EGFR-Mutant Lung Cancer: Emerging Treatments in a Changing Landscape
The current approach to designing cancer therapies, especially for EGFR-mutant lung cancer, is undergoing a significant transformation. In recent years, groundbreaking treatment options and novel combination regimens have emerged, aiming to make the journey less overwhelming for patients. This opinion editorial takes a closer look at these advances, discussing the benefits and some of the tricky parts of the new therapeutic landscape while considering the impact on quality of life.
Understanding EGFR-Mutant Lung Cancer and Its Treatment Challenges
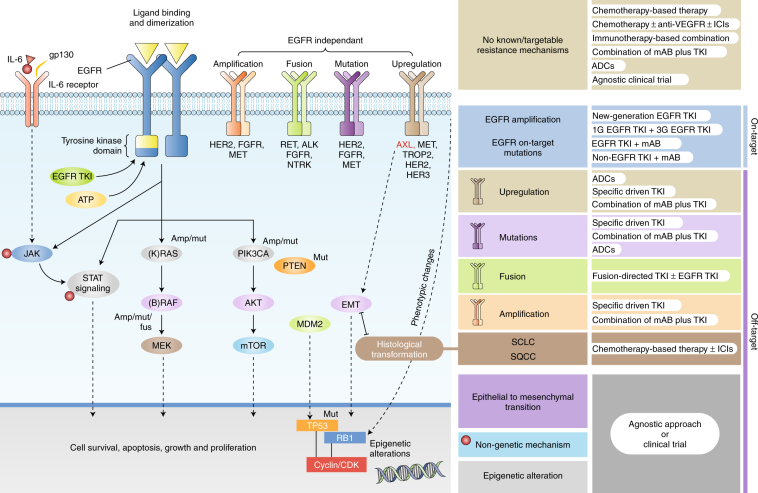
EGFR-mutant lung cancer has posed several tangled issues to oncologists. The condition typically involves the malfunctioning of the epidermal growth factor receptor (EGFR) and requires treatments that can adapt to not only the disease’s evolution but also to the individual patient’s tolerance. With numerous options available, the field has become loaded with both hope and nerve-racking decisions. Managing your way through the treatment maze requires clarity on every subtle part and a deep dive into how combination therapies are addressing these competing needs.
Key Role of Tyrosine Kinase Inhibitors (TKIs) in EGFR-Mutant Lung Cancer
For years, TKIs have been the cornerstone of treatment for patients with EGFR-mutant lung cancer. Medications like Tagrisso (osimertinib) have become common household names among oncologists, largely because of their ability to target the fine points of the mutation at a molecular level. These pills have offered a more tailored approach, bypassing some of the intimidating side effects associated with broader chemotherapy agents.
However, even with the success of these targeted agents, there remain many subtle details and complicated pieces that require close attention. The treatment regimen for each patient is layered with small distinctions based on the stage of the cancer, previous treatments, and the patient’s overall health. Consequently, figuring a path that takes all these factors into account is critical for delivering the best outcome.
- High specificity in targeting mutated receptors
- Reduction of systemic side effects compared to classic chemotherapy
- Convenience of oral administration
- Encouraging early results in patient response rates
Even as TKIs have ushered in the era of personalized medicine, their long-term effectiveness continues to be studied. Researchers and clinicians alike agree that while the benefits are super important, combining therapies with other agents might improve outcomes further.
How Targeted Therapies Affect Lung Cancer Treatment Options
One of the most talked-about innovations in the treatment of EGFR-mutant lung cancer has been the emergence of chemo-free combination regimens. One such regimen, known as the MARIPOSA protocol, features a combination of Rybrevant (amivantamab-vmjw) and Lazcluze (lazertinib). This strategy is designed to provide a potent, yet more tolerable, alternative to traditional chemotherapy plus TKI combinations.
This approach has sparked discussions among clinicians who appreciate the reduced chemotherapy-related toxicities. Patients often find it less intimidating to engage in treatments that avoid the harsh side effects of chemotherapy, and doctors are excited because it can potentially open the door to more patient-friendly cancer management.
- Chemo-free options reduce the likelihood of severe side effects
- Improved patient adherence due to simpler administration
- Potential for similar efficacy when compared to traditional regimens
- High response rates in early clinical studies
Even as these novel combinations show promise, there are still several complicated pieces to work through. The long-term durability of these responses, the fine points of drug resistance and relapse, and the overall integration into existing treatment plans remain the subjects of ongoing research. It is this interplay of new data and traditional treatment experiences that is fueling hope in both medical circles and among patients.
Understanding the MARIPOSA Regimen: A Closer Look at the Chemo-Free Combination
The MARIPOSA regimen is leading the way in offering physicians another tool in managing the tricky bits of EGFR-mutant lung cancer. By combining Rybrevant, a targeted monoclonal antibody infusion, with Lazcluze, an oral pill, the regimen sidesteps the need for chemotherapy altogether. This combination has been reported to show similar levels of efficacy as traditional TKI plus chemotherapy approaches.
Specifically, clinical findings indicate that the response rate with this chemo-free regimen works in more than 80% of patients. What is particularly interesting is that the MARIPOSA approach minimizes the side effects that are generally associated with the nerve-racking adverse events of chemotherapy. Patients have found this approach to be less scary, potentially paving the way for it to become more widely accepted and implemented.
However, as with any new treatment, there come several subtle parts that require further exploration. It is still early days in terms of understanding the full duration of response, and cancer management is full of many small twists that demand ongoing observation and fine-tuning of treatment protocols.
Subcutaneous Versus Intravenous Delivery: Making Treatment More Patient-Friendly
Another critical advancement that has made waves in the oncology community is the adaptation of drug delivery methods. The recent transition from intravenous to subcutaneous delivery for combinations like Rybrevant plus Lazcluze is a testament to how patient care is evolving. The shift towards subcutaneous administration not only simplifies treatment but also adds a layer of convenience that many patients appreciate.
Traditionally, intravenous infusions have required patients to come to the hospital every two weeks. For many, this can be an overwhelming burden, particularly when combined with the nerve-racking uncertainties of a cancer diagnosis. By contrast, the newer subcutaneous method allows for dosing every four weeks, reducing the number of hospital visits and providing flexibility to administer treatments at home.
- Subcutaneous injections enable less frequent dosing
- Increased convenience for patients and caregivers
- Potential reduction in the overall anxiety associated with hospital visits
- Comparable efficacy between subcutaneous and traditional intravenous methods
Clinical trials such as the PALOMA-2 trial have shown promising data that subcutaneous delivery every four weeks, when combined with a daily oral pill, maintains similar effectiveness compared to the more frequent intravenous infusions. This advancement signifies a step forward in finding patient-friendly paths through cancer treatment, ensuring that the delivery of life-saving medications is as streamlined and efficient as possible. With better scheduling and fewer trips to the clinic, patients can enjoy more continuity in their daily routines while still receiving critical care.
The Impact on Quality of Life and Patient Experience
The evolution in treatment regimens isn’t just about clinical efficacy—it’s also about enhancing patient quality of life. When a regimen reduces the frequency of hospital visits and minimizes the risk of tough side effects, it directly impacts how patients cope with the disease on a daily basis. The less intimidating nature of the new subcutaneous delivery methods, for instance, plays a significant role in making the entire process less nerve-racking for patients and their families.
Patients are often faced with an array of decisions that involve navigating a maze of confusing bits and complicated pieces, where each option comes with its own set of risks and benefits. The recent developments in treatment—whether it’s the introduction of chemo-free regimens or the modification of drug delivery techniques—allow patients to find their way through the treatment process with more confidence. This added comfort can lead to improved adherence and a greater sense of control over the treatment journey.
Moreover, the modern methods also encourage a collaborative relationship between patients and healthcare providers. When patients feel that the treatment plan is designed with their lifestyle in mind, the trust between patients and doctors is reinforced. This trust is super important when it comes to managing not only the physical aspects of the disease but also the psychosocial challenges that often accompany a serious diagnosis.
Patient-Centered Advances: A Look at Convenience and Efficacy
Recent innovations in treatments for EGFR-mutant lung cancer reflect a broader trend in modern medicine: delivering care that is both effective and mindful of the patient’s lifestyle. Consider the following key advantages of the current advances:
- Simplified Regimens: Patients no longer need to contend with overly complicated schedules that make making your way through treatment more stressful.
- Outpatient and At-Home Options: The possibility of receiving subcutaneous injections at home reduces the need for constant hospital visits, allowing patients to maintain their normal routines.
- Lower Side Effect Burden: By reducing the reliance on conventional chemotherapy, newer combination regimens minimize the physical toll on patients, translating into better quality of life during treatment.
- High Response Rates: With response rates exceeding 80% in early studies, these treatments are showing promise in effectively controlling disease progression.
Each of these benefits is a testament to how far cancer treatments have come, serving as a reminder that the evolution of medicine is not solely about fighting disease but also about making life more manageable for those affected. The ability to provide consistent, effective, and less stressful treatment options is a win–win not only for patients and their families but also for the entire healthcare community.
Balancing Innovation with Safety: The Role of Ongoing Research
While the promise of new combination therapies and drug delivery systems brings optimism, it is essential to acknowledge that every innovative approach also comes with its set of challenges and hidden twists. The long-term effects of the chemo-free MARIPOSA regimen, for example, are still being studied. The fine shades and subtle details of drug resistance, potential relapse, and overall survival rates require additional trials and real-world data to fully understand.
It is critical that clinicians remain mindful of each patient’s unique circumstances. The seemingly straight-forward benefits observed in early-phase trials must be weighed against the possible long-term risks. Research is continuously evolving to address these tricky parts, with patient safety remaining at the forefront of every new development.
- Ongoing clinical trials help in fine-tuning these new regimens.
- Post-market surveillance ensures that any confusing bits are quickly addressed.
- Collaborative research between institutions offers a more in-depth look into long-term outcomes.
- Patient-reported outcomes are feeding into a more holistic view of treatment efficacy.
By continuing to probe these issues and figure a path forward through ongoing research, the oncology community is set on a trajectory that promises steady improvements. The key lies in the ability to balance the immediate needs for effective intervention with the self-evident requirement for safety and sustainability in long-term cancer care.
Fine-Tuning Treatment: The Little Details That Make a Big Difference
One of the most engaging aspects of these new treatment modalities is the way they address the nitty-gritty of patient needs. The improvements in drug delivery—such as the move from intravenous to subcutaneous infusions—are more than just technical adjustments. They are thoughtful responses to the living realities of patients who have to juggle treatment schedules with work, family, and daily obligations.
Some of the small distinctions that can make a world of difference include:
- Minimal Interference: Fewer clinic visits mean less disruption to everyday life, helping patients maintain a semblance of normalcy.
- Personalized Scheduling: Flexible dosing intervals allow treatment plans to be adjusted to suit individual lifestyles, making it easier to work through the treatment journey.
- Enhanced Monitoring: With the aid of telemedicine and home-based care options, patients can get timely advice from their healthcare providers without the anxiety of long trips to the hospital.
These small twists in the delivery and management of treatment serve as key benefits of modern cancer care. When patients can steer through their treatment with fewer interruptions to their personal lives, the overall success of the therapy can be further enhanced. In this way, every subtle part—from the drug composition to the method of administration—is a carefully thought-out piece of the larger puzzle in modern oncology.
Clinical Trials and Early Data: Interpreting the Latest Findings
While early data about the chemo-free MARIPOSA regimen and subcutaneous drug delivery is promising, many questions remain on the fine points of long-term efficacy. Researchers are now taking a closer look at patient populations, response durations, and the potential need for re-treatment or additional combination options when resistance emerges.
Current clinical trials are exploring several aspects of these treatments, including:
- Duration of Response: Determining how long the treatment maintains its effectiveness is one of the key measures of success.
- Side Effects Profile: Even with reduced toxicities, tracking every subtle detail of adverse reactions is critical for fine-tuning the regimen.
- Quality of Life Assessments: Understanding the real-world impact on patients helps ensure that the benefits of the treatments outweigh any potential drawbacks.
- Comparative Efficacy: Direct comparisons between the standard therapies and new combinations provide insights into which approach may be better suited for different patient groups.
Each of these aspects is loaded with challenges as well as potential rewards. In many ways, managing your way through the labyrinth of clinical data is much like finding your path through uncharted waters. Physicians, researchers, and patients are all working together to piece together the little details that will one day inform a new standard of care—a standard that promises not only improved survival but also a better quality of life.
Integrating Patient Preferences and New Standards of Care
The advent of these advanced treatment options is encouraging, but it also brings into focus the need for a more patient-centric approach in cancer care. Every new method, whether it’s the convenience of at-home subcutaneous injections or the formidable response rates seen with targeted combination therapies such as MARIPOSA, speaks to an underlying principle: personalized care matters.
Patient preferences are increasingly becoming a key part of the treatment discussion. Modern oncology now recognizes that offering patients the choice to decide how and when they receive their treatments can lead to better overall outcomes. It is super important for patients to have a say in their treatment, moving away from a one-size-fits-all approach to one that addresses each individual’s routine, psychological needs, and overall well-being.
- Flexible treatment schedules lead to fewer disruptions in daily life.
- Patient support services, including telehealth and home-based care, are gaining momentum.
- Enhanced communication between patients and care teams improves adherence to treatment regimens.
- Opportunities to adjust treatment plans in response to personal needs help reduce the mental and emotional toll of cancer therapy.
This growing emphasis on individualized care not only helps patients manage the physical side effects but also alleviates some of the overwhelming stress brought on by a cancer diagnosis. As the treatment community continues to adapt to these modern realities, the delicate balance between cutting-edge science and the quirky bits of everyday life remains at the heart of progress.
Addressing Concerns and the Way Forward: A Balanced View
Although much promise surrounds these innovative cancer treatments, the journey is not free from challenges. Critics point out that while early results are impressive, long-term data on survival, potential resistance, and overall safety is still developing. There are also concerns that the adaptation and integration of these novel therapies could be complicated by cost factors and logistical issues in some healthcare settings.
It is important to acknowledge these viewpoints as part of a balanced discussion. Here are some issues that remain under close observation:
- Cost and Accessibility: Advanced treatment options may come with high costs, raising questions about who gets access and how broadly they can be implemented across diverse healthcare systems.
- Long-Term Outcomes: While short-term benefits are evident, the length of time these improved response rates last is still a subject of ongoing research.
- Potential for Drug Resistance: As with any targeted therapy, the possibility of cancer cells developing resistance over time remains an area that requires thorough monitoring.
- Implementation Challenges: Transitioning from traditional intravenous infusions to subcutaneous methods requires training, infrastructure, and sometimes, a change in established clinical processes.
These are not insurmountable issues. In fact, the medical community is already working through these tricky parts. With each new study, pilot program, and patient experience report, the oncology field gets closer to refining these treatments. The goal is clear: to deliver therapy that not only extends life but makes the journey as manageable as possible for everyone involved.
Looking Ahead: The Future of EGFR-Mutant Lung Cancer Treatment
The future of cancer treatment, especially for conditions like EGFR-mutant lung cancer, is full of both promise and challenging twists. With ongoing research and the introduction of innovative techniques, the treatment protocols are set to become even more personalized and patient-friendly. Among the key areas of future focus are:
- Refinement of combination regimens that optimize efficacy while minimizing side effects.
- Expansion of home-based and outpatient treatment models that ease the day-to-day burden on patients.
- Personalized medicine strategies that integrate genomic data, real-world evidence, and patient preferences to tailor therapy.
- Strengthening support networks, including digital health and telemedicine, to drive continuous monitoring and improve quality of life.
When we take a closer look at these factors, it is clear that every small adjustment and thoughtful improvement can lead to a significant impact on patient outcomes. While there are still many confusing bits to work through, the momentum is building. With each study, patient survey, and clinical report, the treatment community is steadily piecing together the large jigsaw puzzle of effective cancer management.
There is also an important cultural shift towards viewing patients as partners in their care. Every decision—from the selection of a specific TKI to the choice between subcutaneous and intravenous delivery—now involves detailed discussions that incorporate a patient’s lifestyle, personal preferences, and long-term goals. In many ways, this is a welcome change, as it makes the treatment process less intimidating and more adaptable to individual needs.
Conclusion: Embracing a New Era in Cancer Treatment
In conclusion, the evolution of treatment options for EGFR-mutant lung cancer marks an inspiring new chapter in oncology. The introduction of sophisticated, tailored therapies and innovative drug delivery methods such as the MARIPOSA regimen and subcutaneous injections offer not only improved clinical efficacy but also a remarkable enhancement in patient quality of life.
Patients now have access to regimens that are designed to steer through the complicated pieces of their cancer treatment in a way that minimizes disruption and maximizes convenience. The ongoing research and clinical trials continue to address the subtle details and hidden challenges associated with these therapies, paving the way for future improvements that may one day render cancer a much less intimidating opponent.
As we look ahead, it is critical to keep in mind the balancing act of embracing innovation while ensuring patient safety. More than ever, individual patient needs and real-world experiences drive the way forward in oncology. The community’s commitment to refining every little twist of treatment—from drug composition to delivery method—is helping to create a future where effective cancer care truly becomes a well-organized partnership between clinicians and patients.
Ultimately, by managing your way through these transformative breakthroughs and keeping patient welfare front and center, modern medicine is making strides that could redefine the standards of cancer care. It is a future where every new therapeutic development builds upon the lessons of the past, integrating scientific breakthroughs with the practical needs of those who face the daily reality of living with cancer.
This ongoing dialogue between research and real-world application is not just a clinical necessity; it is a moral imperative in our struggle to demystify complex treatment approaches and make them as accessible as possible. Only by working together—through thoughtfully designed clinical trials, patient-centered care models, and constant re-evaluation of treatment efficacy—can we truly celebrate a time when life-saving therapies are not only effective but also kind to the lives of those who need them most.
The landscape of lung cancer treatment, particularly for EGFR-mutant cases, has evolved beyond the labyrinth of complicated pieces and nerve-wracking side effects. With innovative strategies like the MARIPOSA regimen and smarter drug delivery methods, the future looks promising. The journey through these tricky parts is far from over, but every step moves us closer to a reality where cancer care is synonymous with understanding, efficiency, and genuine compassion for the patient experience.
Originally Post From https://www.curetoday.com/view/current-treatments-and-new-combinations-in-egfr-mutant-lung-cancer
Read more about this topic at
A New Frontline Standard in the Treatment of EGFR-Mutant …
a network meta-analysis and systemic review – PMC