Unplanned Acute Care in Cancer Patients: A Closer Look at Pre-Visit Symptoms
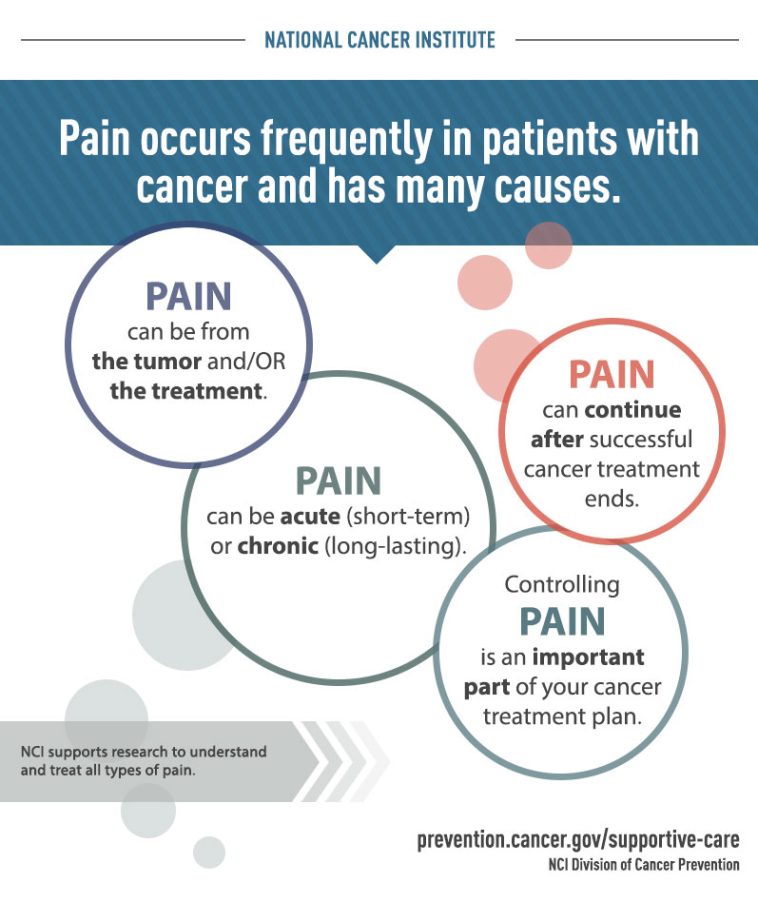
The world of oncology is full of tricky parts and tangled issues, especially when it comes to managing the symptoms that lead to unplanned acute care visits. Recent research has shown that pain, nausea, and vomiting are among the most common signs documented in cancer patients before they have to make an acute visit to the emergency department (ED) or get hospitalized. In this opinion editorial, we take a closer look at this study’s findings, explore what they reveal about the little details of symptom management, and discuss how these insights could steer the healthcare community in addressing disparities in symptom documentation.
Understanding and resolving the obstacles involved in acute care for cancer patients is not only essential for improving patient outcomes and quality of life, but it also comes with its own set of nerve-racking challenges in managing healthcare costs. With a focus on the key complexities that this new study has brought to light, we will dive into the subject matter using natural language processing (NLP) and sociodemographic correlations.
Key Findings and Their Implications in Cancer Symptom Documentation
The study observed 70,606 acute care encounters across a large cohort of over 28,000 adult cancer patients. Researchers used advanced NLP methods to scan the clinical notes written in the 30 days before the acute care visit. With more than 854,000 symptom entries recorded, the data provided an in-depth look into the symptom burden that patients have before seeking acute care.
Using Natural Language Processing in Healthcare Symptom Analysis
The use of natural language processing in this study was designed to get into the nitty-gritty of clinical documentation. NLP helped in identifying more than 10 different symptoms per patient in some cases, a marker that the researchers used to define high symptom burden. The technology proved invaluable for scanning large volumes of text and uncovering subtle parts of patient records that might otherwise have remained hidden. However, there are a few complicated pieces associated with this process:
- Potentially incomplete data due to retrospective study design;
- Limitations in capturing all the twists and turns in clinical notes;
- Risk of bias from repeated visits by the same patients;
- The predominance of a mostly White and insured study population, hindering the generalizability of the findings.
These factors mean that while NLP offers a promising tool for understanding symptom documentation, healthcare professionals need to be mindful of its potential shortcomings. This study serves as both a breakthrough and a reminder of the confusing bits involved in harnessing technology for clinical research.
Symptom Patterns and Their Relationship With Patient Demographics
Delving into the study’s data reveals that certain groups are more prone to having a high symptom burden before acute care visits. For instance, women, individuals from racial minority groups, and patients with Medicaid insurance were more likely to have a record of more than 10 different symptoms. In contrast, men and White patients actually accounted for the majority of the acute care encounters. This observation brings to the forefront the many tangled issues related to racial, sex, and socioeconomic disparities in healthcare.
Below is a simplified table summarizing the key demographic associations found in the study:
| Demographic Group | Adjusted Odds Ratio (aOR) | Interpretation |
|---|---|---|
| Women | 1.14 | Slightly higher likelihood of high symptom burden |
| Asian | 1.22 | Increased chance compared to baseline |
| Black | 1.17 | Moderate increase in symptom documentation |
| American Indian or Alaska Native | 1.21 | Elevated risk of high symptom burden |
| Medicaid-insured patients | 1.10 | Slightly more likely to report a high number of symptoms |
| Patients aged 65 or older | 0.96 | Slightly less likely to have multiple symptoms |
| Patients without insurance | 0.58 | Significantly less likely to have documented multiple symptoms |
This table not only acts as a quick reference to the fine points of the study’s findings but also emphasizes the subtle parts of the data that point to obvious disparities. It is clear that while many patients share the same acute care needs, their journeys to those emergency encounters are very different, marked by socioeconomic and racial factors that must be addressed in future interventions.
Disparities in Symptom Reporting: Are We Missing the Full Picture?
It is both critical and challenging to understand the implications of these findings. The fact that certain groups are more likely to have a high symptom burden before seeking acute care suggests that there may be underlying issues tied to access, communication, and the overall management of cancer-related symptoms. When juggling these myriad issues, healthcare providers must work through a host of confusing bits and little details to fully understand and address the root causes.
Identifying Socioeconomic and Racial Gaps in Cancer Symptom Management
The disparities in symptom documentation are not just statistical anomalies; they represent real differences in patient experiences. Women and racial minorities who are documented to have higher symptom burdens may be facing extra challenges such as:
- Reduced access to timely primary and supportive cancer care;
- Language and cultural barriers that may impair effective communication with healthcare providers;
- Economic and logistical obstacles that delay treatment, thus increasing the number of symptoms recorded before acute visits;
- Potential bias in how symptoms are recorded or interpreted by clinicians.
This growing list of concerns highlights the need for better-targeted interventions to ensure all patients receive adequate care. For example, establishing better support systems and outreach programs in minority and low-income communities could be super important in ensuring early symptom management and potentially reducing the number of unplanned acute care visits.
Potential Strategies to Address Documentation Inequities
If we are to effectively tackle the challenges posed by these disparities, healthcare systems must consider several strategies. Below is a bulleted list of possible interventions:
- Training clinicians on cultural sensitivity and bias reduction in symptom documentation;
- Implementing standardized symptom assessment tools to reduce variation in reporting;
- Expanding the reach of healthcare services, especially in underrepresented areas;
- Using patient-reported outcome measures (PROMs) in clinical settings to capture experiences more accurately;
- Improving integration of health information systems to allow real-time monitoring of patient symptoms.
These next steps could not only help reduce the number of unplanned acute care visits but also ensure that the unique needs of every patient are met—a super important goal for modern cancer care.
Exploring the Role of Technology: Natural Language Processing in Cancer Care
One of the standout features of the study is its use of natural language processing to scan clinical notes for symptom documentation. This technological integration opens up a new realm of possibilities, even if it is loaded with problems when it comes to accurately capturing the many twists and turns of clinical language.
How NLP is Changing the Game in Healthcare Documentation
NLP technology can process large volumes of textual data far faster than a human reviewer could. By applying algorithms to extract key symptoms from unstructured clinical notes, researchers are now able to identify trends that were once almost impossible to get a grasp on. Not only does this allow for a more comprehensive view of patient care, but it also helps in pinpointing areas where the healthcare system could improve its response.
The benefits of implementing NLP are multifold:
- Time efficiency in processing big data
- Enhanced accuracy in spotting patterns across thousands of clinical notes
- Ability to standardize symptom documentation across different providers
- Facilitating a better understanding of how certain symptoms precede emergency visits
However, even with these advantages, clinicians and administrators must acknowledge the intimidating challenges that come with integrating such a tool into everyday practice. For instance, NLP might miss the subtle details or little twists in a patient’s narrative that a well-versed clinician wouldn’t. Therefore, technology should complement human review rather than replace it entirely.
Limitations of Relying on NLP for Clinical Research
While NLP has proven to be an invaluable asset in this study, it is important to recognize that its application in healthcare data analysis is not without its nerve-racking side effects. Some of the challenges include:
- Difficulty in interpreting context-sensitive language or idiomatic expressions in clinical notes
- Potential underestimation or overestimation of symptom severity due to automated misclassification
- Issues with data consistency and completeness, as many clinical notes may have varying levels of detail
- Even subtle differences in phrasing can lead to inaccuracies when scaled across thousands of patient encounters
This cautionary perspective reminds us that, while technology provides powerful tools, the human element remains critical. It takes a collaborative effort between technology and clinical expertise to ensure that the data is interpreted in a way that truly benefits patient outcomes.
Implications for Clinical Practice and Future Interventions
The findings of this study extend far beyond academic interest. They interact deeply with everyday clinical practice and highlight pathways toward improvement in both patient care and the efficiency of hospital operations. With the new insights gained from this research, health professionals can figure a path to provide better care for those most in need.
Strategies for Better Symptom Management in Oncology Patients
Given that pain, nausea, and vomiting are leading symptoms that prompt emergency care, it is super important for clinicians to recognize these early notice signals. Doing so will allow healthcare providers to intervene before these symptoms escalate to a point where acute care is the only option. Strategies to achieve this include:
- Regular symptom screening during routine oncology visits
- Enhanced patient education on early symptom warning signs
- Personalized care pathways that consider socioeconomic and cultural contexts
- Integration of telehealth solutions for remote monitoring, especially for those distant from major healthcare centers
- Streamlining communication between patients and healthcare staff to swiftly address problematic symptoms
By taking these steps, clinicians can not only address the immediate symptom burden but also improve long-term outcomes in cancer care. This approach is all about getting into the fine details and little twists of patient care before problems compound into a full-blown crisis.
Addressing the Healthcare Disparities Revealed by the Study
As the study indicates, there is a clear discrepancy in the documented symptom burden among different patient demographics. For women, racial minorities, and Medicaid recipients, the higher likelihood of experiencing multiple symptoms calls for an equally robust response from the healthcare system. Some recommendations include:
- Developing community outreach programs that target vulnerable groups and emphasize early symptom management
- Enhancing access to supportive care services, including pain management clinics and counseling services
- Increasing funding and research into disparities in healthcare to build more inclusive treatment models
- Offering additional training in cultural competence for healthcare providers to reduce unconscious bias in documentation
- Ensuring that patient communication is clear and that follow-up care is accessible and understandable for all groups
Addressing these disparities is not just a matter of fairness; it has a direct impact on patient survival and quality of life. It represents an opportunity to make a real difference in the lives of those for whom the healthcare system has often been overwhelming and off-putting.
Delving Into the Real-World Impact on Patients’ Lives
The study’s findings are a reminder that behind every data point is a real person facing scary challenges in their cancer journey. The high symptom burden experienced by many patients before an acute care visit is a signal that there are missed opportunities along the way—chances to provide timely care and better manage symptoms before they force patients into an emergency situation.
Real Stories Behind the Data: Patient Experiences
Imagine a cancer patient who has been managing her illness for months, yet finds herself caught in a web of persistent pain, nausea, and fatigue. Despite regular visits to her oncologist, the subtle parts of her symptoms are either underreported or misunderstood. As her discomfort grows, she eventually reaches a point of no return, and unplanned acute care becomes her only option.
Now consider another patient from a minority background who faces language barriers and financial constraints. His subtle symptoms go unaddressed due to communication gaps and accessibility issues. When his symptoms escalate, he is forced to seek emergency care, a scenario that could have been prevented with proper early intervention.
These narratives, though simplified, illustrate the human cost behind the statistics. They remind us that addressing the earthbound challenges of symptom management goes far beyond the clinical environment—it requires a comprehensive strategy in healthcare policy, patient education, and community support.
Patient-Centered Approaches to Improve Symptom Management
To truly make a difference, healthcare systems must take a patient-centered approach. This means involving patients in their own care decisions, listening to their experiences, and tailoring interventions to meet their specific needs. Some key components include:
- Holistic assessments that consider both physical symptoms and emotional well-being
- Collaborative care models that include oncologists, primary care providers, and palliative care specialists
- Clear communication strategies to ensure patients understand their treatment plans and symptom management tactics
- Flexible scheduling and accessible follow-ups that are tailored to the patient’s daily routines and challenges
- Incorporating patient feedback into service design to continuously improve care delivery
Implementing these strategies is not a quick fix—it is a process that requires a sustained effort and a commitment to making incremental improvements. Nonetheless, the potential benefits in reducing unplanned acute care and improving patient quality of life are immense.
The Broader Healthcare Context: Managing Costs and Optimizing Care
Unplanned acute care visits are not only disruptive to patients—they also place significant financial burdens on healthcare systems. Managing these costs while ensuring quality treatment is one of the critical challenges facing modern medicine.
Tackling Healthcare Costs Through Early Symptom Intervention
When patients seek emergency care because their symptoms have escalated, the cost of treatment is invariably higher than if early interventions had been put in place. Research indicates that a proactive approach to symptom management in cancer care can potentially reduce the frequency of unplanned visits, easing the cost burden on both patients and healthcare providers. Here are some actionable considerations for cost reduction:
- Invest in early detection programs that monitor symptom evolution and trigger intervention before a crisis develops
- Expand telehealth services to provide immediate assistance and guidance on managing symptoms at home
- Implement patient education campaigns that empower individuals to recognize early warning signs and seek timely care
- Streamline resource allocation by using data-driven approaches, such as those provided by NLP, to identify high-risk groups
By paying attention to these key cost drivers, healthcare institutions can work on finding your path to an optimal balance between quality patient care and responsible resource management. This is not just about saving money—it is about making sure that every patient has the chance to receive the care they need when they need it most.
Integrating Community Resources and Support Networks
Another critical factor in reducing the financial and emotional strain of unplanned acute care is the integration of community resources. Many patients, particularly those from underserved communities, may benefit from community-based initiatives that offer support beyond the clinical setting. These might include:
- Local health clinics providing regular follow-up and symptom monitoring
- Support groups that offer peer counseling and practical advice on managing daily challenges
- Partnerships with non-profit organizations to bridge gaps in healthcare access
- Community outreach efforts that educate patients about preventive care and early intervention strategies
When combined, these community-based approaches can reduce the friction and intimidating aspects of accessing immediate healthcare support, providing a safety net for those who might otherwise fall through the cracks.
Future Directions: Research, Policy, and Practice
While the study we have examined provides vital insights into the symptom burden and documentation disparities in cancer care, it also prompts a number of questions and future directions for research, policy, and clinical practice.
Expanding Research Beyond Single-Center Studies
One of the major limitations of the current study is that it was conducted at a single tertiary-care institution, involving a predominantly White and insured population. Future research should aim to gather data from multiple sites and incorporate more diverse populations. This would help in understanding whether the observed trends are universal or if they vary across different healthcare settings and demographic groups.
Expanding the research scope could include:
- Multi-center studies to confirm the trends observed in smaller studies
- Inclusion of underrepresented demographics to capture a more comprehensive picture of symptom burden
- Longitudinal studies to track changes in symptom documentation over time
- Qualitative research to capture the perspectives of both patients and providers regarding symptom management and documentation challenges
Such studies would play a super important role in forming a stronger evidence base that could inform policy-making and clinical guidelines.
Policy Implications and the Need for Equitable Care
The data points to certain areas of the healthcare system that require urgent attention—namely, the disparities among various sociodemographic groups. Policy makers need to craft interventions that are not only effective but also equitable. Some policy recommendations might include:
- Mandating regular training for healthcare providers on the subtle details of unbiased symptom documentation
- Allocating more resources to community health centers serving minority and underinsured populations
- Incentivizing the development and adoption of technology, like advanced NLP systems, while ensuring these tools are calibrated for diverse patient populations
- Implementing quality metrics that specifically address disparities in symptom management and acute care visits
These measures, if implemented, could help ensure that early interventions and high-quality care are available to all patients, regardless of their background or socioeconomic status.
Integrating Multidisciplinary Approaches for a Holistic Solution
Modern healthcare is all about collaboration. Addressing the nerve-racking issues highlighted by the study requires the combined efforts of oncologists, primary care physicians, palliative care experts, and even data scientists proficient in NLP. Some recommendations for a multidisciplinary strategy include:
- Creating integrated care teams that meet regularly to discuss patient cases with a high symptom burden
- Sharing best practices on symptom management between different departments and specialties
- Implementing cross-training sessions where data analytics and clinical care intersect, ensuring that both sides understand the little twists and turns of each other’s work
- Developing standardized protocols that leverage both clinical judgment and data-driven insights
This collaborative approach is key to smoothing out the confusing bits and ensuring that patient care is both effective and equitable. By taking a well-rounded approach, healthcare providers can provide a more supportive environment that addresses both the physical and emotional needs of patients.
Conclusion: Steering Through the Twists and Turns of Acute Cancer Care
There is no doubt that the study we’ve discussed shines a light on critical areas in cancer care where early detection and symptom management can make a significant impact. The high prevalence of pain, nausea, and vomiting before unplanned acute care visits underscores the need for proactive strategies that address both the clinical and socio-economic challenges faced by patients.
The research not only highlights the potential of natural language processing to get into the fine points of clinical documentation but also reveals when and where the healthcare system is falling short—especially for women, racial minorities, and Medicaid-insured patients. With this knowledge in hand, clinicians, administrators, and policy makers must work together to find your way through the maze of barriers preventing equitable access to care.
As healthcare continues to evolve, it is imperative that we remain focused on developing targeted interventions and comprehensive approaches, ensuring that no patient’s journey through cancer treatment becomes an unnecessarily nerve-racking ordeal. By addressing the early signs of symptom escalation and rectifying documentation disparities, we can not only reduce healthcare costs but also enhance the overall quality of life for countless individuals living with cancer.
Ultimately, the real-world impact of such changes will be measured in fewer emergency visits, improved patient outcomes, and a healthcare system that truly serves all its communities. The insights from this study serve as a call to action—a reminder that every subtle detail and every little twist in the patient experience demands our attention. We must commit to a future where early intervention, equitable care, and supportive healthcare systems are not just ideals but everyday realities.
By working through these challenges together, we can transform the current state of cancer care into one where patients are empowered, disparities are minimized, and painful symptoms are addressed long before they necessitate acute intervention. This is not just a clinical challenge; it is a societal mission—a mission that requires our collective will, creative problem-solving, and a persistent drive to improve the lives of those affected by cancer.
In summary, the study prompts us to sort out the confusing bits of symptom documentation, to figure a path towards early intervention and equitable care, and to harness technology judiciously in our ongoing fight against cancer. As we take a closer look at these complex issues, we must be ready to tackle the tangled issues head-on, ensuring no patient feels left to face these overwhelming challenges alone.
It is through the combined efforts of research, clinical practice, and policy innovation that we can truly make a difference. And while the journey may be full of twists and turns, every step forward is a step toward a healthier, more equitable future for all cancer patients.
Originally Post From https://www.medscape.com/viewarticle/cancer-pain-most-common-symptom-before-acute-care-visits-2025a1000bae
Read more about this topic at
Cancer Disparities – NCI
The State of Cancer Disparities in the United States