Bridging the Gap in HER2 Therapy: A Critical Look at Breast Cancer Care Disparities
Recent research has brought to light some concerning gaps in the accessibility of HER2-targeting therapies for patients with hormone receptor-negative (HR–) and HER2-positive (HER2+) breast cancer. While these treatments have been proven to improve survival dramatically, it appears that nearly 25% of eligible patients are not receiving them. In this opinion editorial, we take a closer look at the findings, discuss the underlying issues, and suggest practical steps that clinicians, healthcare facilities, and policymakers can take to mitigate these disparities.
The data, drawn from a large retrospective cohort study, highlight that only about 75% of patients with metastatic HR–/HER2+ breast cancer receive HER2-targeted therapy. Given the proven survival benefits—improving median survival from approximately 1.3 years to over 5 years—the fact that one in four patients is not receiving guideline-recommended therapy is both concerning and a call for immediate action.
Unequal Access: Hidden Barriers in HER2-Targeting Treatments
One of the most startling revelations is the uneven access to life-extending HER2 therapies. The study shows that patients from rural areas, those on Medicare, patients of older age, and Black patients are less likely to receive these treatments. This gap in care points to the hidden barriers that are preventing equitable access to advanced therapies.
Several intertwined issues contribute to these disparities:
- Geographical challenges: Rural treatment centers may lack the specialized resources needed to administer newer therapies.
- Insurance limitations: Patients with Medicare or limited insurance options might face higher out-of-pocket costs or more restrictions, deterring optimal therapy use.
- Sociodemographic factors: Racial disparities further complicate the picture, suggesting that broader issues of systemic inequality are at play.
When we examine these factors, it becomes clear that the problem is multi-layered. The hidden barriers affecting treatment access demand a comprehensive strategy to ensure that advances in medical science benefit all patients, regardless of their socioeconomic or geographic status.
Insurance and Facility Differences: The Fine Points of Treatment Uptake
The study emphasizes that having private insurance and being treated at academic or specialized centers is strongly linked with an increased likelihood of receiving HER2-targeted therapies. This observation brings to the forefront the fine points related to insurance coverage and facility capabilities.
For many patients, the type of insurance they hold can make a critical difference. Private insurance often provides easier access to advanced treatments compared to public options like Medicare. More specifically, the data indicates an odds ratio (OR) of 1.76 for patients with private coverages, which translates into a significantly greater likelihood of receiving the appropriate therapy compared to those without it.
Academic facilities, too, play a crucial role in this equation. Centers with robust research programs and more comprehensive oncology services are often the first to adopt new treatments and offer them to patients. With an OR of 1.39 associated with academic facilities, the study underscores that the expertise and resources available at these centers are vital. This disparity suggests that patients treated at non-academic centers might need extra support to access these life-saving therapies.
Rural vs Urban Disparities: The Nitty-Gritty of Geographical Influences
Geography is another major factor that shapes treatment patterns in metastatic HER2+ breast cancer. Rural facilities often face unique challenges that can hinder the delivery of cutting-edge therapies.
In rural settings, the availability of specialized medical care can be limited. Smaller hospitals and clinics, while offering excellent general care, may not have the specific expertise or infrastructure that urban academic centers do. The study found that patients treated in rural facilities had a 41% lower odds (OR 0.59) of receiving HER2-targeted therapies compared to those in urban or academic centers.
This discrepancy is not just a statistical figure; it reflects real-world challenges where patients living in less accessible areas face additional, sometimes intimidating, hurdles in their cancer care pathway. The limited availability of specialists, fewer clinical trial opportunities, and potential delays in diagnosis all contribute to these geographical inequities.
Age, Race, and Other Subtle Details in Therapy Utilization
In addition to insurance and geographic location, patient-specific factors such as age and race play a significant role in determining who receives HER2-targeted therapy. The study illustrates that older patients and Black patients are less likely to benefit from these interventions. With an odds ratio of 0.52 associated with age and 0.78 for Black race, the data are clear: there are subtle yet critical distinctions in treatment patterns that must be addressed.
Older patients may face a combination of medical and social challenges that make clinicians more cautious in prescribing aggressive treatments. Concerns about comorbidities, reduced tolerance to treatment, and the potential for side effects can lead to a more conservative approach. However, withholding effective treatment solely based on age is fraught with problems. Every patient deserves a careful assessment that balances the potential benefits and risks.
Similarly, the lower utilization among Black patients points to systemic issues that extend beyond individual clinical decisions. It raises uncomfortable questions about potential biases, cultural differences in healthcare access, and the need for enhanced outreach programs to minority communities. These subtle details and fine points of care must be addressed to ensure that every patient, regardless of their background, has equal access to life-saving treatment.
Policy and Intervention Strategies: Finding a Path Through Treatment Barriers
The study’s findings call for immediate policy interventions aimed at reducing the treatment gap. Crafting policies that directly target the barriers faced by underserved populations is super important. Here are some potential strategies:
- Improving Insurance Coverage: Expanding the coverage options and reducing the patient’s financial burden in public insurance plans like Medicare could help reduce disparities.
- Enhancing Rural Healthcare Resources: Investing in advanced training for rural healthcare providers and facilitating partnerships between urban academic centers and rural clinics could allow for better sharing of expertise and resources.
- Cultural Competence Training: Implementing programs to address potential implicit biases and ensure culturally sensitive care could improve treatment uptake among minority populations.
- Patient Education and Outreach: Community-based initiatives can empower patients by educating them about the benefits of HER2-targeted therapies, thereby encouraging them to seek appropriate care.
Each of these strategies requires coordinated efforts from federal and state governments, healthcare institutions, and advocacy groups. By ensuring that policies are focused on reducing the tangible barriers highlighted in the study, we can work toward a more equitable healthcare system where advances in cancer treatment benefit everyone.
Medical Advancements Versus Real-World Reality: The Big Picture
The evolution of HER2-targeted therapies represents one of the most significant advances in breast cancer treatment in recent decades. For many patients, these therapies have transformed a once grim prognosis into one where survival is measured in years rather than months. Yet, the big picture remains that scientific progress does not automatically translate into universal care.
On one hand, the rapid adoption of these therapies from 2013 to 2016 demonstrates an impressive uptake in certain patient populations. The numbers show an increase from 64.6% utilization in 2013 to an impressive 80.9% in 2016—a period marked by swift progress and broad recognition of the treatment’s benefits.
On the other hand, the slight decline and stabilization around 75% after 2019 imply that progress can stall when the underlying issues of inequitable access are not addressed. Even as the latest research points to an average increase in overall utilization, we must remain vigilant about persistent barriers affecting the most vulnerable groups.
This situation is a classic example of the twists and turns inherent in healthcare innovation. Scientific breakthroughs are full of promise, yet the almost tangled issues of real-world application—insurance hurdles, geographical discrepancies, and sociodemographic differences—slow down overall progress. The challenge is to bridge the gap between clinical success and equitable care delivery, ensuring that no patient is left behind due to these confusing bits of systemic inequality.
Practical Steps for Clinicians and Policy Makers
Given the study’s findings, it is essential for both clinicians and policymakers to consider actionable steps that can address these barriers head-on. Here are some practical recommendations for stakeholders in the healthcare system:
For Clinicians and Healthcare Providers
- Regular Training: Healthcare providers should engage in ongoing professional development to stay current with the latest treatment protocols and guideline-recommended therapies. Workshops and conferences can provide opportunities to learn about the subtle parts of patient communication, helping physicians tailor their discussions to address patients’ concerns and potential barriers.
- Comprehensive Patient Evaluations: Clinicians need to ensure that every patient is evaluated fairly, considering both their clinical profiles and their socioeconomic backgrounds. While older patients may present an intimidating array of comorbidities, treatment decisions should be personalized to balance benefits and potential risks. Age should not be a deterrent to offering life-saving therapies.
- Facilitating Access to Specialist Services: For patients in rural areas or at non-academic centers, referrals to specialized oncology centers can make a substantial difference. Telemedicine can serve as an effective tool to “find your way” through the tricky parts of geographical constraints and provide remote consultation with experts.
- Patient Advocacy: Providers should take an active role in educating their patients about available treatment options. Clear communication about the potential benefits and side effects of HER2-targeted therapies can empower patients to make informed decisions.
For Healthcare Administrators and Policy Makers
- Invest in Infrastructure: Allocating more resources to rural healthcare systems can help close the gap between rural and urban treatment facilities. Investments in technology, training, and specialist support are essential for enhancing treatment accessibility.
- Enhance Insurance Policies: Revising insurance policies, particularly for public programs, to include broader coverage for advanced cancer therapies can significantly reduce the financial burden on patients. Streamlined reimbursement processes and reduced co-payments should be made a priority.
- Foster Collaborative Networks: Encouraging partnerships between academic centers and smaller facilities can promote the sharing of knowledge and technological advancements. Cross-institutional collaborations can help smaller clinics access expert guidance on administering new treatments.
- Launch Awareness Campaigns: Public health campaigns focused on educating patients about the benefits of HER2-targeted therapies can dispel myths and encourage more patients to seek out these treatments. Such campaigns should be culturally tailored and target communities that have historically been underserved.
Policy changes should not only address the financial and infrastructural aspects but also the underlying social and racial disparities. A multi-faceted approach that considers the human, systemic, and economic factors can lead to more effective and enduring changes in how breast cancer care is delivered.
Evaluating the Impact of HER2-Targeted Therapies: A Closer Look at the Data
It is crucial to take a closer look at the data presented in the study to understand the impact of HER2-targeted therapies. The research shows that patients who received these therapies experienced a median survival of around 5.08 years compared to just 1.27 years for those who did not. Such stark differences underscore the value of these treatments.
An analysis of the numbers reveals several key points:
| Factor | Odds Ratio (OR) | Impact on Treatment Uptake |
|---|---|---|
| Private Insurance | 1.76 | Significantly higher uptake |
| Treatment at Academic Facilities | 1.39 | Enhanced likelihood of receiving therapy |
| Diagnosis Year (2016-2018) | 1.93 | Rapid increase in therapy usage |
| Diagnosis Year (2019-2020) | 1.88 | Sustained, but slightly declining use |
| Rural Facility | 0.59 | Lower utilization |
| Black Race | 0.78 | Lower odds of receiving treatment |
| Medicare Insurance | 0.64 | Reduced uptake compared to private insurance |
| Older Age | 0.52 | Significantly decreased odds of therapy use |
This table not only organizes the data but also provides a visual aid to understand the nuanced issues associated with treatment disparities. Each figure represents a fine shade of the overall picture—a picture that is as revealing as it is concerning.
Socioeconomic Influences and Their Ripple Effects on Patient Care
Beyond the numbers, it is important to acknowledge how socioeconomic factors subtly influence treatment decisions. For many patients, the financial cost of care is an off-putting barrier that can result in delayed or denied treatment. When coupled with limited access to information, patients may inadvertently miss out on life-saving opportunities.
Consider how socioeconomic status impacts patient care:
- Financial Burden: Out-of-pocket expenses for advanced cancer therapies can be overwhelming and may discourage patients from pursuing optimal treatment options, even if they are clinically appropriate.
- Limited Health Literacy: Patients with lower health literacy may not fully understand the benefits of HER2-targeted therapies, making them less likely to ask for or consent to such treatments.
- Access to Specialized Care: Individuals in lower-income areas might have to travel long distances or rely on under-resourced local facilities for specialized oncology services.
These socioeconomic factors create a ripple effect, negatively impacting treatment outcomes. Addressing financial constraints through better insurance coverage and patient support programs is key. Additionally, increasing patient education can help demystify the benefits of HER2 therapies, making sure that misinformation does not further widen the care gap.
Overcoming the Overwhelming: Strategies for a More Equitable Future
Facing the array of issues surrounding HER2 therapy disparities can feel overwhelming—a true nerve-racking situation for many in the healthcare community. However, every challenge poses an opportunity for growth and improvement. By addressing each of the smaller, confusing bits of the problem, we can start to piece together solutions that work for everyone.
Here are some strategies to overcome the current barriers:
- Strengthen Community Outreach: Healthcare institutions and community leaders can collaborate to host informational sessions, ensuring that the benefits of HER2-targeted treatments are well known in underserved communities.
- Telemedicine Expansion: As technology advances, telemedicine represents a practical approach to help patients in remote areas get specialist consultation without the daunting need to travel long distances.
- Enhanced Provider Training: Regular workshops on cultural competence and patient communication can help clinicians appreciate the little twists in each patient’s situation, tailoring their approach to address unique barriers to care.
- Streamlined Referral Systems: Implementing efficient referral processes can ensure prompt transfer of high-risk patients from rural or non-specialized facilities to centers with advanced treatment options.
Each of these strategies, while addressing a specific problem, contributes to the larger goal of creating an equitable healthcare delivery system. The clear takeaway is that, although the advances in HER2-targeted therapies are a beacon of hope, broadening their reach requires concerted, multi-pronged efforts.
Learning from Progress: The Road Ahead in Breast Cancer Care
The evolution of HER2-targeted therapies in metastatic HR–/HER2+ breast cancer has been nothing short of revolutionary. Yet, as the journey continues, we are reminded of the twists and turns in the path to equitable care. The progress made from 2013 through 2016, along with the slight plateau in uptake thereafter, suggests that while strides have been made, the work is far from complete.
We must learn from the way these therapies have been adopted and consider how best to extend their benefits to the entire patient population. The small distinctions in treatment uptake—whether driven by insurance status, geographical location, age, or race—are a call to action for more personalized and inclusive approaches to healthcare delivery.
Moving forward, healthcare providers must continue to refine their approach, making every effort to educate and advocate for their patients. This means not only being aware of the latest clinical guidelines but also recognizing and actively addressing the subtle parts of each patient’s social and economic background that might affect their care.
Closing Thoughts: The Imperative of Collaborative Change
In conclusion, the disparities observed in HER2-targeted therapy usage are both a challenge and an opportunity. With only 75% of eligible patients receiving these transformative treatments, there is a clear need for change. Whether it is through strengthening insurance policies, improving access to advanced care in rural areas, or addressing the subtle details that influence treatment decisions for older and Black patients, the path forward must be multi-faceted and inclusive.
It is super important for all stakeholders—clinicians, healthcare administrators, policymakers, and patient advocates—to work together in addressing these barriers. Only by pooling our resources, knowledge, and resolve can we ensure that every patient with HER2-positive breast cancer has the chance at a better, longer life.
This editorial is a call to arms for us all. We must recognize that the evolution of medical treatments is only as valuable as their accessibility. As we stand on the brink of further innovations in cancer care, let us not allow progress to be derailed by inequalities that are, in many cases, entirely preventable.
By taking decisive action and implementing targeted strategies, we can start to erase the confusing bits that currently separate optimal care from inadequate treatment. The future of breast cancer care depends not only on scientific breakthroughs but also on our collective commitment to making these breakthroughs available to every patient.
Looking Forward: Embracing the Future of Equitable Healthcare
While advancements in HER2-targeted therapies have undoubtedly revolutionized treatment outcomes, the challenge now lies in ensuring that these life-enhancing treatments are distributed fairly and efficiently. The data clearly indicate profound disparities, which serve as a reminder that the trickier parts of healthcare delivery—such as tailoring treatment choices to the socio-demographic context—cannot be overlooked.
Future research should continue to track usage patterns and focus on the subtle parts of patient care that contribute to these disparities. Clinicians and administrators must collaborate, share best practices, and pilot innovative programs that address the root causes of inequitable treatment distribution. Only by working together can we make sure that every eligible patient receives critical, guideline-recommended therapy that could extend their lives.
It is also essential to foster an environment in which lessons learned from current challenges inform future approaches. As the healthcare landscape evolves, maintaining flexibility and openness to change will be must-have attributes for every stakeholder in the system.
Key Takeaways and Final Reflections
To summarize the main points discussed:
- Only about 75% of eligible metastatic HR–/HER2+ breast cancer patients are receiving life-saving HER2-targeted therapies.
- Factors such as private insurance, treatment at academic centers, and more recent diagnosis years are positively associated with higher therapy uptake.
- Rural treatment settings, older age, Black race, and reliance on Medicare are linked to lower odds of receiving these therapies.
- Policy interventions, improved insurance coverage, enhanced outreach, and provider training are essential strategies toward bridging this gap.
- Addressing these issues requires coordinated efforts across multiple layers of the healthcare system, from individual clinicians to policy makers.
The survival benefit provided by HER2-targeted therapies is undeniable, yet the uneven uptake across different patient demographics signals a pressing need for reform. The lessons from this study should serve as a roadmap for future:
- System-wide interventions to improve equitable access to advanced treatments.
- Collaborative initiatives between urban academic centers and rural healthcare facilities.
- Robust educational programs for both patients and healthcare providers to dispel myths and encourage informed decision-making.
Ultimately, the challenge before us is one of balancing remarkable medical progress with the practical realities of how healthcare is delivered. It is imperative that we tackle the intimidating barriers—be they financial, geographical, or sociodemographic—that prevent every eligible patient from receiving the critical treatment they deserve.
As we look to a future where medical breakthroughs continue to transform lives, let us also commit to making these innovations accessible to all. The health and survival of countless patients depend on our ability to resolve these tangled issues and chart a course toward more inclusive, equitable care for everyone.
The journey ahead may be filled with twists and turns, but the destination—a world where every patient can access the best that modern medicine has to offer—remains within reach. By recognizing and addressing the hidden, fine points of current disparities, we can transform challenges into opportunities for growth, collaboration, and, ultimately, better patient outcomes.
In closing, while the progress in HER2-targeted treatments is encouraging, it also brings to light the pressing need for a more equitable healthcare system. The time has come for us to work together, break down the barriers that hinder access, and ensure that groundbreaking therapies benefit every patient irrespective of their background or where they reside. Let us seize this opportunity to make meaningful change and pave the way for a healthier future for everyone battling breast cancer.
Originally Post From https://www.pharmacytimes.com/view/study-reveals-alarming-gaps-in-her2-therapy-access-for-patients-with-breast-cancer
Read more about this topic at
ABC5: Patients with advanced breast cancer are being …
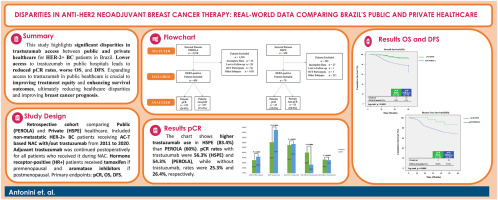
BRaziLian outcomE for metAStatic breasT Cancer