Managing Breast Cancer Radiation Adverse Effects: An Opinion Editorial
This editorial seeks to explore the many sides of adverse effects associated with breast cancer radiation therapy. Today’s radiation oncologists face a range of tricky parts—from preventing skin issues like radiation dermatitis to tackling rare but nerve-racking problems such as brachial plexopathy. In this opinion piece, we take a closer look at these issues, review management strategies, and highlight the importance of early intervention and interdisciplinary care, all while offering practical insights for both patients and healthcare professionals.
Understanding the Scope: Radiation Therapy in Breast Cancer
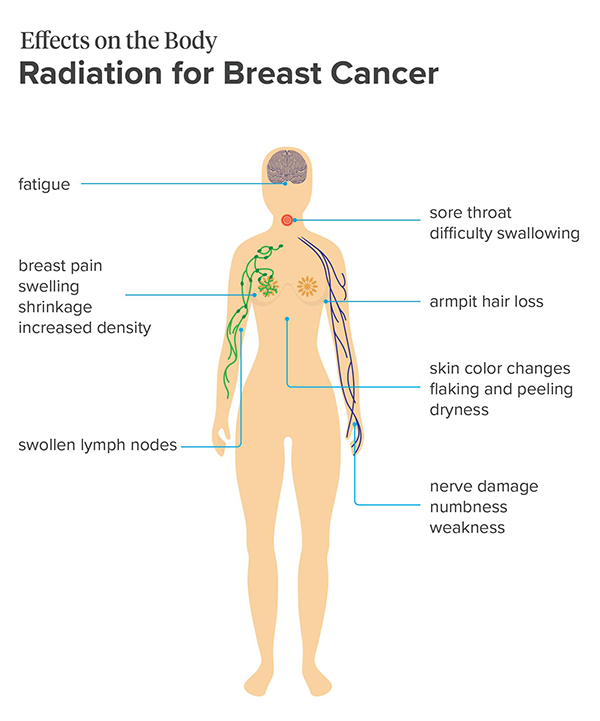
Breast cancer radiation therapy is an essential tool in reducing the risk of local tumor recurrence. Yet, as with any treatment, it comes with its share of tangled issues. The adverse effects largely hinge on the area that receives radiation, meaning that complications can vary from skin conditions to deeper organ toxicities. The experience is often a mix of essential treatment benefits and the challenge of managing side effects.
The discussion that follows is not meant to discourage patients but to better inform them of the possible changes they might face. Radiation therapy is super important for improving patient outcomes, and understanding these effects—and how to manage them—is a key part of modern cancer care.
Preventing and Managing Radiation Dermatitis
Essential Tips for Preventing Skin Irritants
One of the most common and visible adverse effects of breast cancer radiation is radiation dermatitis. This condition typically presents as a sunburn-like reaction with dryness, erythema, or even moist desquamation as the treatment intensifies. The challenge is to prevent this painful condition from progressing while making the treatment tolerable for patients.
Healthcare professionals are encouraged to take a proactive approach. Some effective strategies to prevent or reduce the severity of radiation dermatitis include:
- Regular use of moisturizers to maintain skin hydration
- Application of calendula-based topical treatments
- Daily use of low-dose topical steroids, like 0.1% mometasone
- Utilization of barrier films such as Mepitel to protect the skin from friction and irritants
Once treatment initiates, mild (grade 1) dermatitis resembles a faint sunburn. At this stage, maintaining a personalized regimen that might include over-the-counter analgesics such as ibuprofen—as well as saline, sitz, and vinegar soaks—can significantly ease the discomfort. It’s crucial to tailor these treatments to the patient’s experience, as every individual’s reaction is unique.
Managing More Severe Skin Complications
As the condition progresses to mild-to-moderate stages (grades 2 and 3), patients might develop moist desquamation and blistering. The management plan must then shift gears to more advanced interventions. These can include:
- Topical silver sulfadiazine for its antimicrobial properties
- Medicated soaks with products like Domeboro to soothe rashes
- Hydrocolloid dressings that can protect the affected area and facilitate healing
- Triple antibiotic creams or even systemic oral antibiotics like cephalexin if an infection is suspected
In rare but severe cases (grade 4), the dermatitis may show hemorrhage or necrosis. For these patients, a referral to wound management specialists is essential, and radiation treatment may need to be temporarily halted to allow for proper healing. This layered approach ensures that while the radiation works to control cancer, the skin is given the best chance to recover.
Tackling Lymphedema: When Swelling Takes Hold
Identifying Early Signs and Preventative Measures
Lymphedema is another common consequence of radiation therapy to the breast, manifesting most commonly in the arm of the treated side—sometimes noticeably enlarging the limb. It may also appear around the chest and axilla. The onset of lymphedema can be concerning, but early identification and expert management can help mitigate its impact.
Strategies to curb lymphedema’s negative effects include early referral to lymphedema therapy clinics. In these specialized settings, occupational therapists work with patients to develop home programs that involve:
- Proper use of compression devices
- Gentle exercises designed to promote lymphatic drainage
- Manual lymphatic drainage techniques to aid circulation
This interdisciplinary approach is super important. By involving multiple experts, patients can be confident that every little detail of their care—from physical therapy to occupational therapy—is well considered.
Finding Your Path Through Long-Term Management
Not every patient has immediate access to a specialized lymphedema clinic. Nowadays, healthcare providers are learning to find their way around such situations by researching local physical therapy and occupational practices that specialize in lymphedema management. Making phone calls to verify expertise and reading patient reviews can be a practical way to connect patients with the right help. This grassroots approach underscores the value of personalized patient care in overcoming the nerve-racking challenges that lymphedema can impose.
Addressing Late Effects: Cardiac Toxicities, Fibrosis, and Pneumonitis
Understanding the Risks to the Heart
Cardiac toxicities are among the more intimidating long-term effects of radiation, particularly for patients with left-sided breast cancer. When the heart is in close proximity to the radiation field, the risk of complications such as coronary artery disease, cardiomyopathy, valvular issues, arrhythmias, and pericarditis increases.
To reduce these risks, radiation teams often implement techniques like deep inspiration breath hold (DIBH). This method involves patients taking deep breaths and holding them momentarily during radiation delivery. By doing this, the heart can be moved away from the chest, effectively reducing its exposure. The idea is to protect the heart while ensuring that the radiation effectively targets the breast tissue.
While many patients do not require a referral to a cardiologist, those with preexisting heart conditions may benefit from further cardiovascular assessment through tests like echocardiograms, stress tests, or comprehensive lipid profiles. Interventions may include medications such as statins, beta blockers, ACE inhibitors, or antiplatelet therapy to manage emerging cardiac issues. In cases where pericarditis develops, non-steroidal anti-inflammatory drugs (NSAIDs) can offer relief.
Fibrosis and Lung Complications: Managing the Hidden Complexities
Late radiation effects are not just limited to the heart, however. Fibrosis, which involves tissue thickening and scarring, is a common late effect that can affect various tissues in the chest. This includes both the breast tissue and nearby organs. The process of fibrosis can be a tangled issue that might restrict function and cause discomfort.
Management of fibrosis involves a combination of physical therapy to maintain tissue flexibility and the use of medications such as pentoxifylline combined with vitamin E, intended to address the underlying tissue changes. Additionally, pneumonitis—a condition that can evolve into pulmonary fibrosis—is more typically linked to thoracic cancers but remains a concern in the breast radiation setting. Early detection and prompt treatment are key to preventing progression to more serious lung damage.
Dealing with Skin Changes: Hyperpigmentation, Telangiectasia, and Volume Loss
Understanding Super Important Late Skin Effects
Radiation therapy can lead to permanent skin changes that may affect patients’ quality of life. Hyperpigmentation, characterized by the overproduction of melanin, often manifests as a darker, uneven skin tone in the treated area. Similarly, telangiectasia—where small blood vessels become visibly enlarged—can lead to a red, spider-web appearance on the skin.
Both conditions are not only cosmetic concerns but can also be a source of emotional distress for patients. Effective solutions include laser therapy sessions that target these small twists and turns in the skin’s appearance, offering a chance for significant improvement. In conjunction with hydrophilic moisturizers, these treatments can alleviate some of the stress associated with visible skin changes.
Setting the Record Straight on Breast Volume Loss
In some cases, patients who have undergone both partial mastectomy and radiation may experience changes in breast contour or volume. The tightening of tissue can lead to noticeable volume loss, affecting body image and overall satisfaction with treatment outcomes. For these patients, options such as suitable prostheses or surgical corrective procedures can restore a sense of normalcy. Some institutions even offer custom-fitted support garments which are tailored to enhance comfort and improve aesthetic outcomes.
Rare but Concerning: Costochondritis and Brachial Plexopathy
Identifying and Managing Rib Irritations
While rare, costochondritis—an inflammation of the rib cartilage—can occur as an acute adverse event following breast radiation therapy. Patients with costochondritis typically experience significant chest wall pain, which can be mistaken for other forms of toxicity. The condition is generally manageable with NSAIDs, with dosages ranging from 200 to 800 mg of ibuprofen being effective for many patients.
It is important for both patients and clinicians to be aware of this possibility, as early identification and treatment can prevent symptoms from becoming overwhelming. The management here hinges on carefully monitoring the level of discomfort and ensuring that appropriate analgesics are used to provide relief without interfering with the overall radiation treatment plan.
Tackling Nerve-Related Concerns: Brachial Plexopathy
Brachial plexopathy represents one of the more nerve-racking late effects of radiation therapy. This condition, resulting from damage to the network of nerves responsible for arm and shoulder movement, can lead to symptoms such as numbness, pain, tingling, and muscle weakness. The management of brachial plexopathy requires a careful, multidisciplinary approach.
Therapeutic strategies include the use of anticonvulsant medications that work as gamma-aminobutyric acid (GABA) analogs—such as gabapentin or pregabalin—along with dedicated physical and occupational therapy to help restore function. Despite its rarity, the possibility of brachial plexopathy underpins the need for continual assessment and adaptation of radiation treatment plans to safeguard surrounding tissues.
Summary of Radiation-Related Adverse Effects and Management Strategies
To help clarify the various side effects and their management, consider the table below, which outlines common issues and the corresponding interventions:
| Adverse Effect | Signs/Symptoms | Management Strategies |
|---|---|---|
| Radiation Dermatitis | Erythema, dry or moist desquamation, blistering |
|
| Lymphedema | Swelling of the arm, chest, or axilla |
|
| Cardiac Toxicities | Arrhythmia, coronary artery disease, pericarditis |
|
| Fibrosis & Pneumonitis | Tissue scarring, thickening, breathing difficulties |
|
| Skin Changes (Hyperpigmentation, Telangiectasia) | Discoloration, visible blood vessels |
|
| Costochondritis | Rib pain and tenderness |
|
| Brachial Plexopathy | Numbness, tingling, weakness in arm/shoulder |
|
This table is offered as a tool to help doctors and patients figure a path through the various treatment options and side effects. It lays out the small distinctions in treatment approaches for every type of adverse effect one might encounter.
Interdisciplinary Care: A Super Important Element in Radiation Management
The complexity of managing these adverse effects highlights the importance of interdisciplinary care. Radiation oncologists, nurse practitioners, physical therapists, and even cardiologists must work together to figure a path that maximizes treatment outcomes while minimizing discomfort. This collaborative approach ensures that the many confusing bits of cancer treatment are addressed in a holistic manner.
For instance, the early involvement of lymphedema therapists not only helps manage arm swelling but also protects long-term shoulder mobility. Likewise, engaging cardiologists in cases where heart exposure is a concern can reduce later cardiac complications. In every step of the way, the strategy is to smooth out the twists and turns inherent in radiation therapy.
Patient Empowerment and Self-Advocacy
Patients play a key role in the management of their own care. Being informed about potential side effects and the available treatment options can empower patients to speak up if they notice early signs of complications. Here are some practical tips for patients to keep in mind:
- Keep a detailed symptom diary: Note any skin changes, pain levels, or unusual sensations so that your healthcare team can assess the situation promptly.
- Ask about prophylactic treatments: Don’t hesitate to inquire about preventive measures, such as moisturizers or compression garments, that might reduce the risk of side effects.
- Stay proactive with follow-up: Regular check-ups with your treatment team are essential for catching and managing issues before they become overwhelming.
- Connect with support groups: Sharing experiences with other patients can be invaluable for learning how to handle the nerve-racking aspects of treatment.
By taking the wheel in discussions about their care, patients can ensure that subtle details—those fine shades of discomfort or improvement—are addressed promptly and efficiently.
The Future of Adverse Effect Management in Radiation Therapy
As we look ahead, ongoing research and technological advancements promise to further refine the management of radiation adverse effects. For example, improvements in imaging and radiation delivery techniques continue to reduce off-target exposure, thereby lowering the risks of both acute and late complications.
Furthermore, integration of artificial intelligence in treatment planning is likely to play a role in predicting which patients might develop more complicated pieces of side effects. Such predictive models could lead to early, personalized interventions that improve the overall therapeutic experience.
New medications and topical agents are also being explored to better treat and even prevent the nitty-gritty of radiation-induced tissue damage. The feedback loop between clinical research and patient care is more robust than ever, meaning that strategies that work today may soon be refined into even more effective interventions.
Policy and Practice: Enhancing Supportive Care
Beyond the clinical perspective, there is a growing debate on the need for better supportive care protocols and insurance coverage for post-treatment care. Healthcare policies that emphasize early and integrated management of radiation adverse effects could change the landscape of cancer survivorship. Patients deserve interventions that are not only reactive but also preemptive in averting the awkward moments when side effects become too overwhelming.
Stakeholders across the board—from medical practitioners to policy makers—must work together to ensure that support services, like lymphedema therapy and wound care for radiation dermatitis, are available and easily accessible. The goal is to create a system that allows patients to tackle every small twist with confidence and clarity.
Conclusion: A Balanced Perspective on Breast Cancer Radiation Management
In summary, the journey of radiation therapy for breast cancer is one of high stakes combined with the reality of managing multiple, often interconnected, side effects. From acute skin reactions to late cardiac toxicities, the entire treatment process is laden with potential challenges. However, with an interdisciplinary approach, early intervention, and patient empowerment, these challenges can be managed effectively.
This opinion editorial does not aim to alarm but rather to shed light on the practical, day-to-day management of the confusing bits of radiation therapy. It reminds all involved that proactive care, personalized treatment plans, and effective communication between patients and their healthcare teams are super important for ensuring the best possible outcomes.
Ultimately, while radiation therapy remains a cornerstone in breast cancer treatment, the emphasis must remain on mitigating its side effects. With ongoing research, better technology, and a commitment to comprehensive care, we are steadily moving towards a paradigm where the benefits of radiation are maximized while the adverse events are minimized. This balanced approach is the key to not only curing cancer but also preserving the quality of life for survivors.
In an era where the advances in medicine are rapidly transforming patient care, we owe it to our patients and healthcare providers alike to stay informed and work together. By tackling each of the nerve-racking and overwhelming moments with practical, well-informed strategies, the future of breast cancer care remains as hopeful as it is resilient.
Originally Post From https://www.oncnursingnews.com/view/managing-acute-and-late-adverse-effects-of-breast-cancer-radiation
Read more about this topic at
Radiation therapy‐associated toxicity: Etiology, management …
Radiotherapy toxicities: mechanisms, management, and …