When the Virus Meets the Bacteria: A New Frontier in Cancer Treatment
In recent years, the field of cancer treatment has witnessed some truly groundbreaking ideas. One such concept involves pairing cancer-killing viruses with genetically engineered bacteria in a bid to overcome some of the immune system’s tricky parts. This innovative strategy seeks to boost the effectiveness of oncolytic viruses—viruses that target and kill cancer cells—by using bacteria as a protective shield. In this opinion editorial, we take a closer look at how these two biological agents can work together to tackle severe tumours, weigh the benefits against potential risks, and explore what this means for the future of cancer therapy.
The idea may seem almost sci-fi in nature: a virus normally kept in check by the body’s own immune defenses is given a cloak of invisibility by bacteria, thereby allowing it to thrive long enough to attack cancer cells deep within the body. This approach not only challenges some of our established assumptions about immunotherapy and virotherapy but also opens up new roads for research into treatments that could someday be used beyond tumours near the body’s surface.
Understanding Oncolytic Viruses and Their Applications
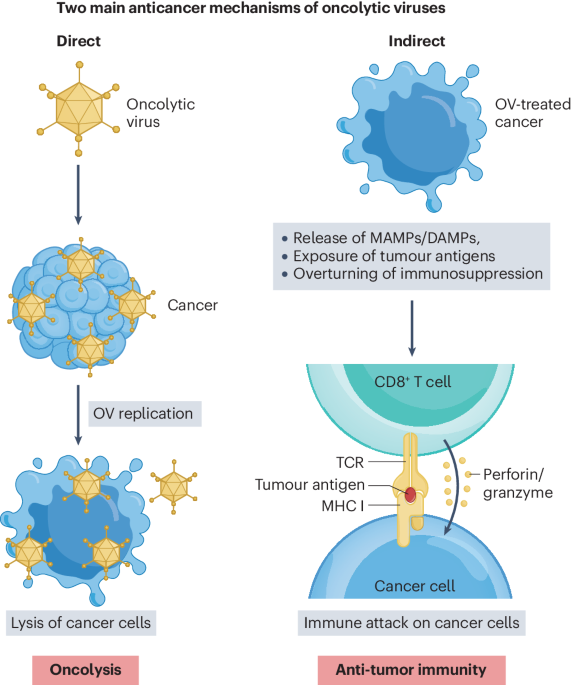
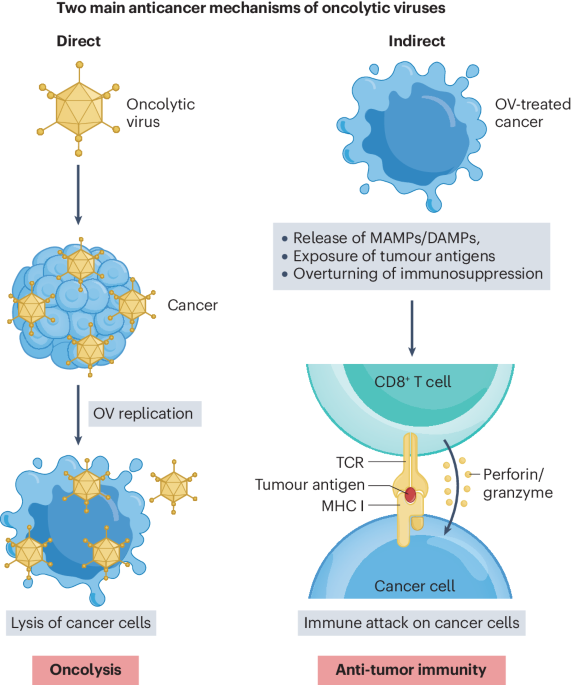
Before we dive in further, let’s take a closer look at what oncolytic viruses are and how they work in treating cancer. These viruses, which have been genetically modified to target tumours, are not new to clinical practice. Already approved for cancers of the skin, brain, and head and neck, they are injected directly into the tumour environment where they infect and burst cancer cells apart. This method exploits the natural ability of viruses to replicate, but engineering these viruses takes into account the fine points of their interaction with the human body.
The way oncolytic viruses function is straightforward but filled with little twists. They spread within the tumour, replicating until the cancer cells can no longer contain the viral infection. Once the cells burst, the immune system is alerted to the presence of the tumour, potentially igniting an immune response that further assists in controlling the cancer. In laboratory settings and initial clinical trials, these viruses have shown promise. However, their widespread application is often limited by the body’s own vigilant immune system, which sometimes stops the virus before it can sufficiently attack the cancer cells.
On a broader scale, these virus therapies represent a super important step in modern medicine. They are one of the more creative alternatives to conventional chemotherapy and radiation. By working with the body’s natural cellular mechanisms, oncolytic viruses deliver a targeted blow to cancer cells while sparing many of the healthy cells that are often collateral damage during standard treatments.
Boosting Efficacy Through Bacterial Shielding
A major limitation to virus-based cancer therapies is the immune system’s tendency to attack the virus before it can perform its intended function. This is where the innovative concept of shielding the viruses with genetically engineered bacteria comes in. Researchers have found that by effectively “masking” the virus with bacteria, the body’s defensive forces may be less likely to rapidly detect and neutralize the virus. In laboratory experiments involving mice, this clever pairing has resulted in delayed tumour growth in otherwise aggressive cancers.
This bacterial cloak acts as both a physical and biological cover, allowing the virus to penetrate deeper into tumours or even reach cancers located in more challenging areas. Imagine if you were sneaking through a heavily guarded building: a disguise might help you get past the watchful eyes long enough to complete your mission. Likewise, the bacteria provide the virus with a temporary shield, making it more effective in its task of killing cancer cells.
Critically, the bacterial component itself is not left unchecked. The bacteria used for these experiments are genetically altered to ensure that they do not cause additional harm to the patient. Instead, they are fine-tuned to resist detection without provoking a separate infection. The combination thus becomes a delicate dance: enough shield to mask the virus, but not so much as to create new complications.
Overcoming the Immune System’s Tricky Parts
In any discussion about viral therapies, one of the most challenging parts is finding a way to bypass the immune system. Our bodies are designed to identify and eliminate foreign invaders, which is excellent for fending off infections but problematic when introducing engineered viruses for therapeutic purposes. With the introduction of a bacterial shield, scientists have managed to work around some of these obstacles, essentially helping the virus find its way to cancer cells without being prematurely neutralized.
The immune system’s response is both a blessing and a curse. On one hand, its ability to recognize and attack foreign particles is crucial for fighting off infections; on the other, it becomes a barrier for therapies that require a temporary period of viral activity. By combining a virus with a supportive bacterial system, scientists have devised a method to slow down this immediate immune onslaught. This gives the virus a better chance of infiltrating tumours that might otherwise have been protected by rapid immune responses.
It is also important to appreciate that while this method shows promise in preclinical trials involving mice, significant work remains to fine-tune this interplay between the virus, bacteria, and immune system. Every patient’s immune profile is unique, and researchers find themselves working through many tangled issues before this approach can be widely adopted. As research continues, ongoing experiments and clinical trials need to address potential off-target effects and determine exactly how robust this bacterial shield could be in human subjects.
Exploring Animal Studies and Their Implications
The initial studies conducted on mice offer a fascinating glimpse into the future of cancer treatments. In these experiments, the genetically engineered bacteria did not just protect the virus; they actively contributed to a more effective attack on severe tumours. In essence, the virus had more time to spread, infecting cancer cells that are typically out of reach when administered alone. The beneficial outcomes observed in these studies have sparked enthusiasm in the broader oncology community.
When we look closely at the data from these animal studies, several key points emerge:
- The bacterial shield helps delay the immune system’s detection of the virus, allowing for deeper penetration into tumour cells.
- The combined therapy has shown a measurable slowdown in tumour growth compared with virus-only therapy approaches.
- Early results indicate that this approach could be particularly promising for cancers located in areas traditionally resistant to oncolytic virus therapy.
While these findings are encouraging, experts caution that translating success in mice to human patients is not a straightforward path. Human biology is riddled with tension and tiny twists that differ significantly from animal models. The immune system in humans is a maze of subtle details and conflicting signals, making the potential transition from animal studies to human therapies a formidable task.
One of the most important considerations for future studies is to determine not just if the shielded virus can slow tumour growth but also whether it can produce lasting remission and improve overall patient survival rates. Only through extended trials and rigorous clinical testing can researchers get into all the hidden complexities to chart a reliable course forward.
Combining Therapies: Integrating Viral and Bacterial Methods
There is a growing consensus in the medical community that combining different therapeutic techniques may provide much-needed breakthroughs in cancer treatment. The idea of teaming up viruses with bacteria is just one example of how interdisciplinary insights—spanning microbiology, genetics, and oncology—can create innovative solutions. When we consider the integration of therapies, several benefits come to light:
- Enhanced Delivery: The bacterial shield allows the virus to circumvent early immune detection, enhancing its delivery to cancer cells.
- Improved Efficacy: By extending the time window during which the virus remains active, the combined treatment can attack tumours more effectively.
- Synergistic Effects: The immune system, once alerted by the viable virus, might mount a more robust response that further aids in the destruction of cancer cells.
- Potential for Broader Applications: This method may eventually extend beyond surface-level tumours to target cancers in more internal organs.
These potential benefits are not without their own set of little details that need careful analysis. For instance, the interaction between the virus and the bacteria must be tightly controlled to avoid any unexpected repercussions. Researchers must figure a path through these complicated pieces, striking a balance between sufficient viral activity and maintaining patient safety.
Moreover, the integration of such therapies forces the scientific community to re-assess traditional boundaries between different treatment modalities. By combining a targeted viral approach with the strategic assistance of protective bacteria, a new paradigm in cancer care is emerging—one that is both creative and adaptable in the face of cancer’s many challenges.
Safety Considerations and Potential Side Effects
While the promise of a virus-bacteria combination therapy is exciting, it is also important to talk about the safety concerns and off-target effects that may come into play. Just like any innovative treatment, the method must be thoroughly vetted to ensure that it does not introduce new problems. The complexity of the human immune system means that even a well-designed bacterial shield could have unintended consequences.
Some of the key safety issues that researchers need to work through include:
- Immune Overreaction: There is a risk that altering the immune response may lead to an unintended and overwhelming reaction.
- Off-Target Infections: Even genetically engineered bacteria can sometimes behave in unexpected ways if they multiply beyond control.
- Long-Term Effects: Since this is a relatively new approach, the long-term systemic effects on the body remain an area of active investigation.
In response to these potential issues, scientists are designing multi-phase clinical studies that carefully monitor patient responses. Simultaneously, they are deploying advanced technologies to track how the engineered bacteria interact with both the virus and the host’s immune molecules. Tables like the one below can help summarize the balance between therapeutic potential and safety risks:
| Aspect | Potential Benefit | Possible Risk |
|---|---|---|
| Enhanced Viral Penetration | Deeper tumour infiltration | Delayed immune detection leading to infection spread |
| Bacterial Cloaking | Protection of the virus for uninterrupted action | Risk of bacterial overgrowth or off-target infections |
| Immune System Modulation | Triggering a more effective antitumour response | Potential to provoke overwhelming immune reactions |
Addressing these concerns is a nerve-racking task, but it is also essential for ensuring that any new cancer therapy can truly be considered safe and effective. Researchers advocate for a rigorous step-by-step process where each element of the treatment is carefully assessed for unintended interactions with the body’s natural defence systems.
Challenges and the Road Ahead: Working Through the Nitty-Gritty to Widespread Use
Even as promising as this virus and bacterial combination appears in laboratory settings, its clinical application in humans is full of problems and tiny twists. For instance, the immune systems of laboratory animals are not always the same as those in human beings, meaning that strategies that work well in mice might need significant adaptation for human therapies. This presents both a scientific and regulatory challenge.
Developing new treatments always involves working through some complicated pieces. There are several steps that the research community will need to address before adopting this approach on a broader scale:
- Extensive Clinical Trials: Before the treatment can be approved for widespread use, it must pass through multiple phases of testing that examine its safety, efficacy, and potential side effects in humans.
- Regulatory Approval: Governmental and international regulatory bodies will need to weigh in on the balance between the new method’s promise and the risks it might pose.
- Production Challenges: Manufacturing genetically engineered bacteria and viruses in a safe, consistent, and scalable manner poses its own set of tricky logistical issues.
- Patient-Specific Considerations: With the immune system acting as both friend and foe in these treatments, personalizing the approach to individual patients will be a key component of success.
The steps listed above are far from simple. They represent just a few of the little twists that researchers and clinicians must figure a path through before this promising treatment can be widely adopted in everyday oncology practice. Each stage of the process is imbued with its own set of challenges—ranging from technical difficulties in ensuring that the bacterial shield does not provoke an adverse reaction, to the rigorous demands of clinical trial protocols.
Despite these hurdles, the potential benefits justify the additional research and investment. As the scientific community continues to explore this innovative method, new insights will likely emerge that simplify these complications. At the same time, working through these challenges will require close cooperation among virologists, microbiologists, oncologists, and regulatory authorities. It is a multi-disciplinary effort that, if successful, could change the landscape of cancer treatment in the decades to come.
Implications for the Future of Cancer Therapy
The emergence of this combined approach offers a glimpse into a future where treatments are not limited by the traditional boundaries set by either the immune system’s rapid response or the sometimes insufficient potency of solo therapies. As we figure a path toward more holistic and integrated treatment strategies, evidence is building that a more nuanced understanding of the body’s immune functions may pave the way for unprecedented advances in cancer care.
This method encourages us to step away from the one-size-fits-all mentality and consider individualized treatment plans. By modifying both the virus and the bacteria to suit different tumour types and patient profiles, there is a possibility of a more personalized approach to cancer treatment. The bacteria act as adjustable “shields,” and the viruses as active agents targeting the malignancy—together forming a cooperative unit that can be modulated based on the unique needs of each case.
In practice, this could mean developing a platform where the therapy is continuously monitored and adjusted based on how the patient’s body responds. Future treatments might even combine this approach with other modalities such as immunotherapy, chemotherapy, and even alternative medicine practices that focus on boosting the body’s overall resilience. This integrated method promises to overcome some of the intimidating hurdles that have long hampered traditional therapies, offering renewed hope for patients with otherwise difficult-to-treat cancers.
Moreover, following this line of thinking, there is a significant potential for cross-disciplinary research that blends modern medical practices with insights drawn from alternative medicine and nutrition. For instance, certain nutritional protocols might improve the body’s tolerance for bacterial elements, or lifestyle modifications could complement the biological treatment, ensuring that patients are in the best possible shape to benefit from the therapy. Such an integrative approach aligns with current trends in medicine that advocate treating the whole patient, rather than just targeting the tumour.
Integrating Modern Medicine with Alternative Perspectives
The promise of shielded virus therapy also raises interesting questions about how modern and alternative medicine can intersect. While modern research is focused on genetic engineering and targeted therapies, alternative medicine emphasizes balance, dietary interventions, and stress reduction. By taking a closer look at both perspectives, we might unlock strategies that address the body’s tricky parts in more than one way.
Some professionals suggest that incorporating nutritional strategies, supplements, or even specific fitness regimens could potentially enhance how well a patient’s immune system supports rather than fights the therapeutic virus-bacteria combination. Although much of this remains speculative at this stage, future studies might find it critical to consider these subtle differences in patient care. The combination of hard science and alternative therapeutic measures could lead to protocols that are even more effective and better tolerated by patients.
For example, a few emerging ideas include:
- Dietary Adjustments: Specific diets rich in antioxidants or anti-inflammatory agents might help modulate the immune response, giving the viral therapy a better chance to work.
- Mind-Body Interventions: Techniques such as meditation or controlled breathing could reduce stress hormones that might otherwise compromise immune regulation.
- Personalized Fitness Plans: Exercise regimens tailored to improve circulatory and immune functions may help patients better handle the treatment while promoting overall wellbeing.
These integrated approaches are not here to replace the cutting-edge biological treatments but rather to complement them. As research advances, the boundaries between conventional medical treatments and holistic, alternative practices might become less defined, allowing for more comprehensive patient care. After all, when treating a condition as critical as cancer, every additional strategy is worth consideration.
Patient Perspectives and Quality of Life Considerations
No discussion of any new treatment can be complete without considering the patient’s experience. While the technical aspects are crucial, the overall quality of life for those undergoing treatment is equally important. Many patients find traditional therapies, such as high-dose chemotherapy or invasive surgeries, off-putting because of the severe side effects and long recovery times. In contrast, targeted therapies like oncolytic viruses, especially when enhanced with a protective bacterial shield, have the potential to be much less frightening in terms of side effects.
Although the idea of introducing viruses and bacteria into the body might sound intimidating at first, many experts believe that these therapies can be designed to minimize collateral damage. In this context, quality of life improvements include:
- Reduced Systemic Side Effects: Targeted delivery means that fewer healthy cells are affected by the treatment, potentially leading to fewer adverse reactions.
- Faster Recovery Times: With less damage to normal tissue, patients could see quicker recoveries compared to more aggressive treatments.
- Personalized Treatment Protocols: Developing therapies that are tailored to individual patient profiles can increase effectiveness while minimizing discomfort.
This approach is also likely to help patients maintain a sense of hope and empowerment. By giving them treatments that are less disruptive to daily life and less nerve-racking than traditional chemotherapy regimens, medical practitioners can support both the physical and emotional aspects of cancer recovery.
The use of combined viral and bacterial therapies could mark a significant shift in how patients view cancer treatments. Instead of the often overwhelming feeling of facing a monster with many tangled issues, patients may begin to see a future where their treatment is as adaptive and multi-faceted as the disease itself. This change in approach—where hope is built not solely on the aggressive elimination of cancer, but on a finely tuned and patient-friendly strategy—could be a turning point in oncology care.
Looking Forward: The Future Landscape of Cancer Treatment
The intersection of virotherapy and bacterial shielding represents a compelling evolution in the fight against cancer. As researchers continue to test and refine this combination, several long-term trends may shape its success:
- Personalized Medicine: Advances in genomic profiling and personalized diagnostics will enable doctors to select and tailor treatments based on a patient’s unique immune makeup and tumour characteristics.
- Interdisciplinary Collaboration: The merging of modern medicine with nutritional science, alternative therapies, and sophisticated genetic engineering may open up new treatment avenues that surpass current limitations.
- Improved Monitoring Techniques: New imaging and biomarker technologies will help clinicians get into the hidden complexities of each patient’s response, allowing for finer adjustments throughout the treatment process.
- Regulatory Innovations: As these therapies evolve, regulatory standards will adapt to better ensure both efficacy and safety while encouraging innovation in cancer treatment.
One can envision a future where cancer treatments are part of a larger network of patient care that routinely includes virus-bacteria therapies integrated with lifestyle interventions and supportive alternative medicine practices. Such a future not only promises improved survival rates but also aims to keep the patient’s overall wellbeing front and center throughout the journey.
As with any new treatment pathway, caution remains essential. Researchers, clinicians, and patients all have roles to play in monitoring how these therapies are deployed and adjusted over time. Just as the immune system has its own tricky parts that must be carefully managed, so too must the medical community work through each of the intricate steps involved in bringing these treatments safely from the laboratory to the clinic.
Concluding Thoughts: Balancing Innovation with Prudence
In our pursuit of more effective and less invasive cancer treatments, the marriage between virus-based therapies and bacterial shielding stands out as a transformative concept. It represents a smart way to get around the overwhelming defensive measures of the immune system while delivering a potent, targeted attack against cancer cells.
However, this innovative strategy is not without its risky turns and challenging bits. The balance between efficacy and patient safety is delicate, and the transition from promising animal studies to broad human application is laden with both opportunities and challenges. Careful, methodical clinical research will be essential to address the unpredictable interactions between immune responses, engineered biological agents, and patient diversity.
What remains clear is that the future of cancer treatment is likely to be built on such integrative approaches—ones that combine modern medicine with alternative perspectives and nutritional insights for a more holistic form of care. By learning to work through the subtle details and less obvious twists of our own biology, the scientific community is charting a new roadmap for cancer therapy that could ultimately empower patients and improve quality of life.
As we take a closer look at these developments, it is important to remember that the path to innovative cancer treatment is a journey filled with trial, adjustment, and collaboration. The virus-bacteria approach is not a magic bullet, but it is a promising step toward new strategies that could one day make a profound difference. With continued research, interdisciplinary dialogue, and a shared commitment to finding better solutions for patients, we can hope that the coming years will bring treatments that are both highly effective and significantly gentler on those who need them most.
Ultimately, the next few years will be crucial. As scientists and clinicians figure a path through the tangled issues of immune modulation and therapeutic delivery, the lessons learned will not only benefit those with cancer but could also pave the way for other treatment modalities that pair biological innovation with patient-centered care. This is an exciting time for the field—a time when the challenges of today may soon transform into the standard of care tomorrow.
In sum, the evolving story of virus-based cancer therapy, bolstered by bacterial shielding, exemplifies humanity’s boundless capacity for innovation in the face of serious diseases. While many of the details remain to be fine-tuned, the promising results observed so far provide a strong foundation for optimism. With each step forward, this combined approach brings us closer to a future where cancer is not only treatable but managed in a way that preserves both life and quality of life.
As we watch these advances, both practitioners and patients are encouraged to remain informed, engaged, and hopeful—knowing that today’s experimental research may soon transform into the next generation of cancer care. The road ahead is long and filled with minor twists and tricky parts, but the collective drive for better treatments serves as a constant reminder that progress is always possible, even in the face of daunting challenges.
It is my hope that by working side by side—researchers refining vaccine-like precision, doctors adapting treatments to individual needs, and patients embracing new possibilities—we will continue to witness a revolution in how cancer is treated. Already, the promise of a shielded, virus-based therapy holds the potential not only to extend lives but to improve day-to-day experiences in ways that were once thought impossible.
Let us then champion innovation tempered by caution, and progress guided by the core principle of patient care. As the science evolves, so too will our understanding of how best to use these powerful biological tools. In the end, the ultimate goal remains clear: to transform cancer from a devastating diagnosis into a manageable condition, bolstered by the combined forces of modern medicine, genetic engineering, and an ever-deepening knowledge of the body’s own remarkable defenses.
Originally Post From https://www.newscientist.com/article/2492641-cancer-killing-virus-becomes-more-effective-when-shielded-by-bacteria/
Read more about this topic at
Synergism and Antagonism of Bacterial-Viral Coinfection in …
Mechanisms of synergy in polymicrobial infections – PMC