Empowering Cancer Recovery: The Role of Specialized Physical Therapy
The journey through cancer treatment is filled with numerous twists and turns that affect not only the body but also the mind and spirit. As someone who has observed changes in modern cancer care, I believe that specialized physical therapy plays a super important role in helping patients regain strength, mobility, and, ultimately, their independence. In my view, physical therapy is a key pillar of cancer recovery that supports patients long after their primary treatments have ended, ensuring that they are not left to face the challenging physical aftermath on their own.
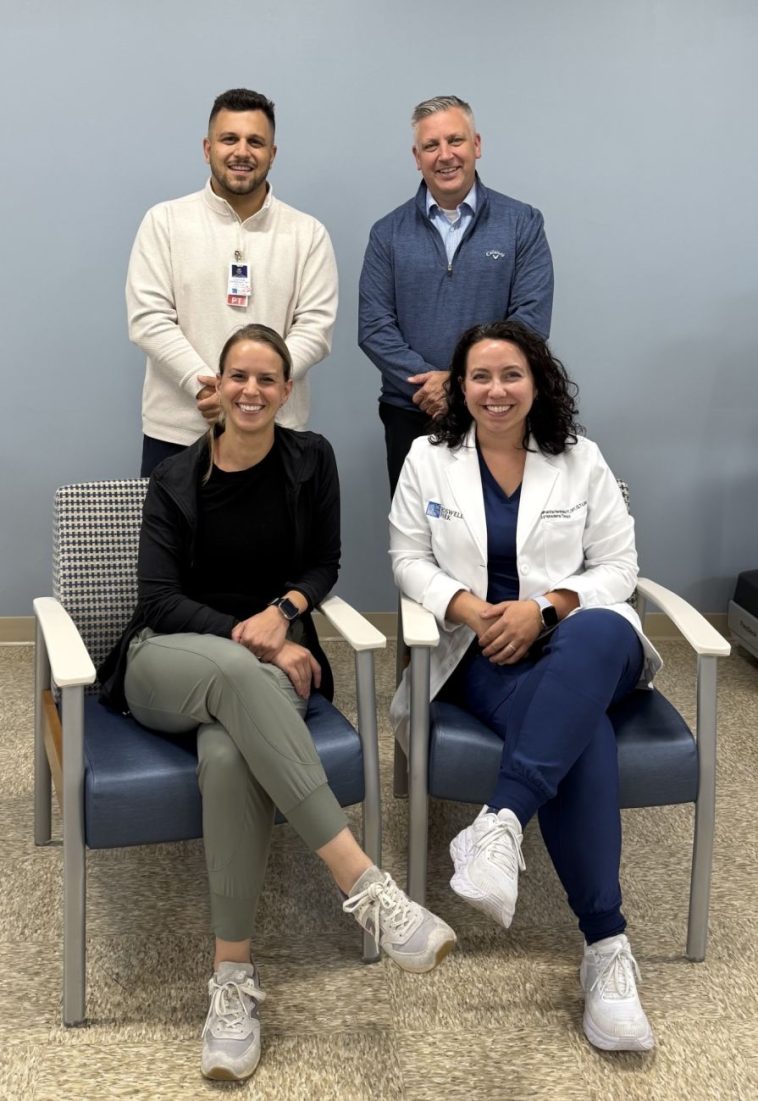
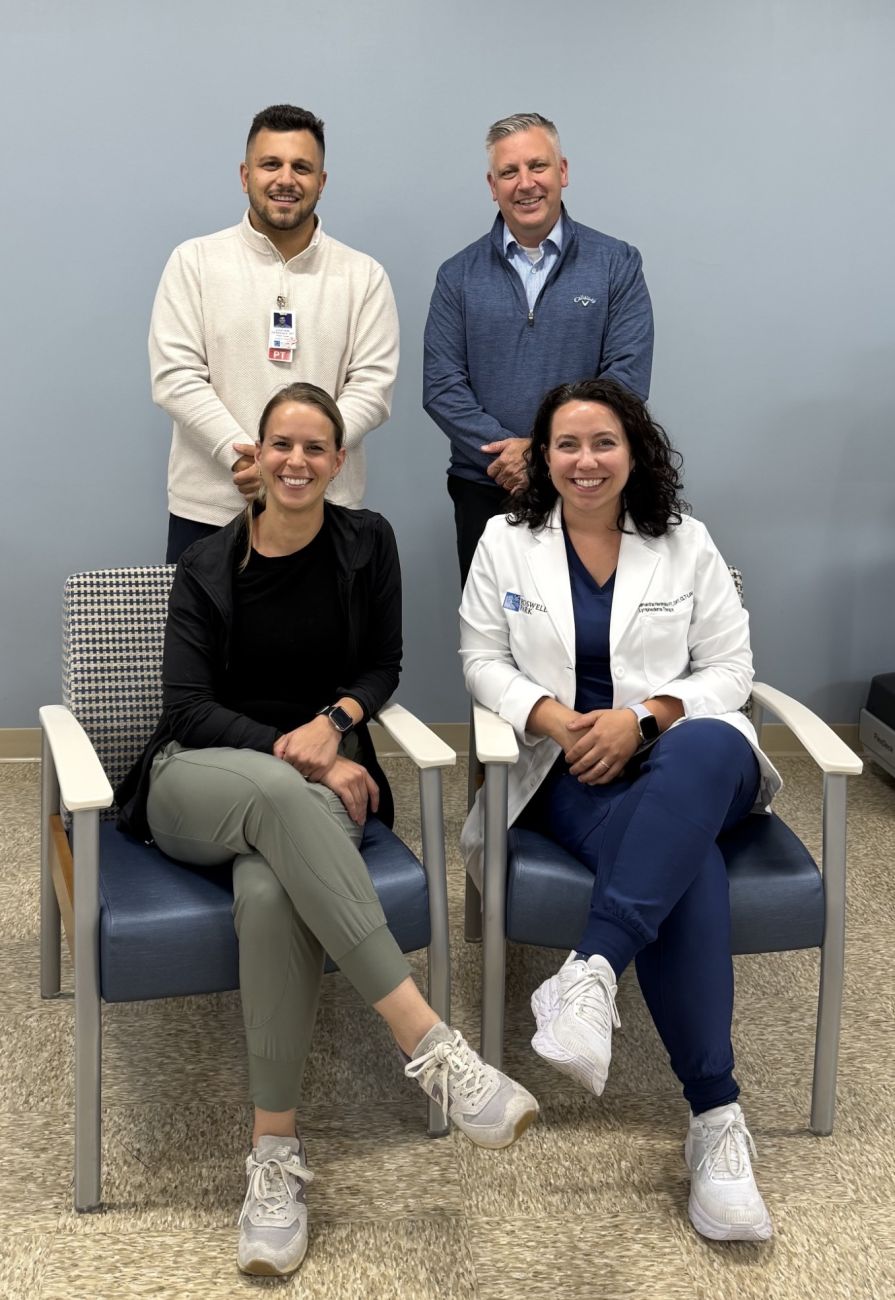
Modern cancer care now encompasses a broader approach that addresses both clinical needs and the everyday challenges patients face. At comprehensive centers like Roswell Park, physical therapy is tailored to meet the unique needs of each patient. This personalized approach in rehabilitation not only eases physical discomfort but also instills hope and motivation in patients facing a life-altering diagnosis.
Unique Challenges in Cancer Recovery: Tackling Tricky Parts in Rehabilitation
Cancer treatment often leaves patients dealing with a range of tricky parts in rehabilitation. The effects of surgery, chemotherapy, and radiation are far from uniform, and the recovery process can be nerve-racking for many. It’s essential for patients to understand that post-treatment fatigue, reduced mobility, and overall weakness are common hurdles—but not insurmountable ones.
Physical therapists at specialized cancer centers take a holistic view of these challenges. They work closely with oncologists and other care providers to chart a recovery plan aimed at overcoming the confusing bits that can impede daily activities. By focusing on boosting strength and mobility, these experts help patients find a path to a more independent life.
Here are some highlights of how physical therapy addresses these challenging parts:
- Personalized Exercise Regimens: Tailored routines that target individual areas of weakness.
- Strength and Endurance Training: Focusing on the tasks of daily living, from walking down a hallway to more strenuous activities like grocery shopping.
- Family and Caregiver Involvement: Ensuring that support networks are educated on safe techniques and methods to assist in daily recovery.
- Ongoing Education and Motivation: Physical therapists provide continual guidance and encouragement, which is essential for patients who feel overwhelmed by their new challenges.
Understanding the Subtle Details of Physical Therapy Techniques
Delving into the subtle details of physical therapy, one finds that the approach at centers like Roswell Park doesn’t simply aim to produce measurable improvements in mobility. Instead, physical therapists focus on the little details that make a huge difference in patient recovery. This means understanding both the finely honed exercise techniques and the recovery timeline that best suits each individual’s condition.
Specialist therapists are skilled at considering various test results—such as hemoglobin and platelet counts—that indicate whether a patient is ready to tackle more intensive physical routines. They factor in any existing fractures, sensitivities, or risk of falling when recommending exercise programs. This meticulous attention to the nitty-gritty ensures that patients are not pushed beyond their capacity and that safety remains a priority throughout the rehabilitation process.
With an emphasis on the subtle parts, the physical therapy program extends beyond simple exercise. Patients learn how different movements and exercises can help manage side effects and restore function over time. By working hand-in-hand with their doctors, therapists make sure that every exercise is suited to the patient’s overall treatment progress, ensuring that each small step is a move toward greater strength.
Managing Mobility: Overcoming Intimidating Side Effects of Cancer Treatments
One of the most frustrating aspects of cancer treatment is the mobility issues that many patients experience. Physical challenges can seem overwhelming after enduring the taxing effects of chemotherapy, radiation, or surgery. Many patients find that moving around their homes, once a simple task, now requires significantly more effort. This is where the expertise of a dedicated physical therapist becomes indispensable.
Physical therapists help patients tackle these overwhelming challenges by focusing on building endurance and reinforcing safe, manageable movement. The role of these specialists is not just to improve muscle strength but also to educate patients about pacing and self-care. They teach patients how to conserve energy for the tasks that matter most, thereby reducing overall fatigue and preventing further injury.
The following table outlines the differences between inpatient and outpatient physical therapy programs in the context of cancer recovery:
| Inpatient Therapy | Outpatient Therapy | |
|---|---|---|
| Setting | Hospital-based, immediate post-surgery care | Standalone clinics, community-based support |
| Focus | Regaining basic mobility and strength | Advanced mobility techniques and long-term care |
| Frequency | Multiple sessions daily during the hospital stay | Regular weekly or bi-weekly sessions |
| Support | Immediate medical oversight and integrated care | Community and family support after discharge |
Holistic Approaches: Integrative Therapies and Their Key Outcomes
Aside from standard physical therapy exercises, a holistic approach to cancer recovery brings in other integrated therapies that target both the body and mind. Holistic care is critical because it acknowledges that recovery is not solely about physical improvement but also about emotional and mental wellness.
Integrative therapies such as lymphedema management, pelvic floor rehabilitation, and pulmonary rehabilitation are essential components of the holistic recovery model. These therapies work to repair the physical damages inflicted by treatment and help patients regain confidence in their bodies. By incorporating methods that address the whole person rather than isolated physical issues, therapists empower patients to overcome the tangled issues that may stand between them and independent living.
Some of the key outcomes of holistic, integrative physical therapy include:
- Improved Physical Function: Enhanced strength and mobility that support everyday activities.
- Emotional Resilience: A boost in confidence and reduction in treatment-related anxiety.
- Enhanced Quality of Life: A better outlook on recovery thanks to comprehensive care.
- Preventative Health Measures: Strategies to maintain mobility and manage long-term side effects.
Addressing Lymphedema: Sorting Out the Swollen Challenges
Lymphedema is one of the more daunting side effects that can occur after cancer treatment, particularly following surgery or radiation therapy. This condition, which leads to swelling in the arms, legs, or trunk due to a buildup of lymphatic fluid, is often full of problems that can hinder a patient’s recovery. The goal in treating lymphedema is to manage swelling effectively to reduce discomfort and prevent complications such as infection.
Specialized physical therapists are adept at sorting out these swollen challenges. Techniques used include manual lymphatic drainage, compression therapy, and exercise routines tailored to enhance lymphatic flow. Patients also receive education about self-care practices that can be followed at home, making it easier to manage symptoms before they escalate.
Here is a summary of standard treatments for lymphedema:
- Manual Lymphatic Drainage (MLD): A gentle massage technique that encourages lymph flow.
- Compression Therapy: Use of bandages or garments to reduce fluid buildup.
- Targeted Exercises: Movements designed to stimulate the lymphatic system.
- Skin Care Regimens: Preventative measures to reduce the risk of infection.
These methods, when applied promptly and consistently, can help patients feel more comfortable in their bodies and ensure that they maintain a higher level of independence as they recover.
Pelvic Health in Cancer Survivorship: Getting Around Confusing Bits of Post-Treatment Recovery
Another area where physical therapy makes a super important difference is in pelvic health care. Many cancer patients, especially survivors of cancers that affect the pelvic region, experience complications such as urinary and bowel incontinence, pelvic pain, or even sexual dysfunction. These confusing bits of post-treatment recovery can be especially overwhelming, significantly impacting the overall quality of life.
Physical therapists who specialize in pelvic health work closely with patients to help them regain control. Through a combination of manual therapy, targeted exercises, and self-care education, therapists equip patients with the tools they need to manage symptoms effectively. The main aim is to restore comfort and confidence in everyday bodily functions, which often suffer in the wake of aggressive cancer treatments.
Key components of pelvic floor rehabilitation include:
- Manual Muscle Release: Techniques to ease tight muscle regions and relieve pain.
- Education on Normal Function: Informing patients about typical patterns of urinary and bowel activity.
- Therapeutic Exercises: Exercises that increase strength, flexibility, and coordination.
- Self-Management Strategies: Empowering patients to handle their own care with confidence.
Patient-Centered Recovery: Customizing Physiotherapy Programs for Unique Needs
In my experience, one of the most compelling aspects of cancer rehabilitation is the personalization of physical therapy programs. Every patient comes with a set of unique needs influenced by their diagnosis, treatment journey, and personal health background. This requires therapists to really dig into creating recovery plans that are as individualized as possible.
One size does not fit all when it comes to cancer recovery. Depending on whether a patient is newly diagnosed, in the process of treatment, or working to maintain mobility post-treatment, the goals and strategies can differ dramatically. For example, while some patients might need a single session to learn a new technique, others might benefit from multiple appointments per week over several months to build strength progressively.
A tailored recovery plan often includes:
- Initial Assessment: A thorough evaluation of the patient’s current physical state, including medical history, strength levels, and mobility challenges.
- Goal Setting: Establishing realistic, incremental objectives that help guide therapy sessions.
- Customized Exercise Programs: Routines designed to address specific issues such as weakness in the lower limbs or reduced upper body mobility.
- Regular Reassessments: Continuous evaluation of progress and adjustment of exercises to match evolving needs.
This personalized approach ensures that every patient receives the level of care they truly need, making the journey to recovery less intimidating and more manageable over time.
Support, Empathy, and Education: The Nitty-Gritty of Physical Therapy
Physical therapy at a cancer center is about more than just the exercises—it’s a holistic approach that combines support, empathy, and detailed education. Patients often face scary and nerve-racking uncertainties during their recovery, and therapists step in not only as exercise instructors, but also as guides through the maze of post-treatment life.
Therapists emphasize the value of education, showing patients what to expect and how to cope with the changes in their physical capabilities. For instance, when a patient undergoes a procedure like a mastectomy, there can be legitimate concerns about whether simple daily movements will remain possible. Therapists work through these fears by teaching safe and effective movements, ensuring that patients learn to manage their own rehabilitation journey.
Key takeaways from a supportive physical therapy approach include:
- Clear Communication: Discussing expected challenges and outlining achievable goals.
- Compassionate Care: Offering reassurance and empathy to help patients cope with anxiety about their physical state.
- Proactive Education: Informing patients about potential side effects and recovery milestones, reducing the sense of being off-course.
- Integrated Family Involvement: Engaging family members in the recovery process to provide additional layers of support.
This bond between therapist and patient is often the unsung hero in rehabilitation. It builds trust, creates a sense of partnership in recovery, and embodies the understanding that every little progress marks a significant victory on the long journey to independence.
Addressing the Overwhelming Effects: A Closer Look at Side-By-Side Comparisons
Cancer therapies, such as chemotherapy and radiation, present a myriad of side effects that create a tangled mix of physical and emotional challenges. When patients are discharged, they often feel overwhelmed by the physical changes—ranging from muscle atrophy to balance issues—that they did not anticipate. Combining the efforts of physical therapy with broader support services helps create a comprehensive recovery framework.
Outlined below is a summary of common side effects from cancer treatment and how physical therapy can help mitigate them:
| Side Effect | Impact | Physical Therapy Strategy |
|---|---|---|
| Muscle Weakness | Decreased ability to perform daily tasks | Strength training and tailored exercise routines |
| Fatigue | Low energy affecting mobility and mood | Energy conservation techniques and gradual activity pacing |
| Balance Issues | Risk of falls and injuries | Stability and coordination exercises |
| Pain and Stiffness | Difficulty in movement and discomfort | Manual therapy and flexibility exercises |
By carefully addressing these challenges, physical therapy not only aids in the recovery process but also contributes significantly to the overall well-being of cancer survivors. It’s a deeply collaborative process that requires the patient to remain engaged, while the therapist patiently works through each confusing bit and each small twist that may arise.
Looking Ahead: Building a Pathway to Independence after Cancer
The ultimate goal of any rehabilitation program, and especially in the context of cancer, is to rebuild independence. The process of getting back on one’s feet is often gradual, and both patients and therapists need to acknowledge that recovery is filled with both setbacks and breakthroughs. It’s about learning to find your way through a maze of physical limitations and emotional challenges.
For many patients, the return to independent living doesn’t just mean moving freely around the house—it also represents reclaiming a sense of normalcy, reconnecting with hobbies, and reengaging with the community. As physical therapy helps to strengthen muscle groups and improve mobility, it also opens doors to activities that may have once seemed unreachable. In this way, therapists play a crucial role in not just physical healing, but in restoring a patient’s will to live fully.
In practical terms, the pathway to independence can be outlined in several stages:
- Initial Recovery: Building functional strength and overcoming immediate post-treatment weakness.
- Progress Monitoring: Regular assessments to tailor ongoing therapy to evolving needs.
- Enhanced Mobility Training: Introducing more advanced movement routines as strength improves.
- Community Reintegration: Assistance with adapting to daily living outside the hospital setting.
This step-by-step recovery can be seen as a blueprint for long-term success. Even if some parts of the process feel off-putting or even scary at the outset, the dedication of both the patient and their care team makes all the difference. Every small improvement is a sign that progress is being made, no matter how gradual it might seem.
Conclusion: Finding Hope in the Journey of Cancer Rehabilitation
After exploring the many facets of cancer rehabilitation, it’s clear that specialized physical therapy is not just a side note in cancer care—it is a cornerstone of recovery. By addressing everything from the tricky parts of regaining mobility to the tangled issues associated with lymphedema and pelvic health, expert therapists lay a strong foundation for a return to independent living.
From patient-centered recovery programs to integrated holistic care, the detailed approach taken by professionals in this field demonstrates that every bit of effort counts. The collaboration between therapists, doctors, patients, and caregivers is essential in transforming a potentially overwhelming situation into a manageable process. As patients learn to steer through their recovery journey, they garner not just physical strength but also hope and confidence in a brighter future.
It is through their detailed and empathetic care that patients not only heal but also rediscover their ability to lead fulfilling lives after cancer. The integration of modern medicine with rehabilitative and alternative care strategies shows that, even in the face of serious illness, there is an abundance of support and expertise available. With every step forward—no matter how small—cancer survivors move towards a life that is empowered by recovery, enriched by community, and emboldened by the determination to overcome the challenges that lie ahead.
For anyone facing the nerve-racking aftermath of cancer treatment, the message is clear: you are not alone. Dedicated physical therapy services, supported by a compassionate team of experts, are designed to guide you through every twist and turn, ensuring that, step by step, you regain the strength and confidence needed to lead a full, independent life. The journey may be long and sometimes intimidating, but with targeted care and a personalized recovery plan, every patient has the potential to emerge stronger and ready to embrace the future with renewed hope.
Originally Post From https://www.roswellpark.org/cancertalk/202510/meet-team-physical-therapy
Read more about this topic at
Empowering Cancer Survivors in Managing Their Own Health
Find Support Programs and Services in Your Area