Innovative Cell Engineering Treatments: A New Era in Cancer Management
The advent of CAR-T therapy has marked a revolutionary shift in cancer treatment—a true breakthrough where modern medicine meets personalized gene therapy. As an evolving technique rooted in over three decades of research, CAR-T (chimeric antigen receptor T-cell) therapy now offers patients a chance to leverage their immune system to identify and wipe out cancer cells. In my view, this innovation is not just a technical feat but a major turning point for individuals burdened by blood cancers, such as leukemia, lymphoma, and myeloma. The approach is proving to be indispensable in offering hope to those who have seen little benefit from conventional treatments.
What makes this method so unique is its ability to repurpose a patient’s own T-cells. These white blood cells are genetically reprogrammed to recognize and attack cancer, acting like specially trained soldiers in a precision-guided mission. The entire process—starting from extraction and cell engineering to reinfusion—is both intricate and fascinating, although the state-of-the-art science behind it can sometimes seem intimidating. However, when the benefits are weighed against the risks, it becomes clear that this therapy is a game changer in modern oncology.
CAR-T therapy, once the subject of science fiction, has now transitioned into reality with FDA approval for several types of blood cancers. As an advocate for advanced therapies, I see this treatment as a beacon of progress, ushering in a new era where gene and immune therapies dovetail to create powerful, personalized treatment plans for cancer patients.
Unpacking the Process: How CAR-T Therapy Works
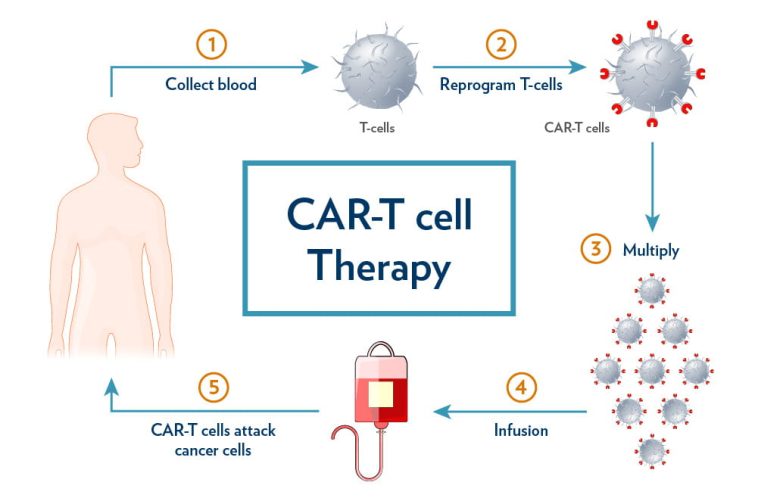
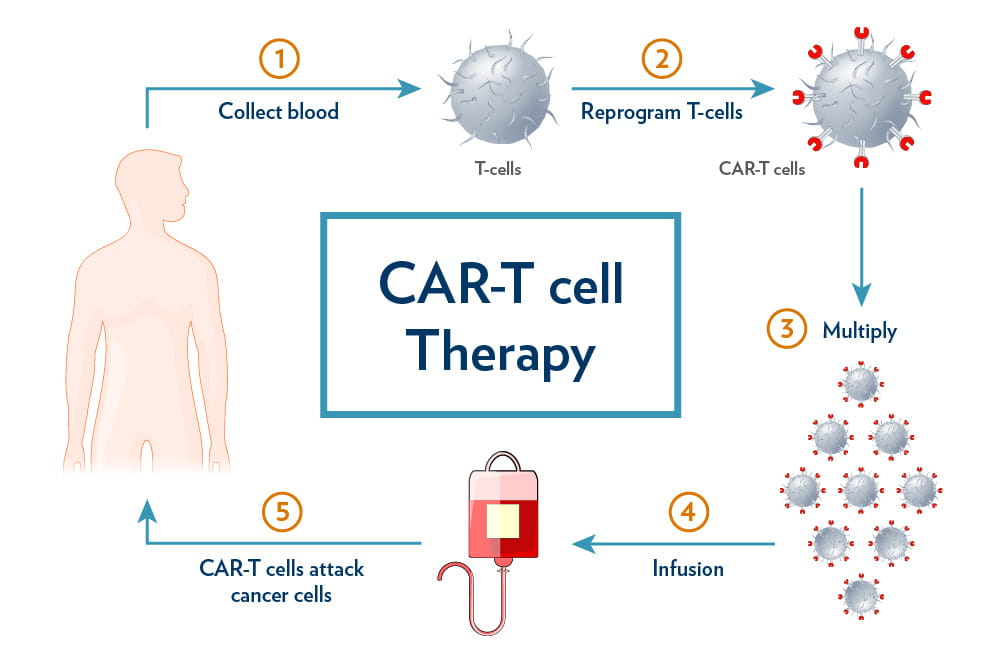
The process of CAR-T cell therapy might sound daunting at first glance, but if we take a closer look, the steps are straightforward—even if the science behind them involves some tricky parts. In essence, the journey of CAR-T therapy includes three major stages: cell collection, cellular engineering, and reinfusion. Each of these stages involves several moving pieces that must work in harmony.
Step 1: Collecting the Cells
The first step involves extracting T-cells from a patient through a specialized blood collection technique called apheresis. In this process, blood is drawn from the patient and then passed through a machine that isolates T-cells, returning the rest of the blood back into the body. Think of it as picking out the elite warriors from an army—the best suited to fight off a formidable enemy like cancer.
Step 2: Engineering the Cells
Once the patient’s T-cells are isolated, they are taken to a laboratory where scientists reengineer them. During this phase, a specially designed molecule—commonly known as a “CAR” or chimeric antigen receptor—is introduced to the T-cells. This molecule functions like a tracking system, guiding the reengineered cells to recognize and latch onto cancer cells with remarkable precision. In effect, what was once a generic immune cell is now a targeted offense unit with a specific, personalized mission against cancer.
Step 3: Returning the Cells
The final stage involves the reinfusion of these fighter cells back into the patient’s body. After a short course of chemotherapy designed to prepare the body and reduce the number of competing cells, the modified T-cells are slowly infused into the bloodstream. Typically, the entire process—from T-cell collection to their reintroduction to the body—takes roughly four to six weeks, with the infusion itself being a brief, one-time procedure that lasts only about 30 minutes.
The science behind these stages may involve some tangled issues and confusing bits in the background, but the outcome is straightforward: patients receive a tailor-made treatment that activates their immune systems to fight cancer more effectively than traditional methods. This personalized approach underlines the impressive potential of CAR-T therapy in modern medicine.
Personalized Gene Therapy for Blood Cancer: Transforming the Patient Experience
One of the most compelling aspects of CAR-T therapy is its personalization. Unlike standard treatments that use a one-size-fits-all approach, CAR-T is a customized treatment plan that treats each patient as a unique individual. By using a patient’s own cells, there is a significantly lower risk of rejection and adverse reactions—the therapy essentially works with the body’s inherent defenses.
This form of personalized gene therapy is revolutionary not only because it tailors treatment to the individual but also because it has the potential to achieve high remission rates. In some cases, a single infusion of CAR-T therapy has been known to induce lasting remissions, and even cures, in patients who previously had limited treatment options. The ability of these engineered cells to remain active in the body for extended periods offers ongoing protection against recurrences, ensuring that the immune system is always on standby to combat any returning cancer cells.
For patients who have seen multiple rounds of chemotherapy or have undergone bone marrow transplants without success, the prospect of CAR-T therapy is a welcome alternative. It brings renewed hope and a tangible option to those who have felt that traditional treatments were either too harsh or simply ineffective. The shift towards personalized, gene-based treatments signifies a deeper understanding of cancer at the molecular level—a perspective that opens new avenues for future research and more focused treatment strategies.
Benefits of CAR-T Therapy: High Remission Rates and Lasting Protection
One of the key advantages of CAR-T cell therapy is its potential to achieve high remission rates, even after a single treatment session. As more patients experience positive results, the cancer care community is beginning to embrace this innovative therapy as a pivotal tool in the battle against blood cancers.
Let’s break down some of the top benefits:
- Tailored Treatment: By using the patient’s own cells, the therapy minimizes the risk of immune rejection and adverse side effects.
- High Remission Potential: Studies show that many patients achieve full remission, in some cases obtaining long-term results that persist well after the initial treatment.
- Ongoing Immune Surveillance: The reengineered cells can remain in the body for months or even years, offering continuous protection and reducing the odds of cancer returning.
- Reduced Recurrence Risk: With active immune cells patrolling the body, there is a lower likelihood of dormant cancer cells reigniting the disease.
Each of these benefits is critical for patients who often face overwhelming treatment decisions amid a myriad of complicated pieces. The ability of CAR-T therapy to offer such potent, customized treatment makes it a cornerstone in the ongoing battle against blood cancers.
Coping with Side Effects: Understanding and Managing Treatment Risks
Despite the many benefits, it is important to be aware that CAR-T therapy is not without its risks. As with any powerful treatment, the aggressive nature of harnessing the immune system can inadvertently trigger some unintended consequences. Two of the most common concerns are Cytokine Release Syndrome (CRS) and neurotoxicity.
Recognizing Cytokine Release Syndrome (CRS)
CRS occurs when the immune system responds in an overly aggressive manner, releasing a flood of signaling proteins called cytokines. This can lead to symptoms such as high fevers, low blood pressure, and difficulty breathing. For some patients, these symptoms can escalate, affecting the nervous system and manifesting as confusion, memory impairment, or even seizures.
To counter these reactions, medical teams closely monitor patients after the infusion. Typically, patients remain in the hospital or nearby facility for 30 days after treatment. During this period, any early signs of CRS can be promptly addressed using targeted treatments and supportive care measures.
Dealing with Neurotoxicity
Neurotoxicity is another significant risk, with symptoms that may include difficulties with speech, motor function, and general cognitive abilities. Like CRS, these complications can be particularly threatening if not managed early and effectively. However, many cases of neurotoxicity have proven to be reversible when detected quickly, stressing the importance of vigilant post-therapy monitoring by knowledgeable specialists.
The management of these side effects involves a combination of close observation, supportive measures, and sometimes additional medications. The goal is to ensure that, while patients do face some scary or nerve-racking challenges, they are well supported every step of the way. Overall, the consensus in the medical community is that the benefits of CAR-T therapy outweigh these risks, provided that the treatment is administered by experts who are well-versed in these tricky parts of the process.
Insurance Coverage and Financial Planning for Advanced Cancer Treatments
Another important factor for patients considering CAR-T therapy is the cost involved. Advanced treatments like these can appear intimidating from a financial standpoint. However, there is encouraging news: most commercial insurance plans, along with government programs such as Medicare and Medicaid, typically cover CAR-T therapy when it is prescribed for approved indications.
Financial planning is an essential aspect of managing any serious health condition. To assist with the costs, many patients may have access to additional financial aid programs offered by product manufacturers, non-profit foundations, and other support networks. These resources are designed to help ease the financial burden so that the focus can remain on healing.
| Insurance Type | Coverage Scope | Additional Support |
|---|---|---|
| Commercial Insurance | Approved for several blood cancers | Supplemental programs sometimes available |
| Medicare | Coverage for FDA-approved indications | Potential for further financial assistance |
| Medicaid | Generally covers approved CAR-T procedures | Nonprofit and manufacturer support programs |
For those planning financially, it might be useful to consult with financial advisors or hospital billing specialists who can help clarify coverage details and benefit options. The existence of support programs is a super important aspect that can ease the pressure on patients and their families during what is already an overwhelming time.
Real-World Experiences: Patient Perspectives on CAR-T Therapy
Though the technical advantages of CAR-T therapy are compelling, the human side of the story is equally powerful. Patients who have previously struggled with the heavy burdens of traditional cancer treatments report feelings of renewed hope and improved quality of life after undergoing CAR-T therapy. Their personal stories highlight the transformative potential of personalized, gene-based treatments.
For many survivors, the journey through CAR-T is one marked by moments of both anxiety and relief. Initially, the idea of genetically modifying one’s own cells may seem off-putting or tense. However, over time, the benefits become apparent: reduced reliance on multiple rounds of chemotherapy, fewer overall side effects, and in many cases, a redefined outlook on life. This therapy is not just a medical procedure; it is a lifeline that transforms the treatment experience into one where patients feel actively engaged in fighting back against the disease.
Patient testimonials underscore two crucial points: the success of CAR-T therapy in achieving remission and the renewed confidence patients gain knowing that their immune system is now their ally. While not every case is without complications, the overall improvement in patients’ quality of life reaffirms my belief in the importance of continued research and refinement in this field.
Expert Opinions: The Medical Community’s Take on CAR-T Therapy
Insights from oncologists and hematologists have been overwhelmingly positive about CAR-T therapy’s potential. Medical experts appreciate that this therapy harnesses the body’s own resources in a way that traditional treatments often cannot. In discussions with peers and specialists, I have come to understand that CAR-T therapy represents both a scientific marvel and a practical solution to the tricky parts of long-standing cancer challenges.
Dr. Igor Medic, a board-certified oncologist and hematologist, is just one voice among many in the field who has championed the benefits of CAR-T therapy. According to him, patients who undergo this treatment often experience significant remission rates—even after a solitary infusion—due to the therapy’s ability to keep the reengineered T-cells active in the body for prolonged periods. His insights reinforce the notion that, despite the complex science behind it, CAR-T therapy’s overall impact on patient care cannot be overstated.
From an expert standpoint, the necessity for specialized training and rigorous certification for physicians administering CAR-T therapy cannot be underscored enough. Teams at renowned cancer centers undergo detailed training that covers every stage of the process, ensuring that they are well-prepared to figure a path through even the most tangled issues that may arise during treatment. This commitment to excellence is a critical factor behind the therapy’s success and safety.
Addressing the Hidden Complexities: Fine Points and Small Distinctions in CAR-T Therapy
While much of the praise for CAR-T therapy focuses on its benefits, it is important to also consider some of the subtle parts and hidden complexities that come with such advanced treatments. The procedure, while innovative, involves several layers of preparation, execution, and aftercare that are often subject to slight differences from patient to patient. These variations can sometimes make the treatment appear as if it is full of problems, but the dedicated efforts by medical teams are aimed at minimizing such issues.
Let’s consider some of these finer points:
- Patient Selection: Not every patient with blood cancer is an ideal candidate for CAR-T therapy. Factors such as overall health, disease progression, and previous treatments are carefully considered.
- Timing and Scheduling: The entire treatment process, from cell collection to infusion, requires precise timing to ensure that the T-cells remain viable and effective.
- Post-Therapy Monitoring: The period immediately following the infusion is crucial, as patients are closely observed for any signs of immune overreaction or neurotoxicity. This requires a collaborative approach between oncologists, nurses, and supportive care teams.
- Management of Side Effects: As already discussed, the risks associated with cytokine release and neurotoxicity call for proactive management strategies that are tailored to the individual. Early detection and prompt intervention are key to mitigating these risks.
By taking these aspects into account, healthcare providers can ensure that every patient receives not only a cutting-edge treatment but also comprehensive care designed to address both the promising outcomes and the challenging twists and turns of CAR-T therapy.
Future Directions: The Evolving Landscape of CAR-T Therapy and Cancer Care
Looking forward, the future of CAR-T cell therapy appears both bright and expansive. As research continues and technology improves, we can anticipate enhancements that will make these treatments even more effective and accessible. There is significant potential for CAR-T therapy to extend beyond just blood cancers and into the realm of solid tumors—a prospect that excites both researchers and clinicians alike.
One promising direction is the development of next-generation CAR-T therapies that incorporate additional modifications to enhance their specificity and reduce adverse side effects. For example, researchers are exploring ways to add multiple layers of safety switches into the engineered cells, allowing clinicians to better control the immune response and mitigate risks associated with overactivation. These advancements are a testament to the tireless efforts of the scientific community to not only expand the applications of CAR-T therapy but also fine-tune the process to address the subtle details that can make a big difference in patient outcomes.
Additionally, interdisciplinary collaborations between bioengineers, genetic scientists, and clinical researchers are paving the way for novel therapies that combine the best aspects of gene editing, immunotherapy, and personalized medicine. This integrative approach is expected to result in treatments that are more precise, with fewer complications and better overall patient experiences. The evolving landscape of cancer care is thus poised to offer more tailored and effective therapies for patients around the world.
Integrating CAR-T Therapy into Standard Cancer Treatment Protocols
As CAR-T therapy gains traction, an important discussion in cancer care is how to integrate this treatment into existing protocols. Traditional cancer treatments, such as chemotherapy, radiation, and surgical interventions, have long been the mainstays of oncology. However, these methods are not without their own set of challenging parts and nerve-racking side effects. CAR-T therapy, with its personalized and targeted approach, offers an alternative that could potentially be combined with or even replace some aspects of standard care.
The process of integrating CAR-T therapy involves several critical considerations:
- Cross-disciplinary Coordination: Successful integration requires that oncologists, hematologists, and immunologists work closely alongside surgical teams and radiologists to create comprehensive treatment plans.
- Patient-Centered Care: Since CAR-T therapy is tailored to individual patients, integrating it into treatment protocols calls for a personalized approach that takes into account each patient’s unique health history and treatment goals.
- Ongoing Research: As clinical trials continue and more data becomes available, treatment protocols will need to be continually revised to reflect the latest insights on efficacy and safety.
- Infrastructure and Training: Hospitals and cancer centers must invest in specialized training and equipment necessary for safely administering CAR-T therapy, ensuring that every step—from cell extraction to monitoring—is executed with precision.
These considerations illustrate that while the integration of CAR-T therapy into standard cancer treatment models presents its fair share of complicated pieces, the potential benefits make it a worthy pursuit. Ultimately, adopting such advanced treatments could streamline cancer care, offering patients a more hopeful and less taxing treatment journey.
Collaborative Care: The Role of the Medical Team in CAR-T Therapy
The success of CAR-T therapy does not rest solely on the shoulders of innovative science—it also depends on the coordinated efforts of a dedicated medical team. From oncologists and hematologists to nursing staff and support personnel, every member of the care team plays a super important role in ensuring that patients receive the best possible treatment and support throughout their journey.
Effective collaborative care involves:
- Comprehensive Training: Specialized certification programs ensure that each participant is familiar with the subtle parts and challenging aspects of CAR-T therapy. This training helps to figure a path through issues that might arise both during and after treatment.
- Consistent Communication: Regular and clear communication among the care team, as well as between the providers and the patient, is key to managing side effects and addressing any concerns promptly. Open dialogue builds trust and helps patients understand every step of the process.
- Coordinated Monitoring: Continuous monitoring after the infusion is critical, particularly during the first 30 days, so that any unexpected immune reactions can be immediately addressed. This collaborative approach ensures that safety is always the top priority.
- Emotional and Psychological Support: The journey through cancer treatment is often overwhelming. Providing mental health support and counseling services is essential to help patients cope with the off-putting and sometimes nerve-racking emotional challenges that arise during treatment.
This comprehensive, patient-centered approach reinforces the idea that advanced treatments like CAR-T therapy are just one part of a bigger picture—a picture that, at its core, is about giving patients the best possible chance at a healthier, more resilient life.
Balancing Hope and Caution: A Personal Reflection on CAR-T Therapy
As someone deeply invested in the field of healthcare and modern medicine, I find myself torn between boundless optimism and prudent caution when considering the potential of CAR-T therapy. On one hand, the possibility of using one’s own cells to fight cancer offers a glimpse into a future where treatments are not only more effective but also less traumatic than traditional methods. On the other hand, the detailed process and the inherent risks remind us that even the most promising treatments come with their share of tangled issues.
My personal reflection on this breakthrough is one of cautious hope. The story of CAR-T therapy is a testament to human ingenuity—a blend of cutting-edge research, rigorous training, and compassionate patient care. With each passing day, as research advances and technology becomes even more refined, the chances of optimizing this therapy improve. The potential for fewer relapses and longer periods of remission heralds a new age in cancer treatment, one where the concept of a “cure” moves ever closer to reality.
Yet, it is essential for patients, families, and even healthcare providers to fully understand both the optimistic potential and the realistic risks of this treatment modality. Being aware of the complicated pieces, the hidden complexities, and the need for ongoing support can help everyone involved find their way through the maze of advanced cancer care with informed confidence.
Conclusion: Shaping a Brighter Future in Cancer Care
CAR-T therapy stands at the crossroads of modern medicine and personalized treatment—a symbol of hope for those who have long battled aggressive blood cancers with few effective options. Its journey from a dream in the lab to a clinical reality is a narrative defined by determination, innovation, and the relentless pursuit of better care. For patients facing the overwhelming challenges of cancer, this therapy offers not just a treatment, but a chance at renewed life, free from the relentless march of conventional methods that often leave too many questions unanswered.
As the medical community continues to work through the tricky parts and manage the hidden complexities of this groundbreaking approach, one thing remains clear: CAR-T therapy is not merely a fleeting trend. It is a critical, transformative tool that will likely pave the way for even more refined therapies to emerge in the near future. Whether you are a patient, a family member, or a healthcare provider, the evolution of CAR-T therapy is a reminder that hope and innovation go hand in hand—each step forward a testament to our collective resilience in the face of one of humanity’s most challenging adversaries.
In closing, while embracing the benefits of CAR-T therapy, it is crucial to remain informed and vigilant about both its advantages and its potential risks. With continued advancements, robust safety measures, and the unwavering dedication of healthcare professionals, the promise of a future where cancer is not a life sentence but a treatable condition is firmly within reach. Let us then look forward to a next-generation era in cancer care—a future where personalized treatment is not just an option, but the standard.
Originally Post From https://eccalifornian.com/innovative-car-t-therapy-brings-new-hope-to-cancer-patients/
Read more about this topic at
Revolutionizing Cancer Treatment: Recent Advances in …
Revolutionizing Cancer Treatment: Recent Advances in …