The Digital Revolution in Oncology: A New Era of Personalized Cancer Care
In today’s fast-evolving world of medicine, groundbreaking developments are steadily reshaping the way we approach cancer care. Recent breakthroughs at renowned institutions, such as MD Anderson, illustrate a drive toward personalized treatment plans, innovative use of digital twin models, and streamlined patient interactions. As we witness a transition from conventional approaches to intelligent, data-driven methods, many are beginning to get into how these novel techniques not only promise improved outcomes but also make the patient journey less intimidating.
The rising integration of advanced computational modeling alongside traditional laboratory experiments is not just a technological triumph—it’s a testament to the relentless efforts of experts determined to conquer some of the most tangled issues in oncology. In this editorial, we will take a closer look at the promising role of digital twin models in oncology, explore various aspects of patient care, and consider the exciting future of collaborative research and clinical trials.
Digital Twin Models in Modern Cancer Research
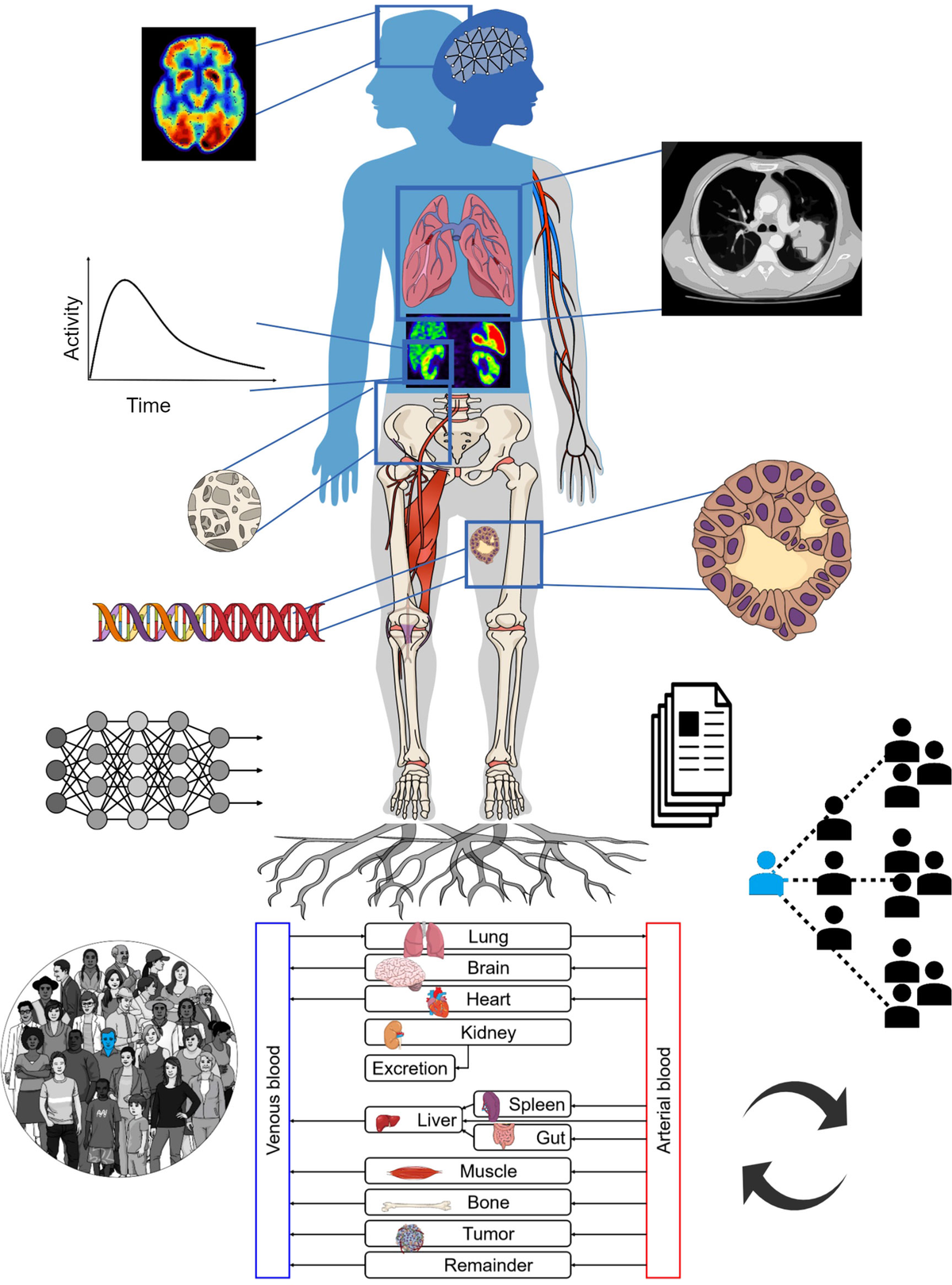
The concept of digital twin models is slowly revolutionizing how we predict, manage, and treat cancers like prostate and renal. These models rely on integrating experimental data with sophisticated computational tools, aiming to mimic the real-world behavior of tumors. Many experts are excited about the potential here because models such as A(BM)² simulate everything from the formation of blood vessels to bone resorption, mapping out even the smallest twists and turns of tumor progression.
Personalized Treatment Approaches for Bone Metastasis
Bone metastasis remains one of the most challenging aspects of treating advanced cancers. In patients with prostate and renal cancers, for example, metastatic bone disease is a key factor that often contributes to poor outcomes. The new digital twin models are enabling oncologists to “figure a path” through this tangled issue by forecasting how a tumor might respond to treatments like cabozantinib and zoledronic acid.
By capturing the fine points of tumor location, blood vessel formation, and bone resorption processes, these digital innovations offer a way to customize drug regimens more effectively. As the models closely mimic in vivo data, they give researchers a clear picture of how tumors behave under various conditions. This, in turn, could pave the way for more personalized cancer therapies tailored to each patient’s unique circumstances.
Key Benefits of Integrated Computational Modeling
- Enhanced Predictability: Digital twin models support oncologists in predicting treatment outcomes more precisely.
- Reduced Uncertainty: By incorporating rich data sets, these models reduce the confusing bits and tangled issues that have long made cancer treatment unpredictable.
- Personalized Regimens: Tailoring treatments to individual patients becomes more practical when the models provide detailed forecasts of tumor behavior.
- Feedback Loop Benefits: A powerful feedback loop is created when experimental data is integrated with digital modeling, ensuring ongoing improvement in treatment strategies.
This approach is a super important development reflecting a trend toward making experimental data more usable for clinical decisions and heralds a future where treatment plans are exclusively data-driven and uniquely tailored for each patient.
The Patient Journey: From Digital Portals to Clinical Trials
Modern healthcare is increasingly centered on patient engagement, with online portals allowing patients to schedule appointments, track their care, and explore various options for screening and treatment options. Websites that were once complex and off-putting in their layout now showcase intuitive design and clear pathways for patient self-management.
Empowering Patients with Digital Access
One of the key shifts in today’s healthcare landscape is the transformation of patient communication channels. Personalized portals empower patients to make appointments, ask questions, and track their care information—the digital equivalent of finding your way through busy hospital corridors.
These platforms are designed to provide essential information without overwhelming users with nerve-racking or intimidating details. Whether you’re a new patient or a returning one, these digital tools are built to simplify the process, ensuring that finding your path to care is as smooth as possible.
The Role of Online Appointment Systems
Scheduling appointments on digital platforms not only saves time—it also connects patients with tailored resources like clinical trials, genetic testing, and reimbursed care options. Healthcare institutions like MD Anderson have refined this process through secure, personalized websites that allow patients to book appointments, review billing information, or even check on the latest research news.
Here’s what makes an effective patient portal:
| Feature | Benefit |
|---|---|
| Secure Login | Protects patient data and ensures privacy |
| Appointment Scheduling | Simplifies the process of booking and managing visits |
| Real-Time Updates | Keeps patients informed about their care schedules and new research |
| Integrated Resources | Provides access to clinical trial information, billing, and educational material |
The smart design of these platforms helps patients manage their health journeys better, ensuring that crucial details are always within reach and explained in clear, accessible language.
Clinical Trials and Innovative Research: A Collaborative Effort
The clinical trial landscape is rapidly evolving as research institutions, healthcare providers, and patients work together toward a common goal—ending cancer. Clinical trials are now a cornerstone of modern oncology treatment, enabling the testing of novel therapies that can be fine-tuned and then distributed across broader patient populations.
The Role of Collaborative Clinical Research
Clinical trials historically have been seen as a way to access experimental treatments, but they are much more than that. They offer a dynamic environment where the fine shades of treatment responses, subtle parts of tumor behavior, and small distinctions in patient responses are closely studied. Such trials are powered by collaborative efforts, where diverse teams from multiple disciplines pool their expertise.
Some significant benefits of robust clinical trials include:
- Access to New Treatments: Patients can benefit early from therapies that could potentially save lives.
- Rigorous Data Collection: The detailed data collected helps refine treatment protocols and predictions made by digital twin models.
- Enhanced Safety Monitoring: Continuous monitoring ensures that any adverse effects are identified early, protecting patients from risky interventions.
- Strategic Resource Allocation: Research funding and collaborations ensure that important projects receive the support they need.
Clinical trials are not without their challenges. The process can be intimidating at times, laden with regulatory and ethical considerations. However, the combined efforts of clinicians, patients, and research centers help steer through these issues, ensuring that the development of new therapeutics is both scientifically rigorous and patient-centric.
Integrating Experimental Data with Computational Modeling
The integration of experimental observations with computational modeling, as showcased by digital twin initiatives, brings a refreshing perspective to cancer research. This blend of hard data and advanced algorithms allows for predictive insights that are both imaginative and rooted in scientific evidence.
Consider the following steps that typically define this process:
- Data Collection: Detailed experimental data is gathered from clinical studies, laboratory experiments, and imaging techniques.
- Model Development: Computational models are developed using this data to simulate complex tumor behavior.
- Predictive Analysis: These models then simulate treatment responses, helping researchers understand how slight differences in intervention could affect patient outcomes.
- Feedback Loop: Ongoing research refines these models continuously, ensuring that predictions remain as accurate as possible.
This process, while sometimes complicated by the need to accommodate a myriad of variables, illustrates just how key modern data integration has become in the realm of oncology. With every step, the collaboration between tech innovators and clinicians is proving to be a super important part of making cancer treatment more reliable and personalized.
Patient-Centered Care in the Digital Age
In an era where healthcare is increasingly digital, the evolution of patient-centered care is evident from the seamless online resources available at major health centers. This new privacy-focused system has revolutionized how patients interact with the healthcare system, allowing them to schedule appointments, follow up on their treatment, and even connect with research initiatives via dedicated digital spaces.
Enhancing Communication Through Secure Portals
The transformation in patient communication has been marked by a move away from those confusing bits of bureaucracy. Secure digital portals have been developed to ensure that information is delivered clearly and concisely. For instance, patients can now easily access:
- Medical Records: Quickly reviewing treatment histories and lab results
- Appointment Management: Booking or rescheduling visits with a few clicks
- Clinical Resources: Accessing educational material and clinical trial information
- Support Services: Finding resources for managing the emotional and physical effects of cancer treatment
All these resources are designed with the patient in mind—clearly presented, easy to use, and intended to help patients find their way in what can sometimes feel like a maze of clinical details. This evolution is not just about technology; it’s about reinforcing the relationship between medical providers and their patients, ensuring that everyone feels heard and well-informed.
Ensuring Transparency in Patient Experiences
Transparency is another critical element in modern healthcare platforms, allowing patients and their families to manage their care without feeling overwhelmed by nerve-racking uncertainty. Clear communication regarding diagnosis, treatment options, and likely side effects can often make the difference in relieving anxiety among patients facing intense treatment pathways.
Some strategies to improve transparency include:
- Regular Updates: Keeping patients informed of their progress and next steps.
- Accessible Data: Sharing clinical trial results and research updates in layman’s terms.
- User-Friendly Interfaces: Simplified design helps patients avoid the tricky parts of deciphering medical jargon.
- Feedback Opportunities: Allowing patients to express their concerns and experiences, thereby contributing to continuous improvement of service delivery.
These initiatives make the approach to healthcare a shared journey. When patients feel empowered to ask questions and receive timely answers, the relationship with their care team is strengthened—a relationship that is crucial when embarking on a treatment journey that might initially seem off-putting or overwhelming.
Collaboration in Healthcare: Bridging Research and Clinical Implementation
The successful merger of experimental research with computational advancements is only possible through significant collaborative efforts in the healthcare and scientific community. Institutions like MD Anderson work in tandem with research centers, mathematicians, and clinical experts to ensure that the latest innovations are thoroughly vetted and ready for real-world application.
The Power of Interdisciplinary Collaboration
One of the standout aspects of recent cancer research initiatives is the active involvement of professionals from a variety of disciplines. From mathematicians who develop the intricate models to oncologists who interpret the data, every player has a critical role in moving the needle on cancer treatment.
Key aspects of interdisciplinary collaboration include:
- Diverse Expertise: When experts in surgery, oncology, and computational modeling pool their knowledge, they can address even the most complicated pieces of cancer biology.
- Shared Resources: Collaborative projects often come with robust funding and shared infrastructural support from institutions like the National Cancer Institute and state research agencies.
- Unified Goals: The collective aim is to design treatment strategies that are personalized, efficient, and scalable, all while ensuring patient safety.
This collaborative spirit has fostered a culture of innovation that is a must-have in today’s challenging medical environment. The merging of insights from multiple fields is leading to breakthroughs that not only improve overall research but also enhance everyday patient care.
Lessons Learned from Recent Clinical Successes
Recent studies have underscored the potential of digital twin models to predict treatment responses with impressive accuracy. One such study, published in a leading oncology journal, highlights that integrating digital models with tangible experimental data can assist researchers in mapping out the microenvironment of tumors. These advancements prove particularly useful when exploring clinically relevant scenarios such as the impact of drug dosing and withdrawal in the context of metastatic disease.
Key lessons from these successes include:
- Data-Driven Decision Making: Enhanced models facilitate better treatment planning by providing a more reliable forecast of patient outcomes.
- Customized Therapy Development: Tailoring therapeutic interventions based on predictive data helps in mitigating possible side effects while maximizing benefits.
- Real-Time Adjustments: Continuous monitoring and feedback allow for dynamic adaptations to treatment strategies, ensuring safety and effectiveness.
These improved outcomes serve as a beacon of hope, reaffirming the immense potential that a union of clinical acumen and computational insight holds for the future of cancer treatment.
Funding, Donations, and Support: The Backbone of Ongoing Research
The journey from laboratory discovery to clinical application is powered not just by scientific genius, but also by strong financial support from donors, foundations, and government agencies. Funding is essential for fueling the research that forms the backbone of innovations like digital twin models and transformative clinical trials.
The Impact of Community and Corporate Support
It is important to recognize the contributions of those who support cancer research financially. Without generous donations and corporate alliances, many of the exciting advancements in cancer care would remain in the realm of theory. Whether it’s through targeted endowments, matching gifts, or charitable events, community support plays a super important role in driving research forward.
Some ways in which financial support bolsters cancer research include:
- Funding Clinical Trials: Financial resources enable rigorous trials that test new treatment modalities, offering hope to patients worldwide.
- Supporting Interdisciplinary Teams: Adequate funding allows for the assembly of teams that blend diverse expertise for comprehensive research projects.
- Accelerating Innovation: Research grants and endowments help to fast-track the development of promising digital tools and models.
- Enhancing Patient Care: Donations directly contribute to innovative patient care initiatives, ensuring that the latest breakthroughs reach the bedside faster.
The funding climate for medical research, while occasionally loaded with issues and regulatory challenges, continues to be buoyed by a shared commitment from patients, philanthropists, scientists, and community stakeholders. In a realm filled with both exciting possibilities and nerve-racking uncertainties, every contribution plays a role in making cancer care a community effort.
The Future of Cancer Care: A Synthesis of Technology, Research, and Compassion
Looking to the future, it is clear that the convergence of digital technology, clinical research, and patient-centric approaches is rewriting the playbook for cancer care. Digital twin models, innovative clinical trials, and integrated data systems are not merely futuristic concepts—they are here now, paving the way for treatments that are both precise and compassionate.
Anticipating Further Advances in Digital Patient Platforms
As patient portals continue to evolve, we can expect even tighter integration of real-time data and research breakthroughs into the patient experience. These platforms do more than just manage appointments and share medical records—they have the potential to integrate personalized treatment planning tools, predictive analytics for treatment response, and educational resources that are tailored to individual patient profiles.
Future digital patient platforms may offer features such as:
- Enhanced Predictive Diagnostics: Leveraging digital twin models to forecast patient outcomes with greater precision.
- Interactive Education Modules: Empowering patients with easily accessible information on their conditions and potential treatments.
- Virtual Care Coordination: Seamless communication channels that connect patients with their care teams in real time.
- Personalized Health Dashboards: Customized interfaces that track treatment progress, lab results, and upcoming appointments.
These innovations, while still in early development, promise to transform how patients and providers work through the many subtle details of cancer care, ensuring that each step is manageable, informed, and supportive.
Bridging the Gap Between Research and Everyday Care
One of the most promising aspects of today’s healthcare innovations is the growing gap between research laboratories and clinical practice. With digital twin models serving as a bridge, the subtle parts of experimental data are being translated into actionable insights. These insights allow clinicians to make informed decisions based not just on theoretical knowledge, but on practical, time-tested simulation data.
This bridging of research and clinical application is made possible by:
- Cross-Disciplinary Partnerships: Collaborative work between computational scientists, biologists, and clinicians ensuring that research insights are effectively implemented.
- Robust Data Sharing Protocols: Secure and efficient sharing of patient data that preserves privacy while enhancing collaborative research efforts.
- Policy Support: Ongoing efforts by regulatory bodies to streamline clinical trial processes and data integration protocols.
These collaborations allow the research community to get around some of the confusing bits and off-putting challenges typically associated with adopting new technologies in healthcare. When every stakeholder—from the lab bench to the patient bed—is on board, the overall trajectory of care improves significantly.
Embracing a New Paradigm in Healthcare Communication and Research
The entire healthcare ecosystem is poised for a significant makeover. Legacy systems are giving way to advanced, user-friendly platforms that enrich both patient experiences and research outcomes. Digital tools are proving their mettle in clinical settings, and the growing data pool continually informs better, more personalized treatment protocols.
Streamlined Communication Channels in Healthcare
For many healthcare providers, clear and efficient communication is the key to delivering effective care. The development of secure, accessible patient portals is a prime example of how the field is working through some of the more challenging parts of patient communication. By simplifying the process of accessing test results, scheduling appointments, and receiving updates, providers can reduce the overwhelming aspects of medical care—making each patient feel more confident and supported throughout their journey.
Effective communication systems contribute by:
- Reducing administrative delays.
- Smoothing out scheduling conflicts.
- Providing clear, jargon-free explanations of complex treatment protocols.
- Facilitating rapid response in times of patient need.
This is crucial not only for day-to-day patient care but also for empowering patients to take a more active role in managing their conditions—a shift that is steadily reshaping the landscape of modern medicine.
Sharing Research Breakthroughs with the Public
Transparency in communicating research findings plays a super important role in public health. Whether it’s the announcement of a new digital twin model or updates on clinical trials, sharing these breakthroughs helps build trust with the broader community. Public relations offices and patient outreach initiatives work together to simplify even the most tangled topics in cancer research, ensuring that state-of-the-art medical advancements are conveyed in a clear and relatable manner.
Efforts to communicate research effectively might include:
- Press Releases: Summarizing key findings while avoiding overly technical language.
- Community Seminars: Educating the public about recent developments and their real-world implications.
- Interactive Webinars: Allowing audiences to ask questions and gain insights directly from leading researchers.
These communication channels are essential in demystifying the fine points of research and ensuring that public support for ongoing innovation remains robust.
Charting the Path Forward: A Call for Continued Innovation and Collaboration
The intersection of technology, research, and compassionate care represents a powerful momentum shift in modern oncology. Digital twin models, refined clinical trials, and enhanced patient portals are now working in unison to turn previously intimidating challenges into opportunities for improved outcomes and better quality of life for cancer patients.
Encouraging More Collaborative Endeavors
As we look ahead, it is clear that the future of cancer treatment relies on robust collaboration between researchers, clinicians, and patients. Continued investment in interdisciplinary projects that bridge experimental models with clinical practice will further refine treatment paradigms and make the fine details of cancer care even more manageable.
Key areas for continued focus include:
- Investing in Data Integration: Prioritizing the development of platforms that merge clinical data with computational models.
- Enhancing Patient Outreach: Ensuring that patients are educated and engaged, with access to tools that demystify their different treatment options.
- Fostering Public-Private Partnerships: Encouraging collaboration between academic institutions, healthcare providers, and industry leaders to drive innovation home.
- Expanding Clinical Trial Networks: Broadening the scope and accessibility of clinical trials to include diverse patient populations.
By embracing these strategies, the healthcare community can continue to achieve breakthroughs that not only improve survival rates but also enhance the quality of life for each patient undergoing treatment.
A Vision for Tomorrow’s Cancer Care
The advancements in digital twin technology, along with a renewed commitment to patient-centered digital interfaces, lay the groundwork for a future where cancer care is more responsive, personalized, and effective. This new paradigm is the result of decades of incremental progress, persistent research, and a willingness to face even the most intimidating challenges head-on.
One can only be optimistic about the prospects when data-driven insights allow oncologists to provide precision medicine that is tailor-made for each patient. With continued support from research funding, community engagement, and interdisciplinary collaboration, the fight against cancer is charting a promising path—one where technology and compassion walk hand in hand.
Final Thoughts: A Call for Unity in the Battle Against Cancer
In summary, the transformation seen in patient care, computational modeling, and research at institutions like MD Anderson is nothing short of revolutionary. As we take a closer look at the innovative ways digital twin models are already impacting treatment for bone metastasis, it becomes apparent that we are on the verge of a new era in oncology—a future where every step is informed by data, every twist and turn is understood, and every patient receives treatment that is as unique as their genetic makeup.
These developments encourage us all to get into the conversation about the future of medicine—a conversation that demands continued investment, collaboration, and a collective commitment to innovation. It is a reminder that despite the sometimes intimidating road ahead, the combined efforts of technology, research, and compassionate care can overcome even the nerve-racking challenges posed by cancer.
For healthcare professionals, patients, and supporters alike, the message is clear: together, we can navigate this complex landscape, working through the confusing bits and twisted turns to create a system that not only treats cancer but also uplifts every aspect of the patient experience. The road ahead may be laden with challenges, yet every collaboration, every donation, and every innovative trial brings us closer to a day when cancer is a conquerable foe.
Let us embrace a future where the integration of computational modeling with clinical practice is not merely an experimental exercise, but a standard of care—a future where personalized medicine is the norm, and every patient can find their way to a healthier, brighter tomorrow.
Originally Post From https://www.mdanderson.org/newsroom/research-highlights/digital-twin-model-shows-promise-for-predicting-bone-metastasis-treatment-response-in-prostate-and-renal-cancers.h00-159779601.html
Read more about this topic at
CanSeer: a translational methodology for developing …
CMU Researchers Build Personalized Models To Advance …