Redefining the Cancer Treatment Journey: A Local Perspective on Comprehensive Care
In today’s fast-paced world, where information is available at the blink of an eye, finding your way to the best possible healthcare can sometimes feel overwhelming. Yet, when it comes to cancer care, especially in our local communities, there is a pressing need for comprehensive, patient-centered services that embrace every aspect: physical, emotional, and even spiritual. The recent initiatives led by renowned institutions like the AtlantiCare Cancer Care Institute offer an illuminating example of what modern, community-based oncology care looks like.
In this opinion editorial, we get into the details of how advanced cancer treatment, integrated support services, and multifaceted care teams work together to lighten the load for patients. We also consider the importance of addressing the tricky parts of cancer diagnosis and treatment planning while keeping the patient’s well-being at the forefront.
Personalized Treatment Plans: Making Sense of Tangled Issues
One of the standout elements of modern cancer care is the creation of personalized, patient-specific treatment plans. For many patients, the process of dealing with a cancer diagnosis can be filled with confusing bits and complicated pieces. No two cancers or their impacts on individuals are exactly the same. What works seamlessly for one person may not be effective for another. Therefore, the concept of tailored treatment plans is super important.
When patients have the opportunity to work with a team of experienced professionals, the experience can be transformed. The specialists at leading institutions really focus on creating these individualized plans. With the collaborative approach embraced by oncology experts, patients are no longer just faced with a scary or intimidating treatment plan that appears overwhelming. Instead, each plan is crafted to fit the specific characteristics of the patient’s condition, lifestyle, and even personal beliefs.
The process starts from the moment of diagnosis and continues through to post-treatment follow-up. Physicians, nurses, social workers, dietitians, and even spiritual counselors join in on this journey, ensuring that the patient always feels supported. The real beauty of this method is that it addresses both the medical needs and the emotional and nutritional facets of recovery.
Key Benefits of Personalized Cancer Treatment
The benefits of personalized treatment plans include:
- Reduction in the nerve-racking uncertainty about treatment options.
- Increased confidence in the treatment process for patients and families.
- A sequential plan that addresses both short-term symptoms and long-term recovery goals.
- Enhanced communication between the patient and the healthcare team, ensuring a sense of control over the process.
Taking the time to create a unique plan for every patient not only improves the odds of success but also helps families steer through the intricate, often intimidating journey that is cancer treatment.
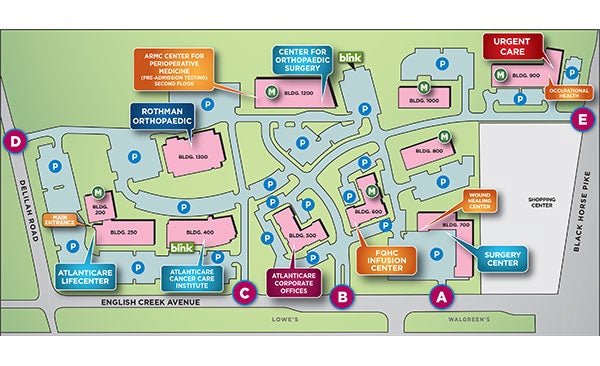
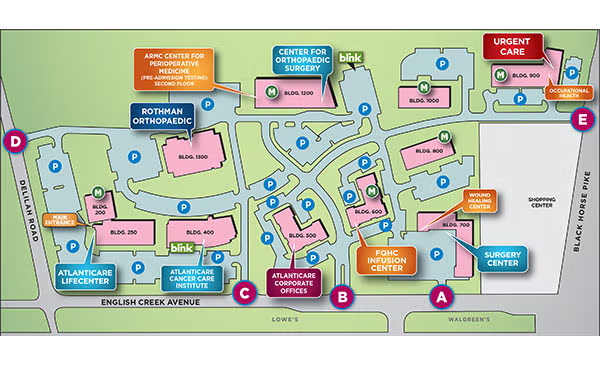
Community-Based Cancer Care: Less Traveling, More Healing
Another important aspect of modern cancer care is its focus on being accessible in local communities. Staying close to home means less traveling for patients—a factor that is absolutely essential for those fighting a tough battle. Treatment centers like those in the AtlantiCare network are designed to be accessible, reducing the strain that long-distance travel can place on already stressed patients and families.
By establishing treatment facilities in local neighborhoods, healthcare providers create a network of care that is both convenient and compassionate. This local availability allows patients to interact frequently with their healthcare team, leading to better communication, faster response times, and overall improved outcomes. In a world where every bit helps, having these resources readily available makes a tremendous difference.
The Advantages of Localized Services
Some of the key advantages of community-based services include:
- Enhanced accessibility: Easier access to treatment centers means quicker diagnosis and follow-up care.
- Improved continuity of care: Patients see the same expert team throughout their treatment, building trust over time.
- Lower travel stress: Especially during rigorous treatment schedules, less travel reduces additional strain.
- Community-driven support: Local programs and support groups provide an extra layer of emotional support.
When healthcare providers set up local stations, they not only support the patient medically but also tap into the existing community networks. This integration creates a more resilient healthcare environment, allowing patients better overall results by staying in a familiar and comforting locale.
Multidisciplinary Approach: Working Through the Confusing Bits Together
The idea behind multidisciplinary care is that patients are best served when various experts work together to create a comprehensive treatment plan. In the context of cancer care, this involves oncologists, radiologists, surgeons, nurses, nutritionists, and counsellors. Each professional brings a unique skill set, ensuring that every little detail is looked after during the journey. The collaboration makes it possible to tackle the tricky parts of a cancer diagnosis from every angle.
Working through these tangled issues collaboratively means that no single aspect of the disease is left unattended. For example, when surgical oncologists and radiation experts team up, patients benefit from a dual-approach that considers both invasive and non-invasive treatment options. Such teamwork leads to a far more nuanced understanding of a patient’s condition, even when the fine points seem complicated or overly detailed.
Table: Multidisciplinary Team Members and Their Roles
| Team Member | Role in Care |
|---|---|
| Medical Oncologist | Determines chemotherapy and systemic treatment |
| Radiation Oncologist | Plans and administers radiation treatment |
| Surgical Oncologist | Performs surgical interventions if necessary |
| Nursing Team | Provides direct patient care and treatment preparation |
| Dietitian | Advises on nutrition plans to bolster recovery |
| Social Worker & Counselor | Delivers emotional and psychological support |
| Pharmacist | Manages drug therapies and interactions |
This table clearly shows the wide variety of experts involved in managing the nerve-racking yet essential journey toward recovery. Each professional plays a key role in designing an effective and balanced treatment plan, ensuring that every aspect of patient care is thoughtfully integrated.
Embracing Innovation: Leading-Edge Treatments and Clinical Trials
Innovation in treatment is a significant factor in transforming cancer care from purely reactive procedures to proactive, precise interventions. Leading centers are continuously at the forefront of new discoveries—introducing treatments that were once considered off-limits or experimental. Being part of ongoing clinical trials means that patients sometimes have access to groundbreaking therapies long before they become mainstream.
These advanced treatments are developed to address even the most tricky parts of cancer care, where traditional methods may fall short. With robotics-assisted procedures such as robotic bronchoscopy for lung cancer and precision radiation therapies, patients can experience treatment methods that are more effective and less invasive. Moreover, clinical trials offer a lifeline for those who have exhausted standard options, providing a new direction in care and hope for recovery.
How Clinical Trials Make a Difference
Participating in clinical research not only helps an individual patient but also contributes to the broader understanding of cancer and its most challenging aspects. Key points include:
- Access to cutting-edge therapies: Sometimes the latest treatment options are only available through clinical trials.
- Personalized care: Trials contribute to developing tailored therapies that consider each patient’s unique condition.
- Increasing survival rates: Innovative treatments can provide improved outcomes compared to standard protocols.
- Future implications: Contributions to research today guide the next generation of oncology care.
Clinical trials serve as a beacon for patients who are determined to beat the disease. These studies focus not only on the outcomes of treatment but also on the overall enhancement of life quality for those affected. To truly appreciate these benefits, patients and families are encouraged to speak with their healthcare providers about potential trial eligibility and the implications for their treatment plans.
Building Trust Through Compassionate Support Services
The fight against cancer isn’t solely fought in hospital rooms and laboratories; it is also a battle waged on an emotional front. With the many confusing bits and nerve-racking twists along the way, patients often need more than just medical expertise. Support services such as counseling, nutritional therapy, and community support groups are designed to tackle these subtle parts of emotional distress and lifestyle changes during treatment.
One of the strongest elements of comprehensive care is the integrated support that goes hand in hand with treatment. Well-informed dietitians can help patients navigate through the intricacies of maintaining proper nutrition during chemotherapy, while trained social workers address issues that might be causing heavy emotional strain for both the patient and their families.
Support Services That Make a Difference
Support services are as important as medical interventions. Some major components include:
- Personalized Counseling: Individual or group sessions that address emotional and mental health.
- Nutritional Guidance: Tailored dietary plans to help maintain energy and promote healing.
- Oncology Nursing Support: Specialized nurses who prepare patients for chemotherapy and radiation therapy.
- Community Support Groups: Local gatherings that offer a soft space for sharing experiences and advice.
- Spiritual Counseling: Support to help address the spiritual aspects of healing, providing balance through moments of doubt.
Offering such a wide array of support measures represents a holistic approach to cancer care where the patient and their family are never left feeling isolated in their fight. These elements work together to build trust and create an environment that is both nurturing and proactive in its approach to healing.
Integrating Modern and Alternative Therapies for Whole-Person Wellness
In recent years, there has been a growing conversation about blending modern medicine with alternative approaches to meet the whole-person wellness needs of cancer patients. For many, conventional treatments such as chemotherapy, surgery, or radiation are complemented by practices like mindfulness, yoga, acupuncture, and nutritional supplements. This integrated approach helps manage the emotional and physical toll often loaded with issues that accompany a cancer diagnosis.
Alternative therapies can work as supportive measures, easing side effects of intense treatments and improving overall life quality. For example, meditation and yoga help alleviate stress and anxiety, making it easier to manage the nerve-racking feelings associated with treatment. On the other hand, acupuncture may assist in controlling pain and nausea, while nutritional plans ensure that patients have the energy to fight back.
Benefits of Integrative Approaches in Cancer Care
By combining modern and alternative methods, patients often experience benefits such as:
- Enhanced physical recovery: Techniques like acupuncture and massage therapy can relieve pain and improve circulation.
- Improved mental health: Mindfulness and meditation help reduce anxiety and create a positive outlook.
- Reduced side effects: Alternative approaches often assist in diminishing the physical side effects of aggressive treatments.
- Empowerment: Patients feel more in control when allowed to participate in decisions about complementary therapies.
This integration does not replace conventional methods, but instead, enhances them. It’s a balanced, medically informed approach that respects the body’s innate healing powers while still applying modern science where it counts. Ultimately, this creates a space where every patient can find their personal road to recovery.
Patient Empowerment and Informed Decision Making
The shift in cancer care towards a more patient-centered model has allowed individuals to be more engaged in their treatment decisions. Patients are encouraged to ask questions, seek second opinions, and voice their personal preferences when it comes to the available options. This empowerment not only builds trust but also reduces the fear that often comes with the many twists and turns of a cancer diagnosis.
Being well-informed is a must-have in this era of rapid medical advancement. When patients feel capable of making educated decisions—whether it be understanding treatment risks, learning about side effects, or considering enrollment in clinical trials—they experience a greater sense of control. This makes the nerve-racking moments of uncertainty a little less intimidating.
Steps to Enhance Informed Decision Making
Patients can take several steps to become more empowered in their cancer care, including:
- Gathering Information: Researching treatment options and reading up on alternative therapies can help demystify the process.
- Engaging with Healthcare Teams: Regular discussions with the multidisciplinary team allow for staying updated on the latest developments.
- Attending Support Groups: Sharing experiences with others can provide practical advice and emotional relief.
- Utilizing Patient Portals: Many hospitals now offer online systems where patients can access their records, upcoming appointments, and treatment plans.
These steps not only help patients feel better prepared for treatment, but also promote a collaborative environment where decisions are made together, ensuring the best possible care outcomes.
Technology and Healthcare: Transforming the Oncology Experience
Technology plays a super important role in modern cancer care. Innovations such as electronic patient portals, advanced diagnostic imaging, and telemedicine have significantly changed the way patients access and manage their care. These technological breakthroughs can help reduce the confusing bits of the medical process by making information more accessible and streamlining communications between patients and healthcare providers.
For instance, the use of telemedicine in follow-up care allows patients to have consultations without the added strain of traveling—ideal for those already weary from treatment. Digital platforms also facilitate smoother scheduling, remote monitoring, and even provide educational materials that patients can access at any time. This not only helps in making the process less off-putting but also boosts patient confidence and satisfaction.
The Impact of Technology on Patient Experience
Technology has reshaped patient care in numerous ways:
- Enhanced communication: Digital communication tools allow for quick consultations and efficient sharing of test results and treatment updates.
- Remote monitoring: Devices and apps enable healthcare providers to keep track of patient progress outside the clinic.
- Accessible educational resources: Informational websites, webinars, and online support groups help patients learn more about their condition.
- Simplified administrative processes: Online bill payments, appointment scheduling, and access to health records streamline the patient experience.
This digital shift not only makes the healthcare system more efficient but also directly addresses the hardships that patients might experience when trying to get around a complicated healthcare process. The convenience provided by modern technology is a significant factor in reducing some of the nerve-racking challenges that come with the cancer care journey.
Holistic Wellness: Beyond the Medical Treatment
While advanced treatment options and technology are key, a truly successful cancer care program also focuses on overall wellness. The journey does not end with the last dose of chemotherapy or after the final radiation session. Healing is a long-term process that involves building resilience, reconnecting with oneself, and maintaining a balanced lifestyle. Many centers now include wellness programs that combine physical rehabilitation, nutritional planning, and even lifestyle coaching.
A holistic approach to cancer care considers the full spectrum of well-being. This means that while the medical side of treatment is essential, the mental and emotional recovery process is equally critical. Custom-tailored wellness programs can help survivors manage lingering side effects, overcome fatigue, and regain a sense of normalcy after treatment. In essence, holistic care embraces both body and mind, turning the challenging journey into an opportunity for a complete and fulfilling recovery.
Components of a Holistic Wellness Program
A comprehensive wellness program during and after cancer treatment may incorporate:
- Physical rehabilitation: Exercise classes, light physiotherapy, and personal training sessions tuned to the patient’s condition.
- Nutritional counseling: Guidance on meal planning and supplements that help rebuild strength.
- Mental health support: Access to counseling sessions, meditation classes, and stress management workshops.
- Social engagement: Support groups and community programs to foster interpersonal connections and morale.
These elements work in tandem to create a supportive environment that encourages recovery and helps survivors feel equipped to manage the road ahead. By addressing both the tangible medical needs and the subtle emotional challenges, this approach creates a resilient, balanced outlook on post-treatment life.
Future Directions in Cancer Care: From Research to Real-World Application
Looking to the future, cancer care continues to evolve. The commitment to integrate research, technological innovation, and patient-centered methodologies suggests a promising path forward. Clinical trials, personalized medicine strategies, and the expansion of support networks are paving the way for next-generation oncology treatments that combine state-of-the-art science with the compassionate care that patients deserve.
One of the most appealing aspects of modern cancer care is its flexibility and willingness to adapt to the small distinctions and fine shades that characterize each patient’s unique journey. Researchers and clinicians alike are constantly exploring innovative methods to manage the tricky parts and tangled issues associated with cancer, ensuring that even the most nerve-racking aspects of the diagnosis and treatment process are addressed with sensitivity and expertise.
Emerging Trends in Oncology
Some of the emerging trends that are shaping the future of cancer care include:
- Precision Medicine: Treatments tailored to the genetic profile of both the patient and the tumor, offering super important customization.
- Immunotherapy Advances: Boosting the body’s own immune system to fight cancer cells more effectively.
- Enhanced Imaging Techniques: Better diagnostic tools that provide clearer insights into tumor behavior and treatment progress.
- Telehealth Expansion: Increasing accessibility to healthcare services through remote consultations and monitoring.
The convergence of these trends is set to redefine what is possible in cancer care. With ongoing investments in research and technology, the hope is that future treatments will become even less intimidating and more efficient, turning the tide for many who face this challenging disease.
Conclusion: Charting the Path Toward a More Compassionate Oncology Future
As we witness the evolution of cancer care, it is clear that the future lies in a balanced approach: one that integrates modern, cutting-edge treatments with heartfelt, holistic care. The AtlantiCare Cancer Care Institute stands as a beacon of hope in our communities, showcasing how a combination of innovative therapies, supportive services, and a strong commitment to personalized care can transform the patient experience.
In our ever-changing healthcare landscape, the narrative is shifting from one of fear and uncertainty to one of empowerment, clarity, and comprehensive wellness. Patients are starting to see that when every subtle part of their condition is addressed—from physical treatment to emotional healing—they are embarking on a journey that offers not only survival but also the possibility of a fulfilling, quality life.
Healthcare providers and community leaders must continue to invest in local facilities, multidisciplinary teams, and integrated support mechanisms. By doing so, they help figure a path that eases the twists and turns of cancer care, ensuring that each patient is met with a team of dedicated professionals, innovative treatments, and an extensive network of support.
Ultimately, the shared goal of advancing cancer care is clear: to create an environment where every patient can access the best treatment options without the extra burden of long-distance travel, excessive stress, or overwhelming complexity. As we look ahead, it is our collective duty to support initiatives that prioritize what truly matters—compassionate, comprehensive care that empowers individuals to reclaim their lives in the face of cancer.
This community-driven approach to oncology is the roadmap for the next chapter in cancer care. With continuous improvements in technology, personalized treatment strategies, and holistic wellness programs, the future is bright for patients and their families. The true measure of success in this field lies not only in survival rates but also in the restoration of hope, dignity, and the promise of a healthier life.
Getting Involved: Community Resources and Patient Advocacy
For those seeking more information or personal guidance as they navigate the sometimes intimidating world of cancer care, there are many resources available. Local centers often provide direct lines of communication to support services, patient education programs, and advocacy groups. These organizations are there to help patients take the wheel of their treatment journey, ensuring that every decision made is based on informed choices and backed by expert insight.
Here are a few steps to get started on this empowering path:
- Consult with Your Physician: Discuss personalized treatment plans and explore all available options.
- Explore Local Support Groups: Engage with community groups that offer shared experiences and critical emotional support.
- Investigate Wellness Programs: Look for holistic care options that focus on both physical and mental wellbeing.
- Stay Updated on Innovations: Follow reputable healthcare websites to learn about upcoming therapies and clinical trials.
- Utilize Online Patient Portals: Access your health records and manage appointments with ease.
Being proactive about understanding all the little details can simplify the decision-making process and ease the tension often associated with a cancer diagnosis. Advancing based on self-education and expert consultation paves the way for better outcomes and a more empowered future.
Embracing a Future Built on Collaboration and Compassion
In conclusion, the journey through cancer care is marked by many challenging twists and turns. Yet, with the right blend of personalized treatments, integrated support services, and ongoing innovation in both technology and research, there is promising reason for optimism. By making care accessible within the community and embracing a truly multidisciplinary approach, institutions like the AtlantiCare Cancer Care Institute provide a template for compassionate, effective treatment that meets patients where they are.
Every step forward in the field of oncology represents progress not just for the science of medicine, but for the countless individuals whose lives are touched by cancer each day. It is a reminder that amidst the tangled issues and nerve-racking moments, there is always hope—a hope that is built on community, collaboration, and the unyielding determination to turn difficult challenges into pathways for healing and recovery.
As healthcare continues to evolve, one thing remains constant: the critical need for care that addresses every facet of a person’s story. When modern medicine meets empathetic support, when technology complements traditional treatments, and when healthcare providers work hand in hand with communities, the outcome is far more than just improved survival rates. It is a future where every patient feels supported, understood, and empowered to live a full and vibrant life after cancer.
The conversation about cancer care will always be evolving, and every new advancement brings us one step closer to a world where the battle against cancer is met head-on with innovation, compassion, and unity. It is an exciting time for the field, and, ultimately, a step toward a brighter, healthier future for all.
Originally Post From https://www.atlanticare.org/services/cancer-care/specialties
Read more about this topic at
Indiana University Melvin and Bren Simon Comprehensive …
IU Health Simon Cancer Center – Indianapolis