treating symptoms; it’s about addressing the root causes and fine shades of inflammatory responses.
Here is a table summarizing some of the compelling features of overlapping autoimmune conditions:
| Condition | Main Symptoms | Key Challenges |
|---|---|---|
| Plaque Psoriasis | Red, scaly skin patches; chronic inflammation | Cosmetic concerns; pruritus; psychological impact |
| Primary Sclerosing Cholangitis | Liver dysfunction; bile duct inflammation | Progressive liver damage; limited effective treatments |
| Ulcerative Colitis | Chronic diarrhea; abdominal pain; rectal bleeding | Risk of colon cancer; frequent flare-ups; nutritional challenges |
Combining these conditions in a single patient creates a situation that is not only confusing but also intimidating to manage clinically. Each condition has its own set of twists and turns, and the overlapping nature of shared inflammatory pathways means that treatment approaches must be both rigorous and innovative. Traditional therapies might fall short, requiring clinicians to be flexible and open to experimenting with newer, more targeted treatments such as apremilast.
Balancing Benefits and Risks in Multi-Therapy Management
When dealing with multiple interlinked conditions, it is essential to figure a path that balances benefits and potential risks. In the detailed case report, the patient had already attempted therapies like oral steroids and biologics, which yielded overwhelming disappointments. This underscores how treatment for complex, misaligned immune disorders can be loaded with issues. Physicians must not only rely on standard protocols but also be prepared to adjust treatment plans based on ongoing observations and the patient’s tolerance levels. The decision to try apremilast was not taken lightly; it was part of a comprehensive management plan that included ursodeoxycholic acid and phosphatidylcholine, aimed at supporting liver function alongside reducing psoriasis symptoms.
It is important to consider that every treatment option carries its own set of potential benefits and risks. Here are a few strategies for managing them:
- Regular monitoring through liver function tests, dermatologic assessments, and gastrointestinal evaluations.
- A structured approach to medication dosing and gradual titration to minimize adverse reactions.
- Incorporation of other supportive therapies such as nutritional management and stress-reduction techniques.
- Open communication between the patient and healthcare provider to promptly adjust the treatment plan if side effects occur.
This balanced scheme not only ensures that all aspects of the patient’s health are considered but also reinforces the need for holistic care. Combining pharmaceutical solutions with supportive measures strengthens the overall management strategy, ensuring that patients receive comprehensive care that addresses every twist and turn along their treatment journey.
Learning from a Single Case: Broader Implications for Clinical Practice
This single case study offers more than just anecdotal evidence—it provides a stepping stone toward rethinking how we approach multi-organ autoimmune conditions. With the patient achieving complete clearance of her lesions and a marked reduction in other systemic symptoms, the door is opened to new possibilities in treatment paradigms. Yet, it is crucial to remain cautious, as one successful case does not necessarily imply universal applicability. More extensive studies and clinical trials will be necessary before apremilast becomes a standard treatment option across the broader spectrum of autoimmune conditions.
Some of the broader questions that emerge from this discussion include:
- How can we ensure that treatments targeting multiple conditions are safe and effective over the long term?
- What are the subtle differences in how various autoimmune conditions interact with each other?
- Can a single treatment approach be effectively customized to address the individual needs of each patient?
- How do we integrate lifestyle and dietary modifications with pharmaceutical interventions in a holistic treatment plan?
Addressing these questions requires medical professionals to take a closer look at every aspect of patient care. The successful use of apremilast in this combined condition scenario suggests that innovative pharmaceutical options can indeed be part of a more integrated strategy. Such strategies would respect the unique challenges of each condition while also focusing on the shared inflammatory drivers common to many autoimmune disorders.
Integrating Novel Therapies with Conventional Medicine
One of the most compelling parts of this case report is the integration of apremilast into a treatment regimen that also included supportive liver therapies. This combination approach is a fine example of how modern medicine can bring together novel therapies with conventional modalities to create a well-rounded treatment plan. While traditional therapies like steroids have been the cornerstone in managing autoimmune conditions, their potential side effects and inconsistent outcomes often leave patients and physicians searching for alternatives.
A multi-pronged approach may include the following elements:
- Immunomodulation via novel agents such as apremilast to directly address inflammatory pathways.
- Hepatoprotective measures using medications like ursodeoxycholic acid to support liver function.
- Adjunctive therapies including phosphatidylcholine to further stabilize cell membranes and reduce liver stress.
- Close monitoring and regular clinical assessments to tailor and adjust treatments as needed.
Such diversified strategies remind us that often there isn’t a one-size-fits-all treatment. Physicians must be ready to get into the fine details and figure a path that responds to each patient’s unique health profile. While the small distinctions between different medications may seem like minor matters, they can make all the difference when it comes to long-term outcomes and overall quality of life.
Taking a Closer Look at Patient-Centered Treatment Approaches
At the heart of modern medicine lies patient-centered care—a philosophy that demands both compassion and precision. In cases where autoimmune conditions converge, this approach takes on added significance. The patient in our case report was not just a subject within a study; she is a real person whose quality of life improved dramatically due to a carefully tailored treatment plan. Her story compels us to get into the gritty details of her experience, to appreciate the real-world impact and the potential ripple effects for similar patients in the future.
Patient-centered care in autoimmune management involves several critical components:
- Personalized Treatment Plans: Recognizing that each patient presents with a unique mix of symptoms, genetic predispositions, and comorbidities. Tailoring therapy—including drug selection and dosing—ensures that treatment is as specific as possible.
- Holistic Support: Acknowledging the need for supportive measures beyond pharmacotherapy. This might include nutritional support, mental health counseling, and lifestyle modifications—all of which contribute to making the overall treatment less intimidating.
- Regular Follow-Up: Close monitoring allows healthcare providers to detect any side effects early and adjust treatment strategies as needed. This ongoing vigilance is crucial, especially when dealing with overlapping conditions.
- Collaborative Decision Making: Involving patients in their own health decisions builds trust and encourages adherence to the treatment plan. It also allows for shared insights that might improve outcomes.
This multi-layered, patient-centered approach not only addresses the visible symptoms but also takes into account the nerve-racking, behind-the-scenes struggles that patients experience daily. In this light, the integration of apremilast as an alternative therapy becomes a vital part of a larger strategy designed to enhance overall well-being.
Connecting Clinical Innovation With Real-World Impact
The transformation seen in the case of the 36-year-old patient is a reminder that medical innovation can have a profound and immediate real-world impact. Clinical trials and case reports such as these serve as a bridge between theoretical research and everyday practice. The impressive safety profile and positive outcomes associated with apremilast in this scenario are encouraging; yet, they represent just one step in an ongoing process of discovery and adaptation in the medical field.
When evaluating new therapeutic interventions, clinicians must consider several practical aspects, including:
- Efficacy Across Conditions: How well does the treatment work when multiple conditions are present concurrently?
- Ease of Use: Is the drug regimen manageable for patients who are already dealing with multiple health issues?
- Side Effect Profile: What are the risks compared to the benefits, and how can these be mitigated?
- Cost and Accessibility: Are the treatments available and affordable for the majority of patients who might benefit from them?
These practical considerations are as important as the clinical benefits. They remind us that medical practice is not only about developing new drugs but also about ensuring that these advancements translate into real improvements in patients’ lives. The experience with apremilast in this case report is a promising signal that, when managed thoughtfully, novel therapies can fit harmoniously into a comprehensive treatment landscape for autoimmune disorders.
Charting a Future Path for Autoimmune Disease Management
Looking ahead, this case report invites us to take a closer look at our existing treatment paradigms and consider where innovation might lead us next. The integration of modern pharmaceuticals, such as apremilast, within a framework that also respects traditional supportive care methods is a promising development. The journey ahead involves sorting out a myriad of interconnected small distinctions and ensuring that we do not overlook any subtle details in the patient’s overall health profile.
As research continues and more data become available, the following focal points may guide future efforts:
- Expanded Clinical Trials: Conduct larger, controlled studies to verify whether the successes seen in this case can be replicated across diverse patient populations.
- Mechanistic Studies: Invest in research that dives into the immunological pathways shared by different autoimmune conditions, potentially revealing new targets for therapy.
- Interdisciplinary Collaboration: Encourage communication between dermatologists, gastroenterologists, hepatologists, and immunologists to holistically manage patients with multi-system diseases.
- Personalized Medicine: Leverage genetic profiling, biomarker analysis, and other modern tools to tailor treatments more precisely to individual patient needs.
Each of these pathways represents a stepping stone toward a future where multi-system autoimmune diseases are managed more successfully. The experience with apremilast is a testament to the fact that even when the road seems intimidating and full of problems, there are still promising avenues to explore. With a commitment to patient-centered care, ongoing research, and clinical collaboration, the medical community can hope to figure a path through even the most tangled issues in autoimmune disease management.
Bridging Gaps Between Research and Everyday Clinical Practice
One of the greatest challenges in healthcare is making sure that innovations in research quickly and efficiently translate into everyday clinical practice. While case reports like the one discussed here provide a glimpse of what the future may hold, the actual process of bridging this gap requires careful planning and execution. Healthcare providers must work together to develop guidelines and protocols that integrate new treatment options—even as novel as apremilast—into standard care routines.
Some actionable steps for bridging this research-to-practice gap include:
- Educational Initiatives: Organize training sessions, workshops, and seminars to familiarize practitioners with innovative therapies and their nuanced applications.
- Guideline Revisions: Update treatment guidelines periodically to incorporate the latest research findings, ensuring that clinicians are not left behind by emerging trends.
- Patient Education: Keep patients informed about new treatment options, empowering them to take an active role in their own health decisions.
- Cross-Disciplinary Conferences: Support forums where specialists from different fields can share experiences and collaboratively address the complicated pieces of managing overlapping conditions.
These steps are not just administrative necessities—they are critical components that ensure medical breakthroughs benefit the widest possible audience. When research and practice work hand in hand, patients receive care that is both scientifically sound and personally tailored to their individual needs.
Conclusion: A Hopeful Glimpse into a More Integrated Future
The case report featuring the use of apremilast in a patient battling plaque psoriasis alongside primary sclerosing cholangitis and ulcerative colitis offers more than just clinical data; it provides a narrative of hope amid tangled issues. It underscores the potential for novel therapies to break new ground in the treatment of complex, overlapping autoimmune conditions. Even though the path forward is riddled with challenges, the success seen in this instance gives both clinicians and patients a reason to be optimistic.
While the complete picture of how best to treat overlapping autoimmune disorders is still emerging, one thing is clear: a patient-centered, integrated approach that embraces both innovation and tradition holds promise for overcoming even the most intimidating hurdles. Future research, guided by the fine points of immunological science and the real-world experiences of patients, will continue to shape strategies that are as dynamic and multifaceted as the conditions they aim to treat.
Ultimately, the integration of apremilast into a broader therapeutic framework could mark the beginning of a new era in autoimmune disease management—one where precise, carefully considered treatments are customized to meet the nerve-racking challenges posed by overlapping conditions. As we take a closer look at these developments, it is essential that we keep an open mind, be willing to make incremental adjustments, and never lose sight of the ultimate goal: improving patient’s lives in a comprehensive and compassionate way.
This emerging perspective on managing overlapping autoimmune disorders reminds us that in the realm of modern medicine, every challenge—no matter how complicated the pieces—brings with it an opportunity for innovation, collaboration, and above all, hope. With continuous research, open dialogue among specialties, and an unwavering commitment to patient-centered care, the twists and turns of autoimmune disease management can transform from a nerve-racking maze into a bridge that leads to a better quality of life for countless patients.
Read more about this topic at
Innovative directions in immunotherapy research
Advances in Immunotherapy and Innovative Therapeutic …