Exploring the Ties Between Diabetes, Obesity and Cancer: A Modern Perspective
In today’s rapidly evolving field of healthcare, the links between diabetes, obesity, and cancer have become a central topic of discussion among researchers, clinicians, and patients alike. With overweight now recognized as the leading modifiable factor—aside from smoking—that can contribute to cancer risk, it is essential to take a closer look at how our own metabolism can both protect and endanger us. Recent studies from City of Hope have shed light on the tangled issues between these conditions, emphasizing that a deeper understanding of metabolic dysfunction can pave the way for innovative treatments and better patient outcomes.
This opinion piece takes a comprehensive look at the current research findings, the roles of genetic predispositions, and the therapeutic potential these insights harbor. Here, we will examine the tricky parts of the relationship between metabolic dysfunction and cancer, explore the little details that reveal subtle but crucial connections, and offer a neutral perspective on where healthcare might be headed in light of these discoveries.
A Closer Look at Diabetes, Obesity and Cancer Interrelations
Over the past few decades, the landscape of oncologic and metabolic research has shifted dramatically. With an alarming increase in global rates of overweight and diabetes, more and more individuals are facing the possibility of multiple organ site cancers linked to these metabolic conditions. Researchers at City of Hope are working through the tangled issues that connect metabolic dysfunction with cancer development and progression. Their interdisciplinary work, integrating clinical studies, population data, and basic science research, has opened new windows into understanding how conditions like type 2 diabetes (T2D) and obesity might serve as catalysts for cancer.
It is important to note that the robust research agenda at City of Hope is not restricted to mere incidences of disease; instead, the focus is on the fine points of how metabolic imbalances actually drive cancer biology. By taking a closer look at the complicated pieces of our genetic heritage and their roles in energy storage and metabolism, scientists are uncovering key aspects that were once hidden away in the nitty-gritty of our genetic code.
Genetic Heritage and Metabolic Mismatch: Storing More Than Energy
One fascinating aspect highlighted by recent research is how our genes—developed over millennia to help our ancestors survive periods of famine—are now, in the age of abundance, contributing to a cascade of metabolic problems. The hepatocytes in our liver, evolved to store excess energy as fat, are now often overloaded with lipids, creating an environment ripe for metabolic dysfunction. This mismatch between the genes we inherited and the current conditions we live in is one of the core reasons for the development of metabolic dysfunction-associated steatotic liver disease (MASLD), a condition previously known as fatty liver disease.
The evolutionarily conserved pathways that originally protected us now have the opposite effect, frequently leading to hepatic insulin resistance, fibrotic liver dysfunction, and even an increased risk of cancer. This discovery sets the stage for a broader discussion about how genetic predisposition and environmental pressures can converge, steering our bodies toward conditions that are both intimidating and overwhelming to patients.
Unearthing Hidden Connections: MASLD and Its Wider Implications
MASLD affects more than a billion people around the globe. Despite its widespread presence, many individuals remain unaware of their condition until it has progressed to more severe states such as diabetes or hepatocellular carcinoma (HCC). This lack of early diagnosis demonstrates one of the tricky parts of modern healthcare: the subtle details that can easily be overlooked until severe complications arise.
While MASLD is often associated with those who are overweight, a significant number of lean individuals are also affected. This phenomenon, often puzzling to clinicians and researchers, suggests that underlying energy storage problems may not always align with visible weight issues. In such cases, understanding the fine shades of metabolic imbalance becomes a super important task. Research is now focusing on the different manifestations of MASLD, aiming to unravel the little twists that distinguish lean MASLD from the more common forms seen in overweight individuals.
Rare Diseases Illuminate Common Conditions: The Case of Citrin Deficiency
Rare diseases often serve as potent models for understanding more common illnesses. An excellent example of this is Citrin Deficiency (CD), a rare metabolic disorder that has provided unexpected insights into liver function and fat storage. Unlike the typical MASLD patient, individuals with CD tend to be lean, yet they suffer from severe metabolic dysfunction in their livers. Their livers struggle with ATP generation, yet paradoxically, still deposit fat in the form of lipid droplets.
One particularly intriguing observation among CD patients is their general dislike for sweets. Researchers have hypothesized that this aversion may be a result of elevated levels of FGF21, a hormone produced by the liver that signals the brain to lose interest in sugary foods. Experiments using genetically modified mice have supported this idea, with findings suggesting that high FGF21 levels are connected to both increased liver fat accumulation and impaired ability to burn that fat.
The investigation into CD illustrates how diving in to examine rare conditions can yield valuable insights into more widespread problems. Despite being a rare condition, CD studies have provided clues regarding some of the subtle, mysterious aspects of liver metabolism, potentially offering new ways to treat both lean and common MASLD.
Mapping Out the Therapeutic Landscape: From Genetic Pathways to Treatment Avenues
Research at City of Hope has unlocked several therapeutic avenues that could revolutionize the treatment of MASLD, diabetes, and cancer. As researchers take a closer look at the tangled issues in energy metabolism, they are identifying drug targets that might enable the liver to release stored fat, thereby reducing the risk of progression to insulin resistance and full-blown liver dysfunction. The overall objective is to manage the liver’s energy storage and utilization better—crucial steps in managing not only MASLD but also its downstream consequences, like cancer.
There are three promising therapeutic directions that have emerged from this research:
- Mobilizing Fat from the Liver: This approach seeks to convert the liver from a fat-storing organ into one that can more efficiently burn fat, a key to mitigating both MASLD and its associated complications.
- Targeting Urea Cycle Toxicities: In patients with rare conditions such as Citrin Deficiency, managing the toxicities related to the urea cycle is a critical issue. Targeting these pathways could alleviate some of the severe metabolic disturbances seen in these patients.
- Enhancing FGF21 Production: Given the role of FGF21 in regulating sweet preference and liver fat accumulation, researchers are investigating oral drugs that can increase the body’s own production of this hormone. This strategy holds promise for managing MASLD, reducing overweight, and even curbing cravings for sweets and alcohol.
Each of these approaches offers a unique angle on treating metabolic dysfunction, and illustrations in early studies highlight the potential for these therapeutic strategies to extend their benefits to a wide variety of patients. The possibility of an oral drug that could stimulate FGF21 production, for instance, is especially enticing because it might simultaneously help patients deal with weight management and reduce cancer risks.
Understanding the Tricky Parts of Metabolism Research
It is not always easy to figure a path through the maze of interconnections between metabolism, diabetes, and cancer. The research conducted at City of Hope is replete with challenges that require careful evaluation of small distinctions in genetic expression and metabolic responses. Among these are the confusing bits of how our livers respond to persistent metabolic stress and the ways in which seemingly minor gene expression changes can lead to significant health problems.
The work being done in this field is loaded with challenges. Scientists must sort out a multitude of subtle parts and little details that, taken together, form a broader picture of metabolic health. For example, the differences between fat accumulation in lean versus overweight individuals are not merely a matter of scale but involve distinct biological processes that require diverse therapeutic approaches. Understanding these fine points is a super important area of research that continues to evolve as new data emerge.
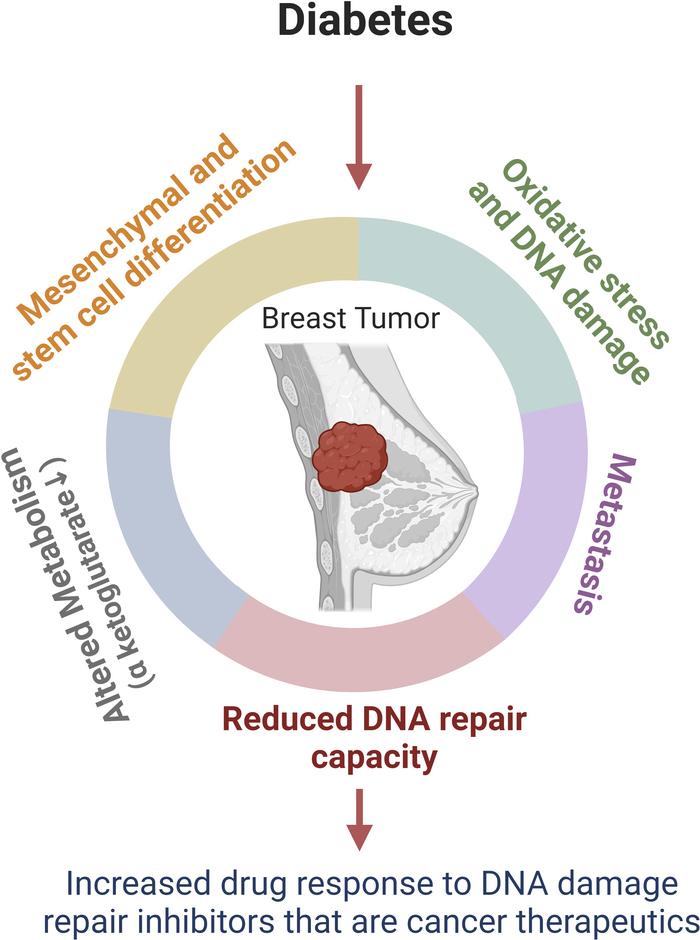
Intersecting Pathways: How Metabolism Influences Cancer Development and Progression
The interconnected nature of metabolism and cancer creates a scenario that is on edge with potential breakthroughs. Metabolic dysfunction does not only prelude diabetes and liver diseases but also appears to play a key role in cancer development. One of the challenges that researchers face is teasing out the subtle details in how altered metabolic pathways can influence cancer cell growth, survival, and resistance to treatment.
Recent findings demonstrate that the same signaling pathways that once represented a survival advantage now contribute to the aggressive behavior of cancer cells. These cells seem to reprogram their mechanisms to thrive in an environment characterized by metabolic stress. The twists and turns in these processes highlight that cancer, in many cases, should be viewed as a disease of metabolism as much as it is one of cell division and genetic mutations.
This deeper understanding of cancer’s metabolic dependencies has practical implications. By identifying points where metabolic regulation goes awry, scientists can develop targeted therapies that may disrupt the energy supplies that cancer cells rely on. Given the highly adaptive nature of cancer cells, finding these vulnerable moments, even if they occur amid a maze of tangled issues, could lead to the development of more effective and personalized treatments.
Charting the Course for Patient-Centric Benefits
While the science behind these discoveries is complex, the ultimate goal remains simple: to transform our understanding of metabolic dysfunction into tangible benefits for patients. This includes not only improving treatment outcomes but also developing early detection strategies for metabolic disorders such as MASLD before they progress to more serious conditions like diabetes and cancer.
For patients and healthcare providers alike, managing a chronic disease that is loaded with issues can seem intimidating, nerve-racking, and at times overwhelming. However, as our understanding of the tangled issues behind metabolic dysfunction improves, so does our ability to develop interventions that are both innovative and effective. Research that ties together multiple aspects of metabolism, cancer, and genetic predispositions is slowly starting to chip away at these challenges, offering hope where there was once uncertainty.
Key Takeaways in the Fight Against Metabolic Disorder-Related Cancers
To crystallize the discussion, consider the following table summarizing the core elements and targeted strategies emerging from recent research:
| Aspect of Metabolic Dysfunction | Description | Potential Therapeutic Strategy |
|---|---|---|
| Liver Fat Accumulation | Excess energy storage due to evolutionary gene pathways | Drug targets to mobilize liver fat for improved metabolic function |
| Urea Cycle Toxicities | Particularly prominent in rare conditions like Citrin Deficiency | Interventions that alleviate toxicities and restore metabolic balance |
| FGF21 Regulation | High levels correlate with sweet aversion and liver fat build-up | Oral drugs to enhance natural FGF21 production and reduce cravings |
| Metabolic Reprogramming in Cancer | Cancer cells adapt to metabolic stress by altering energy pathways | Targeted therapies to disrupt cancer cell energy supply |
This table distills the fine points of the evolving research landscape, highlighting potential areas where patient care can be significantly improved. Each approach represents a piece of the broader picture, emphasizing that the pathways fueling our metabolic processes can also be harnessed for therapeutic benefit.
Future Horizons: Integrating Research Into Clinical Practice
As these discoveries continue to emerge from City of Hope and similar research institutions, the importance of integrating these insights into clinical practice becomes increasingly clear. The challenging bits of metabolic dysfunction research—the subtle details of gene expression, the hidden complexities of fat storage, and the intricate relationship between chronic diseases—must all be translated into diagnostic and treatment protocols that benefit patients at every stage of their disease journey.
There is a growing consensus among healthcare experts that a more holistic approach, which takes into account the intertwined nature of diabetes, obesity, and cancer, is essential. By piecing together the different aspects of metabolic health and disease risk, clinicians can begin to figure a path that not only treats the immediate symptoms but also addresses the root causes of these interconnected conditions.
Future clinical trials and public health initiatives need to adopt a multi-disciplinary perspective. This involves:
- Collaboration between oncologists, endocrinologists, and nutritionists.
- Enhanced screening protocols for early detection of MASLD.
- Patient education programs that focus on lifestyle modifications and dietary changes aimed at mitigating metabolic risk factors.
- The incorporation of personalized medicine where genetic markers guide the choice of therapy and lifestyle interventions.
As these strategies are refined and implemented, the hope is that patients will experience a significant reduction in the progression of metabolic disorders to chronic conditions like diabetes and cancer. The delicate balance of metabolism, once seen as a source of overwhelming complications, may soon be managed in ways that directly target the core issues leading to disease.
Integrative Health Approaches: Beyond Conventional Medicine
In addition to traditional approaches, alternative medicine and nutrition have an essential role to play in managing metabolic dysfunction. The modern lifestyle, characterized by high-calorie diets and sedentary behaviors, has led many to grapple with energy imbalances that neither medicine nor surgery alone can fix.
Diet and lifestyle modifications, when combined with the latest research on metabolic pathways, offer a practical approach to addressing the subtle parts of these conditions. For example, nutritional plans focused on reducing sugar intake, managing insulin sensitivity, and optimizing micronutrient levels can help to counteract the internal processes that lead to MASLD and related disorders.
Alternative therapies such as acupuncture, mindfulness, and herbal supplements are also being explored for their potential benefits in regulating metabolism. When integrated with conventional treatments, these strategies may help patients steer through the maze of changing metabolic profiles, offering relief from some of the more tangled issues associated with chronic disease.
Patient Empowerment and the Changing Role of Healthcare Providers
One of the hallmarks of this evolving research is the empowerment of patients. With access to more information, patients today are better equipped to participate actively in decisions about their health care. As research reveals more about the connection between diabetes, obesity, and cancer, healthcare providers have a responsibility to communicate these findings in clear, practical terms.
By demystifying the little twists of metabolic dysfunction, clinicians can help patients understand the importance of early lifestyle changes and routine screenings. This isn’t just about treating a disease once it manifests; it’s about preemptively managing risk factors—a strategy that may well be the key to reducing overall disease burden in the community.
Patients are encouraged to ask questions, participate in clinical trials, and work with a multidisciplinary team that can help them figure a path tailored to their specific metabolic profile. This collaborative approach, combining modern medicine with nutritional science and even complementary therapies, represents one of the most promising directions for healthcare in the coming years.
The Road Ahead: Challenges and Optimism in Metabolic Health Research
While much progress has been made, the road ahead is loaded with challenges. Research into the metabolic underpinnings of cancer remains a field on edge, full of problems that are as intimidating as they are promising. For every discovery that guides new treatment options, there are a host of complicated pieces that researchers continue to unravel.
Nonetheless, the momentum generated by recent studies offers a sense of cautious optimism. The insights gained from examining fine shades of metabolic regulation have already begun to influence clinical protocols and public health initiatives. With continued investment in research that digs into the tangled issues of metabolic health, the next decade may bring therapies that not only treat cancer and diabetes but also prevent them from developing in the first place.
The future of healthcare in this area will likely depend on maintaining a multidisciplinary dialogue among various scientific disciplines. The work at City of Hope serves as a prime example of how combining genetic insights with clinical observations and nutritional research can lead to breakthroughs that benefit patients across the board.
Conclusion: Transforming Insights into Tangible Health Advances
In conclusion, the evolving research linking diabetes, obesity, and cancer highlights the significant impact metabolic dysfunction has on our overall health. It is a field characterized by tangled issues, tricky parts, and hidden complexities that call for patience, perseverance, and innovative thinking. By taking a closer look at our genetic heritage and the little complexities of liver metabolism, researchers are gradually demystifying the processes that underpin these serious conditions.
The transformative work at City of Hope is a reminder that modern medicine is an ever-evolving landscape. With a commitment to understanding the fine details of energy metabolism and its influence on diseases like cancer, we are beginning to see new therapeutic targets that could one day revolutionize patient care. Through multidisciplinary collaboration, patient empowerment, and a willingness to integrate alternative approaches with conventional medicine, the future of treating these interconnected conditions looks promising.
Though the twists and turns in this research may seem overwhelming at times, every discovery brings us one step closer to treatments that not only ease the burden of disease but also improve the quality of life for millions of patients worldwide. The key now is to continue to figure a path through these complicated pieces—a task that requires both scientific rigor and a compassionate, patient-centered approach to healthcare.
As we stand at the crossroads of metabolic research and clinical innovation, the lessons learned from studies on MASLD, Citrin Deficiency, and FGF21 regulation serve to remind us that even the most tangled issues can eventually lead to clear, practical solutions. By embracing these insights and working collaboratively, the medical community can forge a new era where the combined forces of modern medicine, alternative strategies, and nutritional science hold the promise of a healthier future for all.
Originally Post From https://cancerletter.com/sponsored-article/20250711_5/
Read more about this topic at
the role of salivary amylase activity in modulating visceral …
the role of salivary amylase activity in modulating visceral fat …