Illuminating New Frontiers in Cervical Cancer Therapy
Recent research is shining a light on a trailblazing treatment approach that combines photodynamic therapy (PDT) with the chemotherapeutic agent oxaliplatin to tackle cervical cancer. In this opinion editorial, we take a closer look at this cutting‐edge modality, exploring how merging light-activated treatment methods with conventionally used chemotherapy can potentially transform the way we treat this challenging disease.
Cervical cancer has long represented a significant global health challenge, partly due to its aggressive progression and stubborn resistance to many conventional therapies. The novel integration of PDT and oxaliplatin has sparked interest among oncologists and researchers alike, as it seems to offer a more precise and targeted means to eradicate cancer cells. This innovative approach could prove a game changer not only for cervical cancer patients but also for those diagnosed with other malignancies where cancer stem cells are at work.
Pioneering the Use of Photodynamic Therapy in Modern Oncology
Photodynamic therapy relies on the use of photosensitizing agents that become activated when exposed to specific wavelengths of light. Once activated, these compounds generate reactive oxygen species that can kill cancer cells with pinpoint precision. Unlike standard chemotherapy, PDT offers spatial control and is able to steer through the tricky parts of treatment by limiting damage to surrounding healthy tissue.
The marriage of PDT with chemotherapy, like oxaliplatin, brings new possibilities to the table. PDT can specifically attack tumor cells, reducing the risk of systemic side effects, while oxaliplatin contributes its well-documented anti-tumor activity. Together, they enhance the anti-proliferative activity against cervical cancer cells. Researchers report that when PDT is applied alongside oxaliplatin, there is a marked increase in cell death via synergistic activation of apoptotic pathways.
Clinical Implications of Targeted Photomedicine in Cervical Cancer
The clinical implications of this combined therapy are profound. Cervical cancer often comes with a host of complicated pieces including rapid progression, early metastasis, and resistance to treatment. Traditional chemotherapies sometimes fall short in addressing the fine points related to cancer stem cells—those hidden complexities that allow tumors to regenerate and survive even after treatment.
By incorporating PDT, clinicians have the opportunity to better manage treatment by directly targeting these cancer stem cells. Research shows that combined therapy results in significant downregulation of key stemness markers, such as SOX2, NANOG, and OCT4, which are critical for the self-renewal and persistence of cancer cells. This suppression of stemness factors is a super important step in reducing the risk of cancer relapse, potentially offering patients a brighter prognosis.
Synergy Between Oxaliplatin and Photodynamic Therapy
The duo of oxaliplatin and photodynamic therapy is generating considerable excitement based on its potential to overcome some of the nerve-racking challenges posed by cervical cancer. Oxaliplatin, a platinum-based drug known for its effectiveness in various solid tumors, has had limited success when used alone against cervical cancer. However, when the tedious process of standalone chemotherapy is combined with the precise action of PDT, a new therapeutic synergy emerges.
This synergy is attributed to the different yet complementary modes of action. Oxaliplatin primarily functions by inducing DNA damage, leading to cell death. The additional oxidative stress generated by the light-activated PDT further propels cancer cells toward apoptosis. In effect, the combination can tackle both the proliferative mass of the tumor and its underlying stem cells. Here is a summary of how each component contributes to the overall efficacy:
- Oxaliplatin: Causes DNA cross-linking and damage, triggering apoptosis in cancer cells.
- Photodynamic Therapy: Activates photosensitizers that produce reactive oxygen species, leading to localized cell destruction.
- Combined Action: Enhances cytotoxicity by simultaneously attacking broad tumor cells and reducing cancer stem cell survival.
This combined strategy not only augments the anti-tumor efficacy but also holds promise in reducing the overwhelming side effects typically associated with platinum-based chemotherapy. The precision of PDT may allow clinicians to lower the doses of chemotherapeutic agents needed, thereby preserving the quality of life for patients during treatment.
Dissecting the Molecular Landscape: Stemness-Related Genes in Focus
At the heart of the PDT-oxaliplatin synergy lies the regulation of stemness-related genes. These genes, including SOX2, NANOG, and OCT4, are the little details that govern the survival and propagation of cancer stem cells. These subtle parts of genetic regulation are among the primary causes of treatment resistance and cancer recurrence.
In recent studies, significant downregulation of these markers was observed with combined treatment, hinting at a promising mechanism by which the therapy disrupts the cancer’s regenerative potential. When these key genes are suppressed, the cancer stem cells lose their ability to self-renew and generate new tumor cells, effectively reducing the likelihood of metastasis and relapse.
For many oncologists, understanding these subtle genetic twists is critical because they hold the key to long-term remission. The table below outlines some of the important contrasts between the traditional treatment approach and the new combined therapy:
| Aspect | Conventional Chemotherapy | Combined PDT & Oxaliplatin |
|---|---|---|
| Cancer Cell Targeting | Broad but can affect healthy cells | Precise localized targeting with reduced collateral damage |
| Stemness Gene Modulation | Limited effect on cancer stem cells | Significant downregulation of SOX2, NANOG, OCT4 |
| Systemic Toxicity | High, often leading to severe side effects | Lower due to spatial control of PDT |
| Overall Efficacy | Variable, with resistance often emerging | Enhanced cell death, offering greater tumor control |
This table highlights how combining two different yet synergistic modalities can help overcome the scattered issues that have long puzzled clinicians treating cervical cancer.
Managing Your Way Through Treatment Side Effects
One of the major concerns with conventional chemotherapy is its overwhelming side effect profile. Patients often experience nerve-racking systemic toxicities that significantly impact their quality of life. With the introduction of PDT in combination therapy, there is a growing optimism that these adverse effects may become more manageable.
PDT’s ability to confine its action to targeted tumor cells means that off-target damage is minimized. This selective approach allows patients to potentially experience fewer and less severe side effects compared to traditional chemotherapy alone. In practical terms, it means:
- Lower systemic toxicity due to localized treatment effects.
- Potential for lower dosages of chemotherapeutic agents.
- Improved overall patient comfort and adherence to treatment protocols.
For patients and caregivers alike, this is an immensely encouraging development. The strategic combination not only fights the disease more effectively but also tackles the nerve-racking challenge of managing treatment-related complications.
Reducing the Risk of Cancer Recurrence: Long-Term Benefits
Reducing the likelihood of cancer recurrence is a must-have goal for any therapy. Cervical cancer, like many other malignancies, tends to return because of its ability to preserve a small population of resilient cancer stem cells. The combined PDT and oxaliplatin approach holds promise in tackling this particularly pesky issue.
Clinical studies have indicated that the dual treatment significantly compromises the regenerative potential of these cancer stem cells by suppressing their key genetic drivers. The long-term benefits of this strategy could include:
- A lower incidence of metastasis.
- Increased disease-free survival rates.
- A more sustained remission period.
- Overall improved life expectancy.
By chipping away at the root of cancer’s persistence, this therapy offers a more durable solution than many existing treatments. It represents a shift from solely destroying the visible tumor mass to also eradicating the hidden cells that keep cancer alive, protecting patients from the constant fear of relapse.
Overcoming the Overwhelming Challenges of Treatment Resistance
Combating treatment resistance is one of the most intimidating issues in oncological medicine. The twists and turns of cervical cancer, particularly its ability to defy conventional drugs, have always kept oncologists on high alert. However, by combining PDT with oxaliplatin, there’s hope to outsmart the disease’s many defenses.
The combined approach works by addressing both the proliferating tumor cells and the dormant, drug-resistant stem cells within the tumor. As a result, the dynamics of the cancer’s survival pathways are altered, making it more vulnerable to treatment. Here are some of the key benefits of this multi-pronged attack:
- Multi-layered Action: The dual therapy tackles cancer on several fronts, reducing the probability that resistant clones will emerge.
- Enhanced Apoptosis: The simultaneous induction of DNA damage and oxidative stress forces cancer cells into a state of programmed cell death.
- Interrupting Cancer Stem Cell Function: Downregulation of stemness markers helps deprive the tumor of its regenerative capabilities.
These benefits illustrate how understanding and targeting the tricky parts of cancer biology might finally allow us to figure a path around longstanding obstacles in cancer treatment.
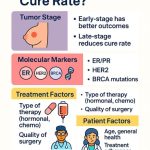
Personalizing Cancer Therapy: Tailoring Treatment Based on Molecular Profiles
Personalized medicine has been gaining ground in recent years, and the combination of PDT with oxaliplatin is a shining example of this trend. As researchers probe deeper into the molecular landscape of cervical cancer, they are beginning to identify subtle details that can be used to tailor treatments to individual patients.
By examining the expression levels of stemness genes such as SOX2, NANOG, and OCT4, clinicians can better predict how a patient’s tumor might respond to combined therapy. Such a customized approach is especially critical in a field where one size rarely fits all.
Key steps in personalizing treatment include:
- Molecular Profiling: Testing patient samples to assess the expression of genes linked with cancer stem cell properties.
- Risk Stratification: Determining which patients are more likely to benefit from a combined regimen based on their genetic profile.
- Dosage Adjustment: Modifying treatment protocols to achieve maximal efficacy while minimizing potential side effects.
This emerging framework not only improves the chances of successful treatment but also contributes to a safer and more personalized form of care, converting what was once an overwhelming challenge into a well-managed process.
Looking Ahead: Future Prospects and Research Directions
Despite the promising advances, the combined PDT and oxaliplatin therapy is still on its way through research phases and early clinical trials. As with any new medical strategy, there are many tangled issues and fine points yet to be fully understood. However, early results are very encouraging and have set the stage for further exploration.
Future research directions will likely include:
- Optimizing Treatment Protocols: Determining the most effective dosing schedules for both PDT and oxaliplatin to maximize therapeutic synergy.
- Expanding Treatment Applications: Evaluating whether similar approaches can be expanded to other types of cancer, including those of the breast, colon, and lung.
- Advanced Imaging and Monitoring: Integrating real-time imaging to better track the response of tumors to PDT, ensuring that the treatment precisely targets cancer cells and minimizes damage to nearby healthy tissue.
- Exploring Combined Modalities: Investigating how other chemotherapeutic agents might work in tandem with PDT to offer even more potent combinations.
Researchers are also focused on understanding the hidden complexities of the tumor microenvironment and how it influences treatment outcomes. By getting into these subtle details, scientists hope to design therapies that effectively overcome resistance while preserving healthy tissues.
Practical Considerations for Clinicians and Patients
Implementing this innovative treatment in everyday clinical practice involves figuring a path through a number of practical challenges. Healthcare providers must balance cutting-edge research with real-life treatment constraints, such as patient comfort, resource availability, and the risk of side effects.
For clinicians, some immediate steps to consider include:
- Training and Equipment: Ensuring that medical facilities are equipped with the necessary light sources and photosensitizers required for PDT.
- Patient Selection: Using molecular profiling to choose the patients most likely to benefit from combined therapy.
- Interdisciplinary Collaboration: Encouraging oncologists, radiologists, and surgeons to work together to craft individualized treatment plans.
- Monitoring and Follow-Up: Establishing monitoring protocols to assess patient response and adjust treatment as needed.
Patients, in turn, should be informed about the potential benefits and limitations of this treatment. Open discussion about possible side effects, the rationale behind combination therapy, and expected outcomes is essential to build trust and ensure adherence.
Concluding Thoughts: A Step Toward a More Effective, Less Toxic Future
The integration of photodynamic therapy with oxaliplatin represents a bold stride forward in the fight against cervical cancer. By targeting both the proliferative mass and the underlying cancer stem cells, this combined therapeutic approach offers substantial promise for reducing recurrence rates and improving overall patient outcomes.
While some parts of this new treatment paradigm involve navigating tricky bits and tangled issues that are still on the research horizon, the potential benefits are too significant to overlook. In the coming years, as further clinical trials clarify dosing schedules, risk factors, and long-term outcomes, it is hoped that this synergistic approach will become an essential tool in the oncologist’s arsenal.
It is important to recognize that progress in medical science is often gradual, with each breakthrough building on the last. The fusion of PDT and oxaliplatin is a testament to the power of interdisciplinary research and innovative thinking. As researchers continue to unearth more about the hidden genetic components that contribute to tumor survival, treatment strategies can be honed to target these fine shades of resistance.
The promise of a more targeted, less toxic cancer treatment is a beacon of hope for patients around the world. This combination therapeutic strategy is proof that by taking a closer look at the subtle details and embracing modern technological advances, we can make meaningful progress in areas that were once considered overwhelming.
In summary, the dual approach of using photodynamic therapy alongside oxaliplatin not only boosts anti-proliferative activity in cervical cancer cells but also fundamentally challenges the conventional methods by disrupting the very foundations of cancer stem cell survival. While additional studies will be needed to confirm these effects in larger clinical settings, the current findings offer a promising route to better treatment outcomes with reduced side effects.
For healthcare providers, researchers, and patients alike, this innovative therapy serves as a reminder that overcoming the nerve-racking challenges of cancer treatment is possible. By steering through the maze of molecular genetics, fine points of cellular resistance, and the tricky parts of clinical implementation, we are taking significant steps toward a future where cancer is not only treated more effectively but also approached with less fear and more optimism.
As we look ahead, it becomes clear that the future of oncology will likely be marked by multi-modal therapies that balance the strengths of several treatment methods. With each new discovery, the prospect of transforming cancer care from a nerve-racking ordeal into a manageable—and perhaps even conquerable—challenge becomes ever more real.
The journey is ongoing, and while there remain many puzzling bits and confusing pieces to sort out, the progress made thus far demonstrates that innovative scientific collaborations can lead to breakthrough treatments that truly revolutionize patient care. The convergence of photodynamic therapy and oxaliplatin is not just a new combination; it symbolizes our unwavering commitment to finding smarter, safer, and more effective ways to combat cervical cancer and, potentially, other stubborn malignancies.
In this rapidly evolving field, staying informed and involved is essential. As more clinical results emerge, both healthcare professionals and patients will benefit from the insights gained, ultimately enabling a smoother transition toward therapies that embrace personalized medicine, reduced collateral damage, and a brighter future for cancer treatment.
In conclusion, the integration of PDT with oxaliplatin is a promising development that addresses several of the overt challenges in cervical cancer therapy. It provides a fresh perspective on combating treatment resistance, reducing adverse effects, and personalizing care based on molecular insights. While further research is essential to fully understand all the subtle details and potential long-term benefits, the evidence to date suggests that this combined modality could soon become an essential cornerstone in the modern management of cervical cancer.
Looking forward, we can only hope that continued interdisciplinary research and clinical trials will help us fine-tune this strategy, ensuring that patients receive the most effective and least intimidating treatment possible. Amid the ever-changing landscape of oncology, breakthroughs such as these reassure us that today’s innovative approaches will lay the groundwork for tomorrow’s standard of care.
Originally Post From https://bioengineer.org/photodynamic-therapy-enhances-oxaliplatin-against-cervical-cancer/
Read more about this topic at
New Light-Based Therapy Kills 92% of Skin Cancer Cells …
Team Creates Light-Activated Therapy To Target Hard-To …